INTRODUCTION
The femoral nerve block is one of the most clinically applicable nerve block techniques that it is relatively simple to perform, carries a low risk of complications, and results in a high success rate.
INDICATIONS
Single-Injection Technique
A femoral nerve block is well suited for surgery on the anterior aspect of the thigh and for superficial surgery on the medial aspect of the leg below the knee. Some examples include repair of the quadriceps tendon or quadriceps muscle biopsy, long saphenous vein stripping, and postoperative pain management after femur and knee surgery.
A perineural catheter can be placed to provide prolonged analgesia for patients with fractures on the femoral neck or shaft. Femoral nerve block provides effective analgesia following total knee arthroplasty. A femoral nerve block can also be used to supplement a sciatic or popliteal block to provide complete anesthesia of the lower leg and ankle.
Continuous Technique
The primary indication of continuous femoral nerve block is pain management after major femur or knee surgery. In addition, when compared with a single-dose technique or placebo, continuous femoral nerve block significantly reduces postoperative morphine consumption in patients having a total hip replacement.
Continuous femoral nerve block provides excellent analgesia in patients with femoral shaft or femoral neck fractures. Its relative simplicity makes it uniquely suitable for use to provide analgesia in the emergency room and facilitate physical and radiologic examinations as well as manipulations of the fractured femur or hip. After major knee surgery, continuous femoral nerve block provides better pain relief than parenteral administration of opioids (IV PCA, intramuscular) or intra-articular analgesia. For knee surgery, continuous femoral block is as effective as continuous lumbar plexus block or continuous epidural analgesia but causes fewer complications.
CONTRAINDICATIONS
Relative contraindications for femoral nerve block include previous ilioinguinal surgery (femoral vascular graft, kidney transplantation), large inguinal lymph nodes or tumor, local infection, peritoneal infection, and preexisting femoral neuropathy.
ANATOMY
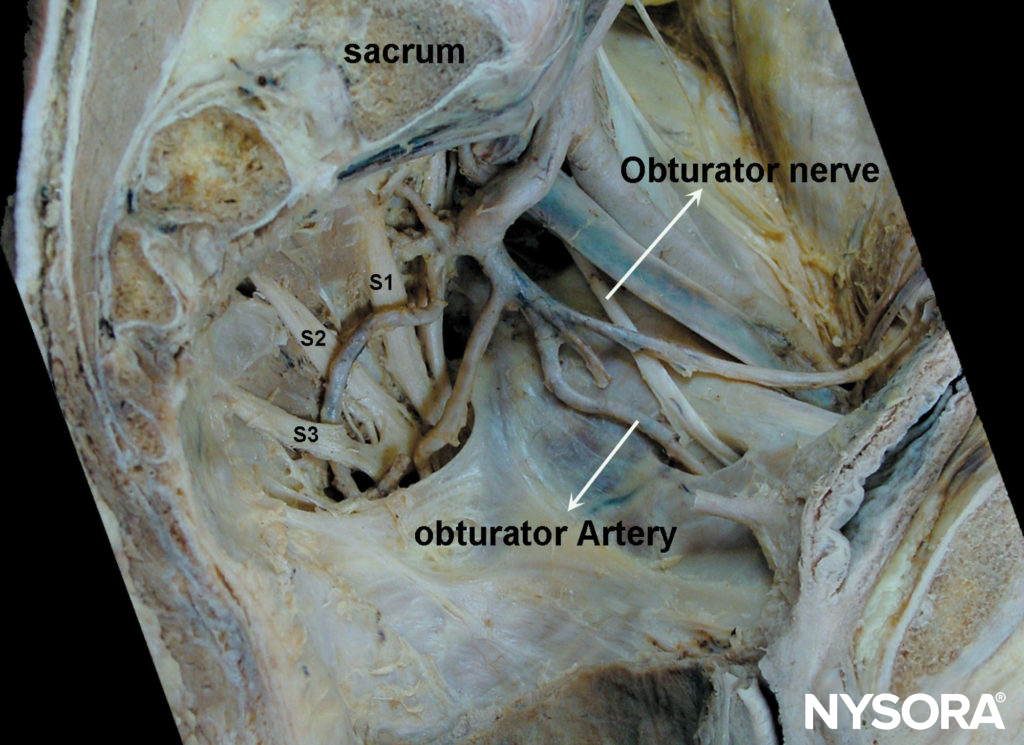
The femoral nerve is the largest branch of the lumbar plexus. It is formed by the dorsal divisions of the anterior rami of the L2, L3, and L4 spinal nerves. It emerges from the lateral border of the psoas muscle, approximately at the junction of the middle and lower thirds of that muscle. Along with its course to the thigh, it remains deep to the fascia iliaca. It enters the thigh posterior to the inguinal ligament, where it is positioned immediately lateral and slightly posterior to the femoral artery (Figure 1). At this level, it is situated deep to both fascia lata and fascia iliaca (Figure 2). As the nerve passes into the thigh, it divides into anterior and posterior branches (Figure 3). Located above the fascia iliaca, the anterior branches innervate the sartorius and pectineus muscles (Figure 4) and the skin of the anterior and medial aspects of the thigh.
