INTRODUCTION
Strauss provided the first description of the digital block in 1889 for the condition of an ingrown toenail, using 20% cocaine at the base and under the nail. In 1905, Heinrich Braun reported the synergistic advantage of adding epinephrine to local anesthetics. However, the use of epinephrine in digital block anesthesia has been avoided due to the theoretical risk of ischemia and possible gangrene. However, Bradon Wilhelmi and colleagues demonstrated the safety and efficacy of epinephrine-containing local anesthetic for digital block.
Digital block is one of the most common nerve block techniques. It is frequently used in the emergency department and primary care settings for various procedures such as lacerations of the finger or toe, nail removal, nail bed repair, paronychia drainage, removal of foreign bodies, and any other painful procedures on digits.
In 1990, almost a century after the first publication regarding traditional digital block, David Chiu described a technique of digital block that produced complete finger anesthesia with a single injection into the flexor tendon sheath at the level of the distal palmar crease. In anatomic investigations, he showed that after injection of methylene blue into the flexor tendon sheath there was “complete staining of the entire flexor tendon sheath and centrifugal diffusion of the blue dye circumscribing the entire circumference of the proximal phalanx” (see Transthecal Digital Block).
The advantages of this technique are (1) rapid onset of action, (2) only a small volume of anesthetic solution is required, (3) only a single injection is required, and (4) absence of risk of direct trauma to the neurovascular bundles.