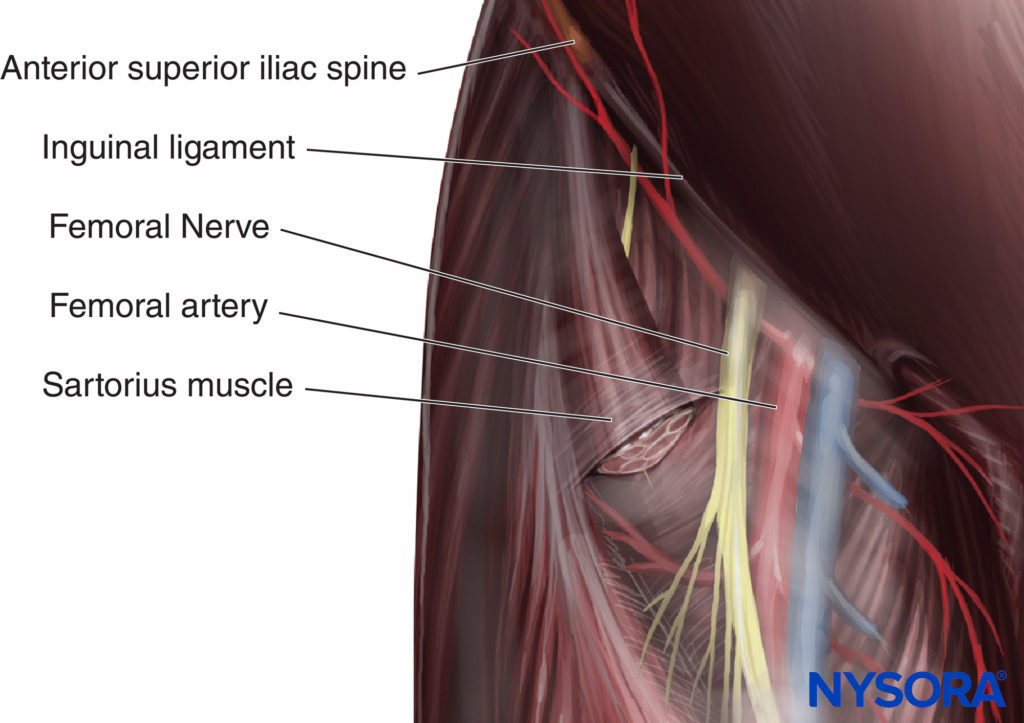
FIGURE 1. Anatomic relationship in the femoral triangle.

FIGURE 2. Tissue sheaths and femoral nerve, artery and vein relationships.

FIGURE 3. Composition of the femoral nerve at the level of block.
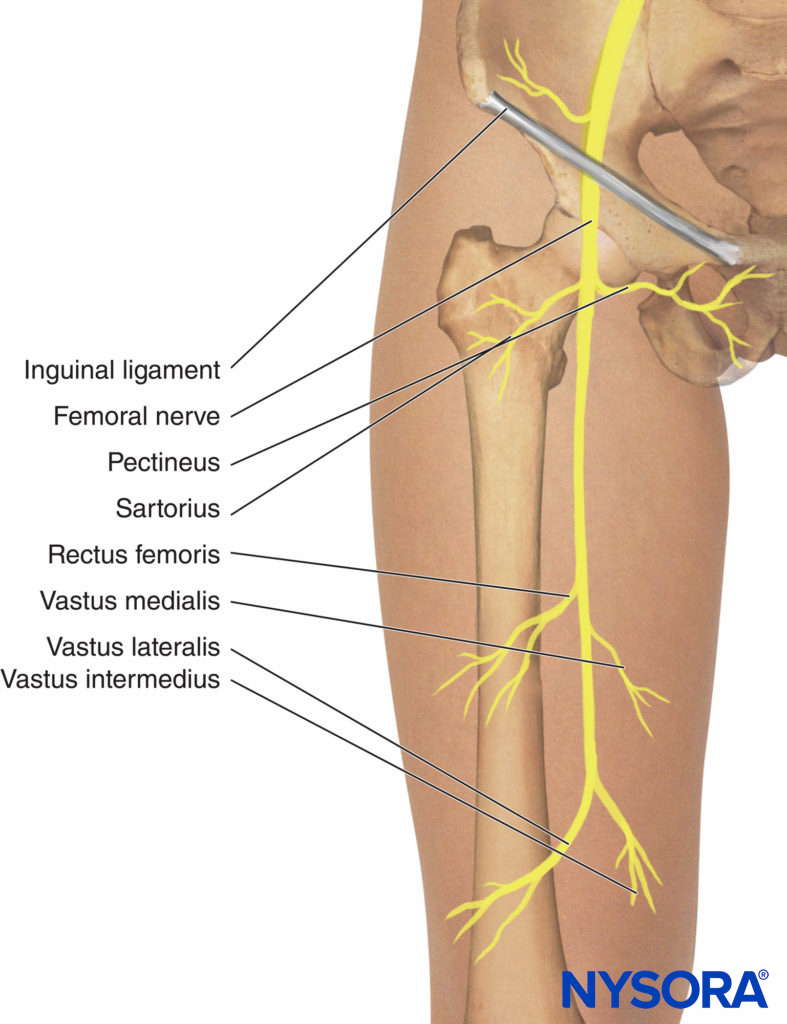
FIGURE 4. Motor branches of the femoral nerve.
NYSORA Tips
In obese patients, the identification of the inguinal crease can be facilitated by asking an assistant to retract the lower abdomen laterally (see Figure 7).
EQUIPMENT
A standard regional anesthesia tray is prepared with the following equipment:
- Sterile towels and gauze packs
- 20-mL syringe with local anesthetic
- Sterile gloves, marking pen
- One 25-gauge, 1.5-in. needle for skin infiltration
- A 5-cm long, short-bevel, insulated stimulating needle
- A peripheral nerve stimulator and a surface electrode
- Injection pressure monitor
Learn more about Equipment for Peripheral Nerve Blocks
BLOCK TECHNIQUE
Patient position. The patient lies in the supine position. The ipsilateral extremity is abducted 10–20 degrees and slightly externally rotated with the lateral side of the foot resting on the table.
The site of needle insertion (Figure 5) is located at the femoral crease but below the inguinal crease and immediately lateral (1 cm) to the pulse of the femoral artery. Located under the fascia iliaca, the posterior branches innervate the quadriceps muscle and the knee joint and give off the saphenous nerve. The saphenous nerve supplies the skin of the medial aspect of the leg below the knee (Figure 6).
Landmarks
The following landmarks are used to determine the site of needle insertion: inguinal ligament, inguinal crease, femoral artery (see Figure 6).

FIGURE 5. Anatomic landmarks for femoral nerve block. The needle insertion site (X) is located just below the inguinal crease, 1–2 cm lateral to the pulse of the femoral artery.