Although Chevaleraud and coworkers did not find anesthesia of the dorsum of the finger in all cases, some investigators consider the transthecal method to be as effective as a traditional digital nerve block. Others have found that it results in anesthesia comparable to the newer single-injection subcutaneous digital blocks, both in experimental and clinical situations.
Transthecal anesthesia appears to be safe and effective without causing any long-term damage to the tendon sheath. Several different techniques of digital block and their modifications are available: In this chapter, we describe the two that are most commonly used in our institution.
REGIONAL ANESTHESIA ANATOMY
The common digital nerves are derived from the median and ulnar nerves and divide in the distal palm into the volar aspect, tip, and nail bed area (Figure 1). The main digital nerves, accompanied by digital vessels, run on the ventrolateral aspect of the finger immediately lateral to the flexor tendon sheath (Figure 2). Small dorsal digital nerves run on the dorsolateral aspect of the finger and supply innervation to the back of the fingers as far as the proximal joint.
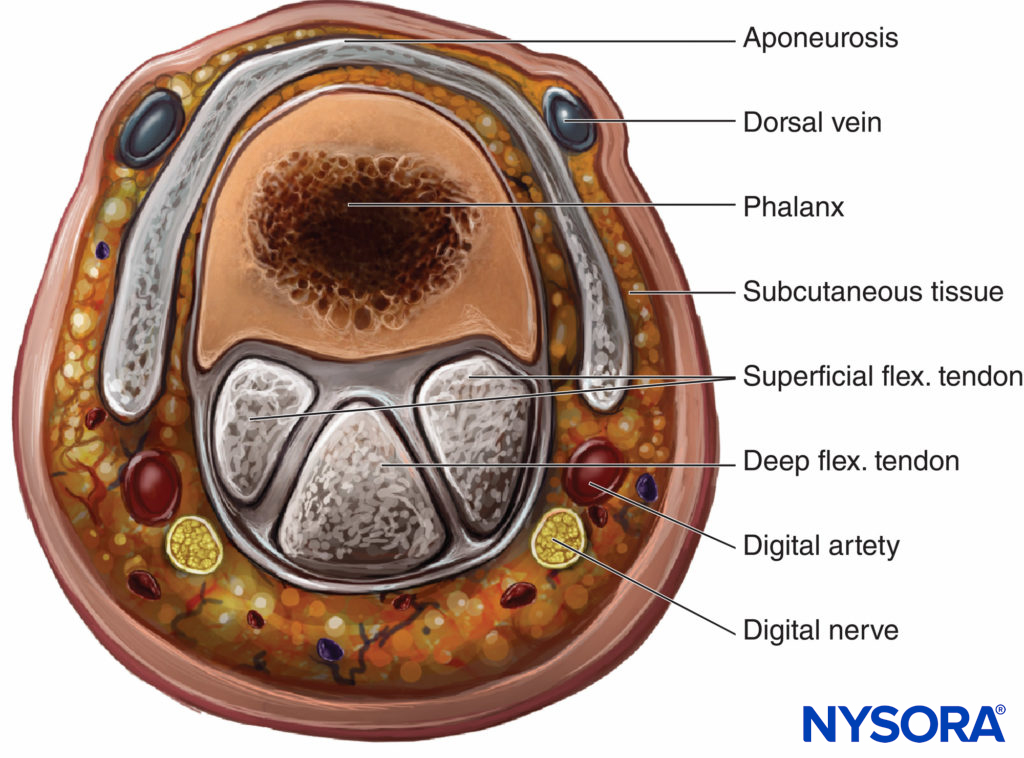
Figure 1. The origin and Distribution of the digital nerves
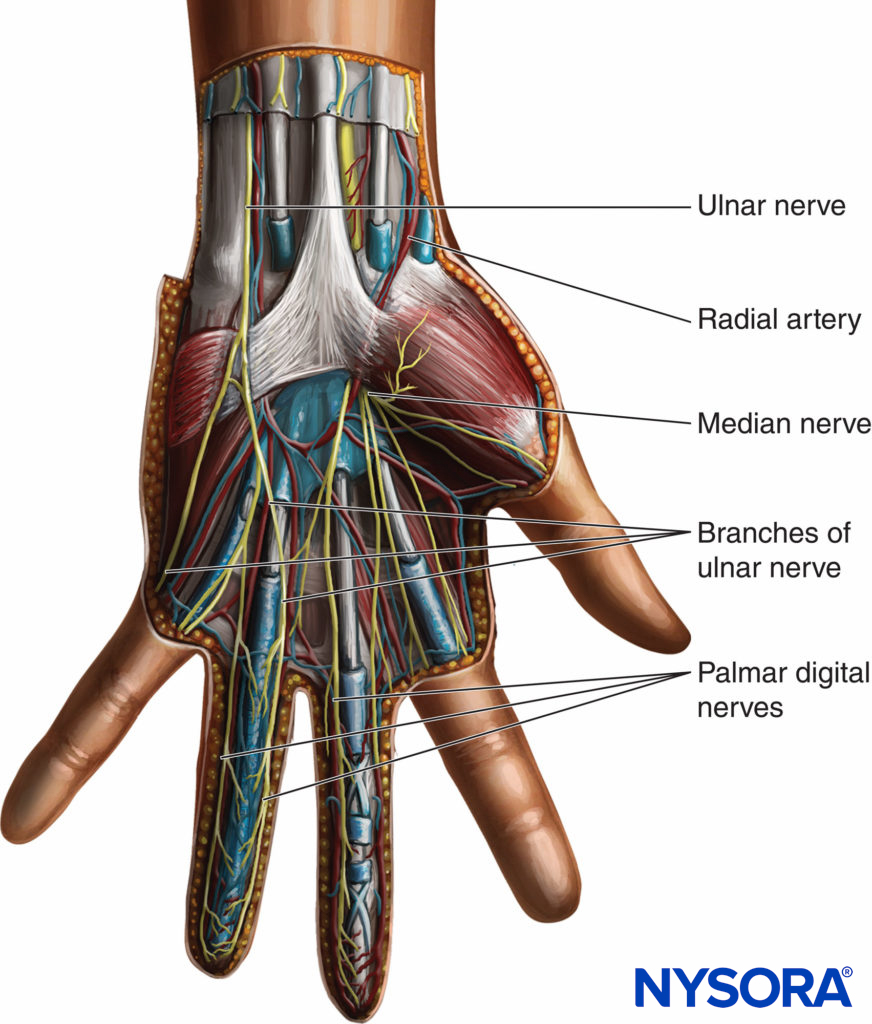
Figure 2. Cross-sectional view of the anatomy of the phalanx.
EQUIPMENT
A standard regional anesthesia tray is prepared with the following equipment:
- Sterile towels and 4-in. × 4-in. gauze pads
- A controlled, 10-mL syringe with local anesthetic
- One 1.5 -in., 25-gauge needle
Learn more about Equipment for Regional Anesthesia.
TECHNIQUE
Block of Volar and Dorsal Digital Nerves at the Base of the Finger
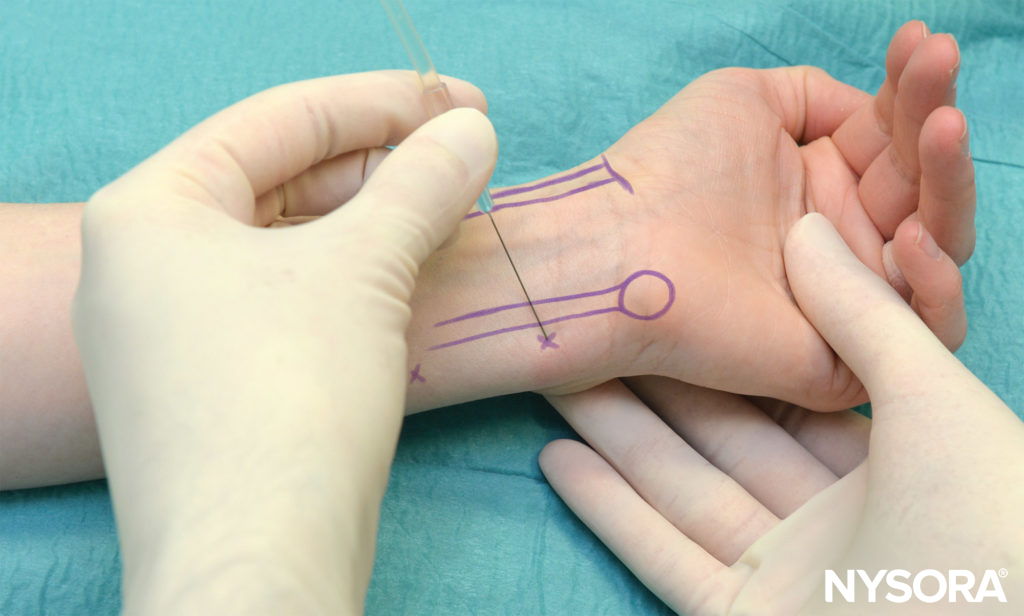
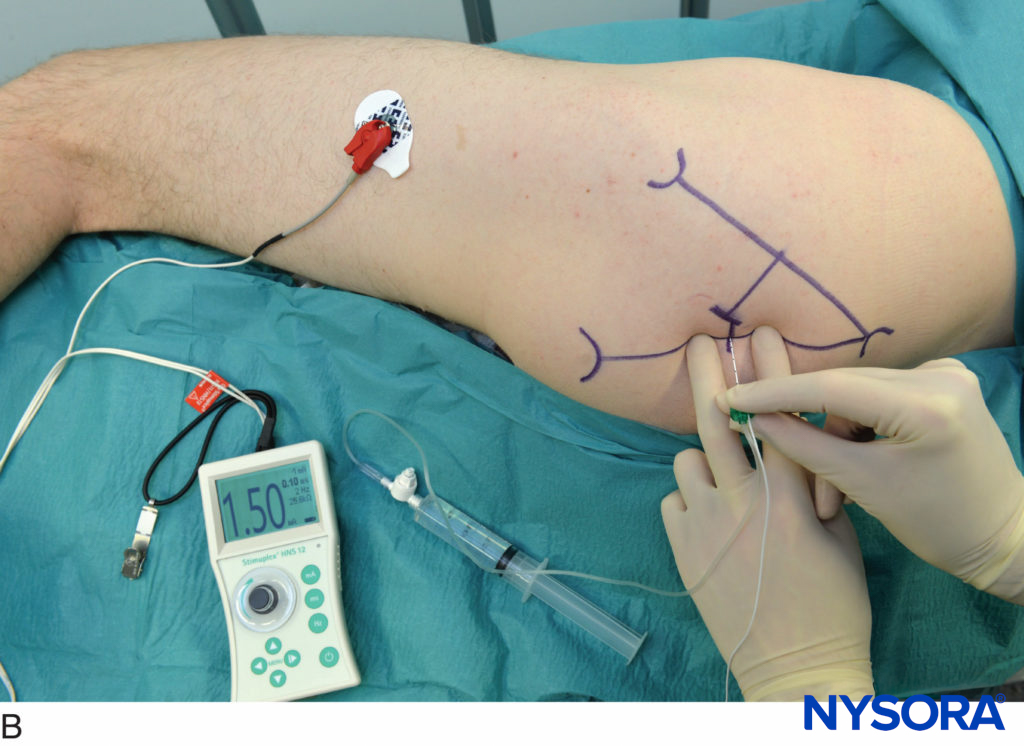
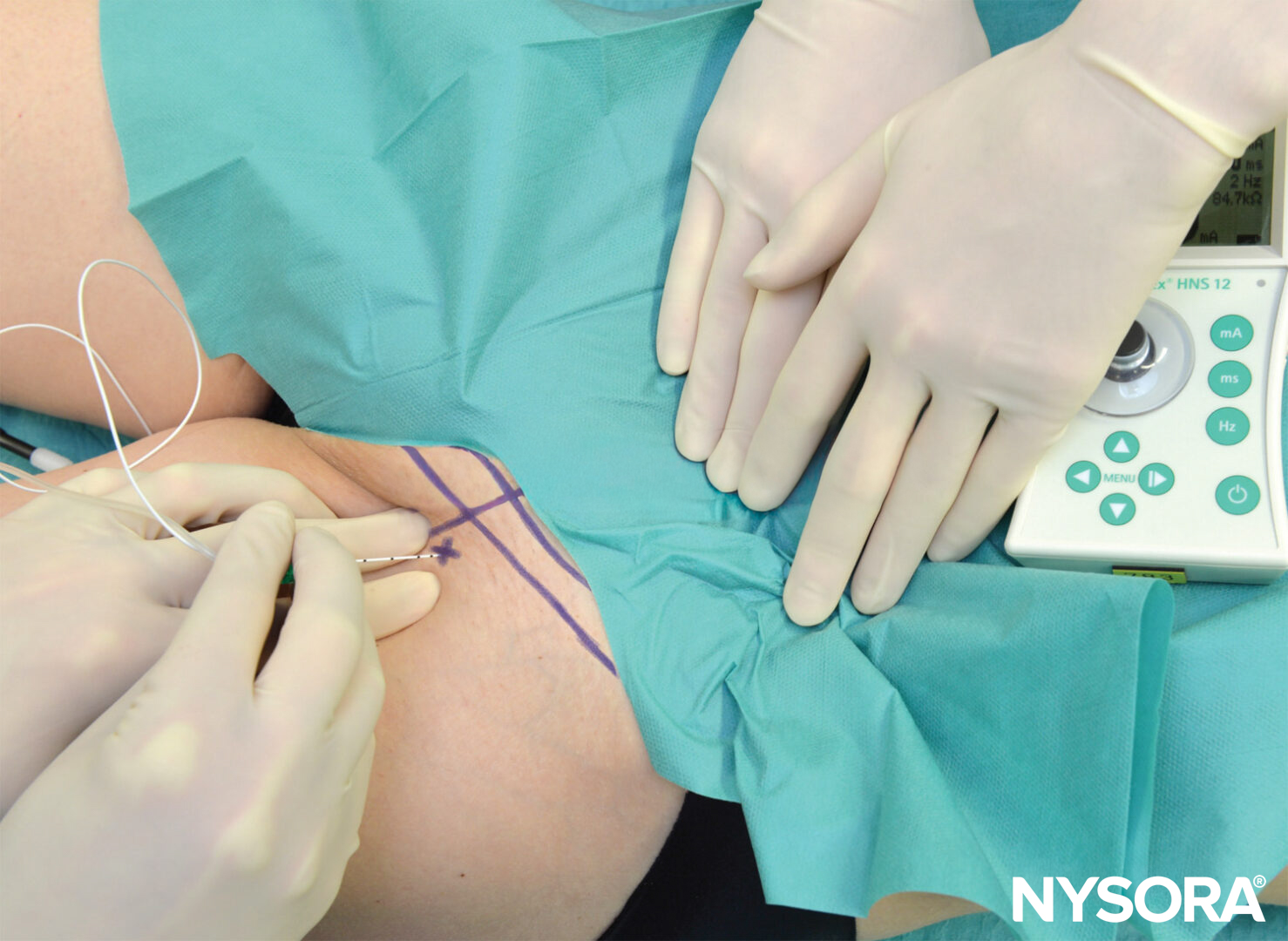
A 25-gauge, 1.5 -in. needle is inserted at a point on the dorsolateral aspect of the base of the finger, and a small skin wheal is raised. The needle is then directed anteriorly toward the base of the phalanx (Figures 3 and 4 ). The needle is advanced until it contacts the phalanx, while the anesthesiologist observes for any protrusion from the palmar dermis directly opposite the needle path (Figure 5 A and B). One milliliter of solution is injected as the needle is withdrawn 1–2 mm from the bone contact. An additional 1 mL is injected continuously as the needle is withdrawn back to the skin.