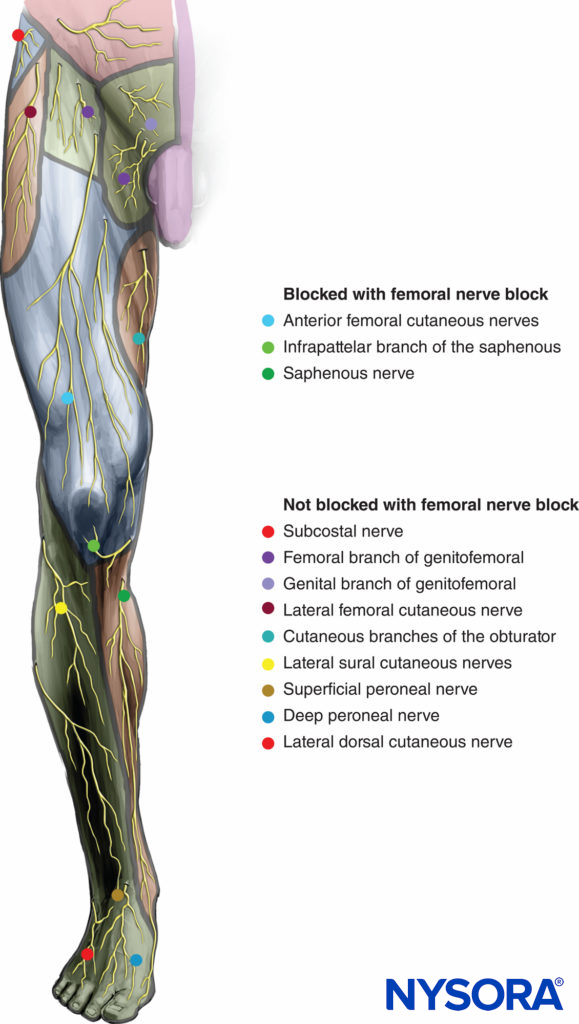
FIGURE 6. Sensory innervation of the femoral nerve and distribution of anesthesia with a femoral nerve block.
NYSORA Tips
- It is useful to think of the mnemonic VAN (vein, artery, nerve) going from medial to lateral when recalling the relationship of the femoral nerve to vessels at the inguinal crease.
- The femoral nerve is approached at the femoral crease, rather than at the inguinal ligament.
Single-Injection Technique
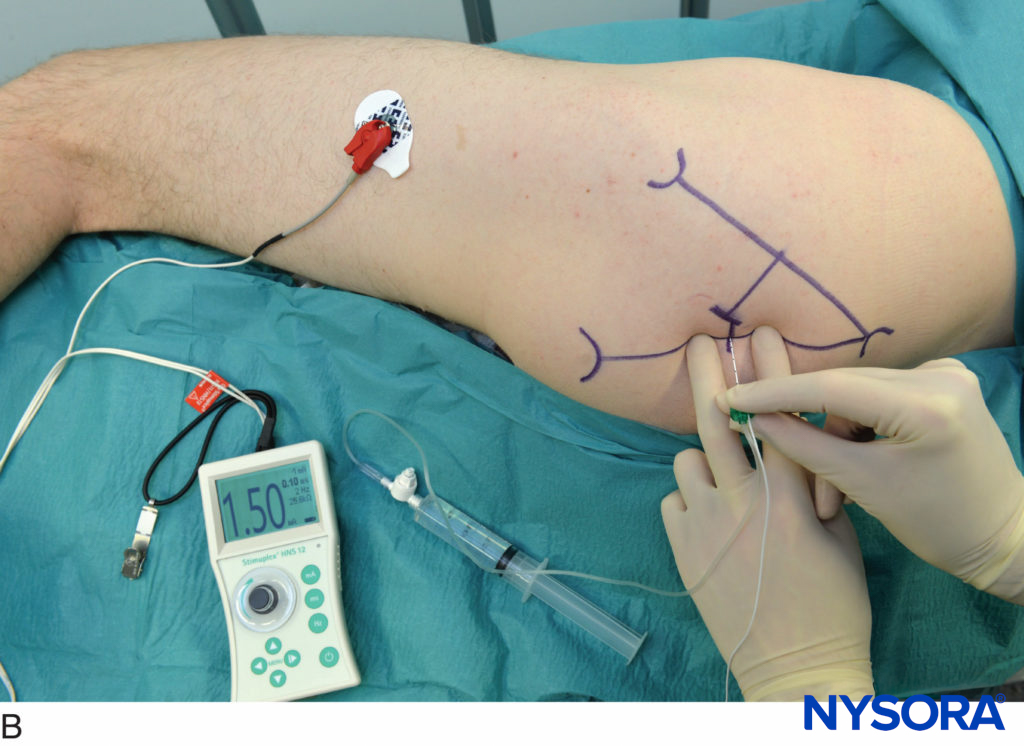
In obese patients, the lower abdomen is retracted laterally to allow access to the inguinal area (Figure 7). The needle is connected to a nerve stimulator set at a current intensity of 1 mA (0.1 msec/2 Hz) and introduced at a 30- to a 45-degree angle to the skin in a cephalad direction (Figure 8).

FIGURE 7. The abdomen is retracted laterally to facilitate exposure of the anatomy during femoral nerve block.
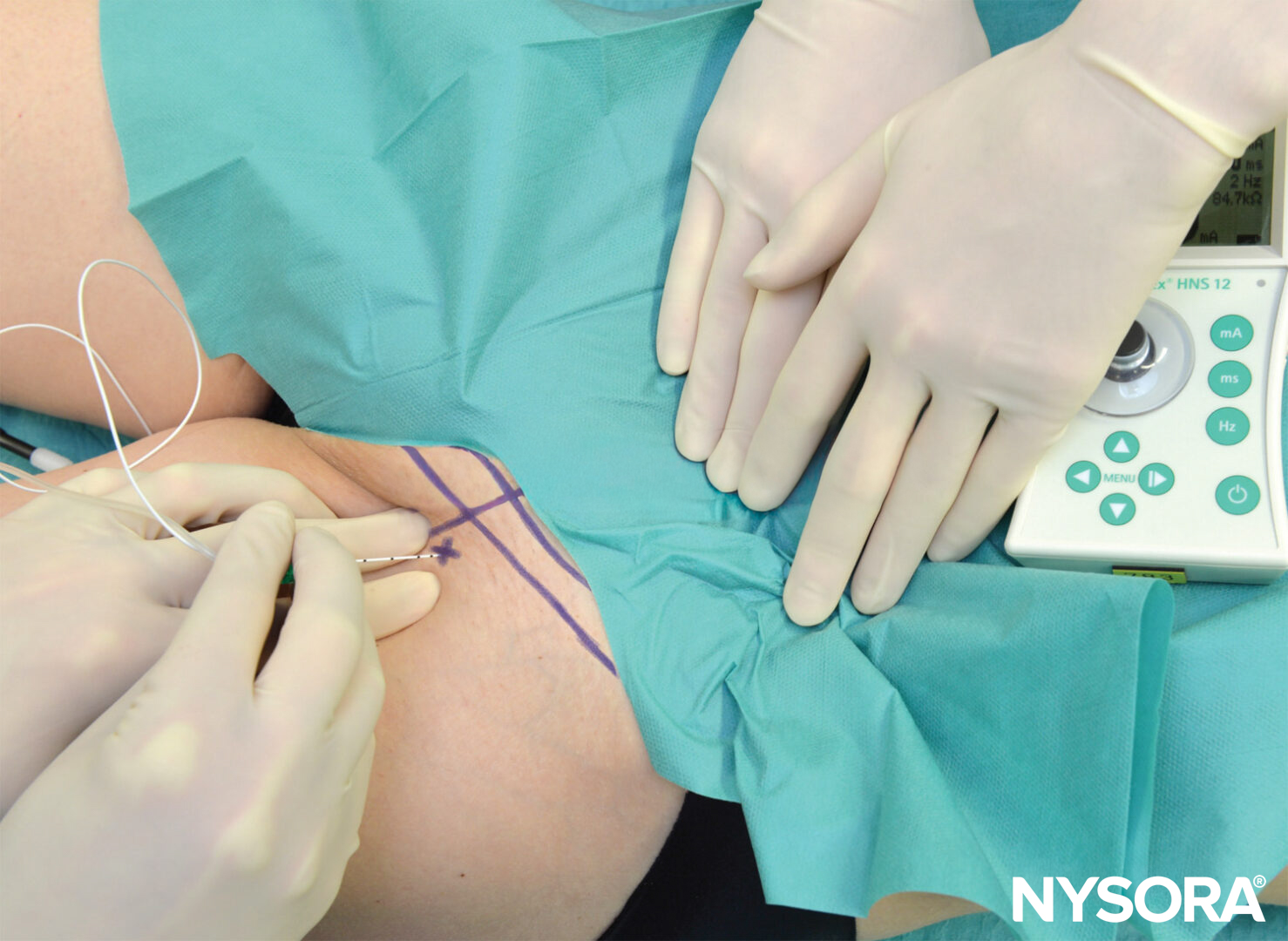
FIGURE 8. The needle is connected to a nerve stimulator set at 1 mA current intensity and introduced at a 30- to 45-degree angle to the skin in a cephalad direction.