FIGURE 3. Angle of needle insertion for transthecal digital block.

FIGURE 4. The needle is shown inserted at the base of the proximal phalanx to block the medial digital nerve.

FIGURE 5. As the needle is inserted and injection is being made, the operator observes the palmar area to stop the advancement of the needle should a protrusion from the palmar dermis opposite the nerve tip be seen.
The same procedure is repeated on each side of the base of the finger to achieve anesthesia of the entire finger (Figure 6 A and B).
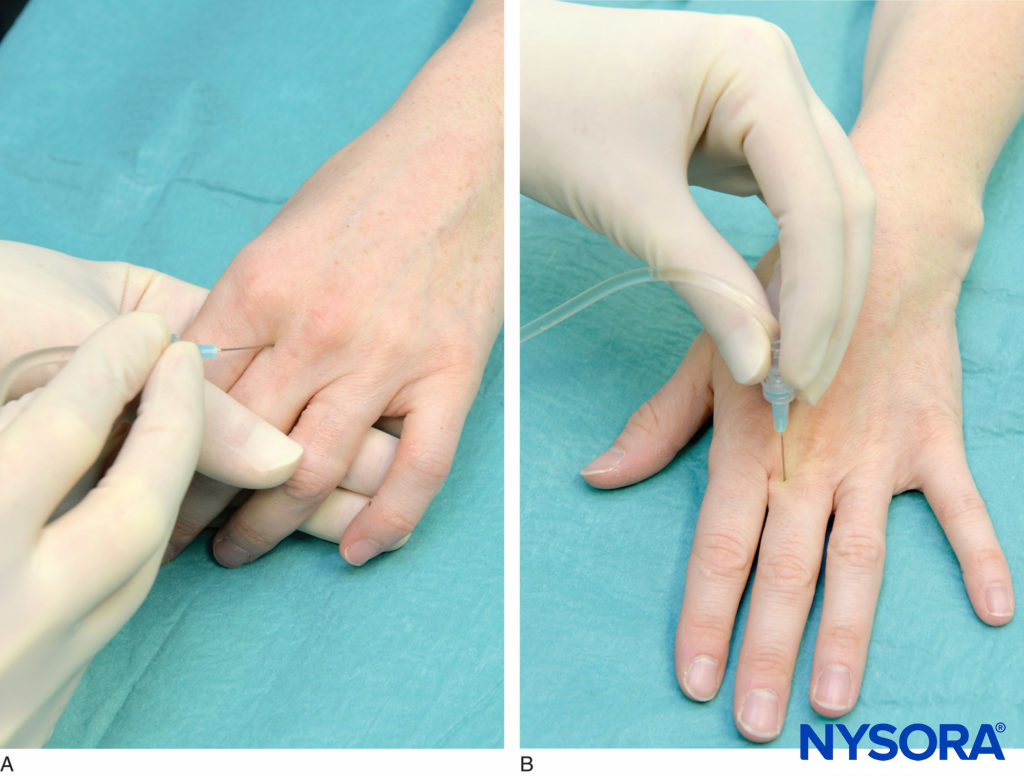
FIGURE 6. A and B: The identical procedure is repeated on the radial side of the proximal phalanx to block the radial branch of the digital nerve.
Transthecal Digital Block
The transthecal digital block is placed by using the flexor tendon sheath for local anesthetic injection. In this technique, the patient’s hand is supinated and the flexor tendon is located. Using a 25- to 27-gauge, 1-in. needle, 2 mL of local anesthetic is injected into the flexor tendon sheath at the level of the distal palmar crease (Figures 3 and 7). The needle should puncture the skin at a 45-degree angle. Resistance to the injection suggests that the needle tip is against the flexor tendon. Careful withdrawal of the needle results in the free flow of medication as the potential space between tendon and sheath is entered. Proximal pressure is then applied to the volar surface for the duration of the injection for the diffusion of the medication throughout the synovial sheath
NYSORA Tips
- The advantage of this approach is the provision of anesthesia to the entire digit with a single injection and a reportedly higher success rate.
- For more extensive surgery on the finger, it may be advantageous to combine both approaches discussed in this chapter for a greater success rate and more extensive distribution of anesthesia.

FIGURE 7. Transthecal digital block. The needle is placed into the flexor tendon sheath. To confirm the correct needle placement in the tendon sheath, the needle can be placed without the syringe, in which case the operator flexes and deflexes the finger. This should result in a free and substantial swinging of the needle.
BLOCK DYNAMICS AND PERIOPERATIVE MANAGEMENT
A skin wheal at the point of needle insertion significantly reduces the discomfort during the placement of the block. A digital block requires a small dose of a sedative or a narcotic during placement. Typical onset time for this block is 10–20 min, depending on the concentration and volume of local anesthetic used.
CHOICE OF LOCAL ANESTHETIC
The choice of the type and concentration of local anesthetic for a digital block is based on the desired duration of block (Table 1).
TABLE 1. Onset times and duration of anesthesia for some commonly used local anesthetics mixtures.
| Onset (min) | Anesthesia (h) | Analgesia(h) | |
|---|---|---|---|
| 1.5% Mepivacaine (+ HCO3 –) | 15–20 | 2–3 | 3–5 |
| 2% Lidocaine (+ HCO3 –) | 10–20 | 2–5 | 3–8 |
| 0.5% Ropivacaine | 15–30 | 4–8 | 5–12 |
| 0.75% Ropivacaine | 10–15 | 5–10 | 6–24 |
| 0.5% Bupivacaine (or L-bupivacaine) | 15–30 | 5–15 | 6–30 |
COMPLICATIONS AND HOW TO AVOID THEM
One specific complication of digital blocks is vascular insufficiency and gangrene. This catastrophe is a result of digital artery occlusion together with collateral circulation insufficiency. A series of causative factors is often involved to produce this rare, but serious complication (Table 2).
TABLE 2. Complications of digital blocks.
| Infection | This should be very rare with use of an aseptic technique. |
| Hematoma | Avoid multiple needle insertions. Use 25-gauge needle (or smaller) and avoid puncturing superficial veins. |
| Other | Instruct the patient on the care of the insensate finger. |
| Gangrene of the digit(s) | The use of epinephrine-containing solutions for this block is avoided by many; the safety of its use is controversial. Limit the injection volume to 3 mL on each side. The mechanical pressure effects of injecting solution into a potentially confined space should always be borne in mind, particularly in blocks at the base of the digit. In patients with small-vessel disease, perhaps an alternative method should be sought in addition to avoidance of digital tourniquet. |
| Nerve injury | Residual paresthesias are rare and may be due to an inadvertent intraneuronal injection. Systemic toxicity is rare because of the distal location of the block and small dose of local anaesthetic used. Do not inject when the patient complains of pain or when high resistance to injection is encountered. |
Clinical updates
Morales et al. (Regional Anesthesia & Pain Medicine, 2025) performed a cadaveric comparative dye study and found that the WALANT technique consistently stained the proper digital nerves (100%) without involving the common digital nerve, demonstrating more selective perineural spread than transthecal or interdigital blocks. In contrast, interdigital and transthecal injections showed extension to the common palmar digital nerves and adjacent finger nerves (up to 100% in the interdigital group), suggesting greater proximal and collateral spread; these findings support WALANT as anatomically targeted and potentially lower risk of unintended nerve exposure while maintaining effective digital blockade.
- Read more about the study HERE.
Gottlieb et al. (Journal of Emergency Medicine, 2022) provide a comparative review of digital nerve block techniques and report that single-injection approaches—particularly the volar subcutaneous block—offer similar or higher success rates (≈89%) compared with the traditional dorsal web space block (60–92%), with faster onset and lower procedural pain scores. The transthecal block demonstrated very high success (94–100%) but may be associated with post-injection sheath discomfort and slower onset, while dorsal approaches provide superior nail bed and dorsal anesthesia; the authors recommend volar subcutaneous block as first-line for palmar injuries, dorsal or transthecal techniques for dorsal involvement, and three-sided ring block for thumb or great toe injuries.
- Read more about the study HERE.