The needle is advanced through the fascia lata and iliaca, often associated with a certain feeling of a “pop” as the needle pierces the fasciae. As the quadriceps muscle contractions (i.e., patellar twitch) are obtained, the current is gradually decreased while the needle is advanced. The position of the needle is adequate when patellar twitches are elicited with current output between 0.3 and 0.5 mA. After negative aspiration; 15–20 mL of local anesthetic is injected. Some common responses to nerve stimulation and appropriate action to troubleshoot are featured in Table 1.
TABLE 1. Common responses to nerve stimulation and action to obtain femoral nerve twitch.
| Response Obtained | Interpretation | Problem | Action |
|---|---|---|---|
| No response | The needle is inserted either too medially or to laterally | Femoral artery not properly localized | Follow the systematic lateral angulation and reinsertion of the needle as described in the technique |
| Bone contact | The needle contacts hip or superior ramus of the pubic bone | The needle is inserted too deep | Withdraw to the level of the skin and reinsert in another direction |
| Local twitch | Direct stimulation of the illiopsoas or pectineus muscle | Too deep insertion | Withdraw to the level of the skin and re-insert in another direction |
| Twitch of the sartorius muscle | Sartorius muscle twitch | The needle tip is slightly anterior and medial to the main trunk of the femoral nerve | Redirect the needle laterally and advance deeper 1–3 mm |
| Vascular puncture | Needle placement into the femoral or femoral circumflex artery, less commonly - femoral vein | Too medial needle placement | Withdraw and reinsert laterally 1 cm |
| Patella twitch | Stimulation of the main trunk of the femoral nerve | None | Accept and inject local anesthetic |
Multiple injection techniques have also been described, where vastus lateralis, intermedius, and medialis twitches are individually identified and separate injections of local anesthetic made at each nerve branch. When compared with a single injection, the total volume of local anesthetic required and the block onset time were significantly reduced. However, 14% of patients reported paresthesia, and 28% reported discomfort during block performance. Consequently, this technique has been largely abandoned as being unnecessary.
NYSORA Tips
- The needle tip must be positioned below fascia iliaca to obtain a complete femoral nerve block.
- Larger volume than 15-20 mL is not necessary because it is not associated with a better success rate.
Continuous Femoral Nerve Block
The continuous technique is similar to the single-injection technique. After passage through both fascia lata and iliaca, the needle is advanced to elicit a patellar twitch using a current output between 0.3 and 0.5 mA (0.1 msec) (Figure 9).
The catheter is then inserted 5 cm beyond the tip of the needle and secured in place. After a negative aspiration test for blood, a bolus dose of 10 mL of local anesthetic is injected and followed by a continuous infusion of dilute local anesthetic and/or intermittent boluses of 5 mL hourly. (Figure 10).
- Catheter insertion under the fascia iliaca should be without resistance. When this is not the case, the needle is probably not under the fascia iliaca. The needle should be withdrawn to the skin and reinserted.
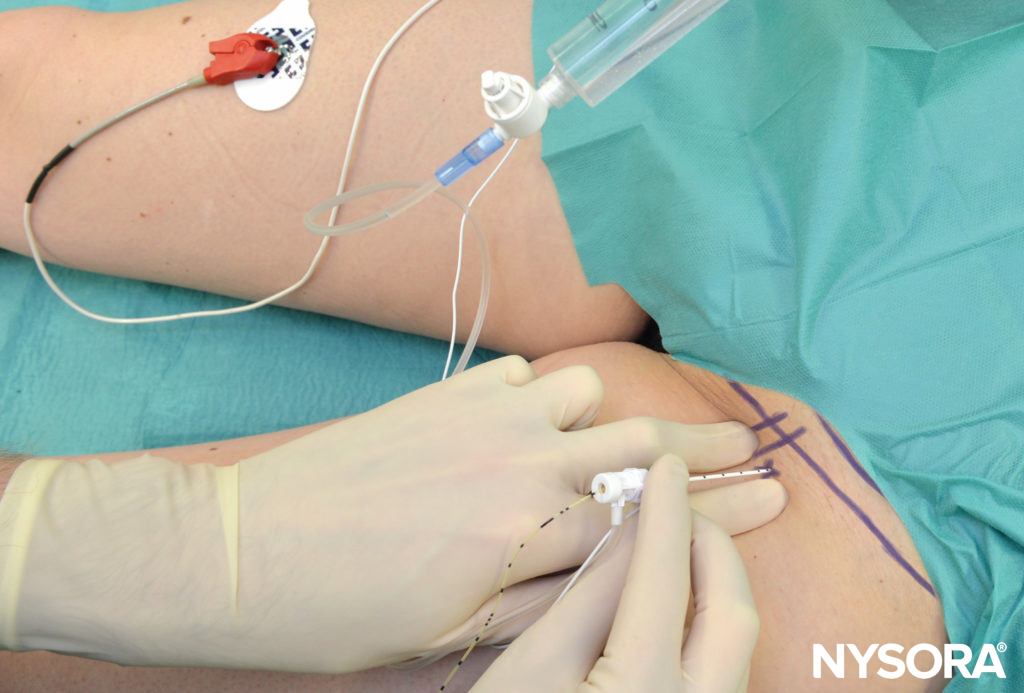
FIGURE 9. Continuous femoral nerve block: Needle insertion.

FIGURE 10. Spread of the injectate underneath the fascia iliaca after injection through the femoral catheter. (Used with permission from Dr. Philippe Gautier, Bruxelles, BE.)
Block Assessment
Sensory block is assessed by cold or pinprick test on the anterior and medial aspect of the thigh (femoral nerve) and on the medial aspect of the lower leg (saphenous nerve). Motor block is evaluated by asking the patient to extend the knee (e.g., to elevate the foot from the table).
CHOICE OF LOCAL ANESTHETIC
Single-Injection Technique
For surgical anesthesia, mepivacaine or lidocaine 1.5–2.0% or ropivacaine 0.5%–0.75% are frequently used, depending on the expected duration of surgery. For postoperative analgesia alone, a more dilute concentration of long-acting local anesthetic (eg ropivacaine or bupivacaine 0.2%–0.25%) is appropriate. Onset times and mean duration of both anesthesia and analgesia with different types and concentrations of local anesthetic solution are presented in Table 2.
TABLE 2. Onset and duration of 20 ml of local anesthetic in femoral block.
| Onset (min) | Anesthesia (h) | Analgesia (h) | |
|---|---|---|---|
| 3% 2-Chloroprocaine | 10–15 | 1 | 2 |
| 3% 2-Chloroprocaine (+ HCO3 + epi) | 10–15 | 1.5–2 | 2–3 |
| 1.5% Mepivacaine | 15–20 | 2–3 | 3–5 |
| 1.5% Mepivacaine (+ HCO3 + epi) | 15–20 | 2–5 | 3–8 |
| 2% Lidocaine | 10–20 | 2–5 | 3–8 |
| 0.5% Ropivacaine | 15–30 | 4–8 | 5–12 |
| 0.75% Ropivacaine | 10–15 | 5–10 | 6–24 |
| 0.5 Bupivacaine | 15–30 | 5–15 | 8–30 |
Continuous Technique
The initial bolus of 10–15 mL is followed by an infusion of dilute concentration (e.g., ropivacaine 0.2%). A typical infusion regimen is 5 mL/h basal infusion with a 5 mL/q60min patient-controlled bolus.
For additional information see Continuous Peripheral Nerve Blocks: Local Anesthetic Solutions and Infusion Strategies.
PERIOPERATIVE MANAGEMENT OF FEMORAL NERVE BLOCKS
The performance of femoral nerve block is associated with minor patient discomfort because the needle passes only through the skin and adipose of the inguinal region. Femoral nerve block is associated with weakness of the quadriceps muscle, leading to the decrease in its use in some practices, particularly where ultrasound is available for adductor canal blocks. This is because knee extension and weight-bearing on the blocked side are impaired with femoral nerve block, which must be clearly explained to the patient to reduce the risk of falls. The use of a knee immobilizer for ambulation following femoral nerve block has been shown to reduce the risk of falls, particularly following total knee arthroplasty.
Complications and How to Avoid Them
Complications of femoral nerve block include vascular puncture, femoral nerve compression by a hematoma, diffusion of the local anesthetic solution into the epidural space with the resultant epidural block, catheter shearing, and femoral nerve injury (incidence of 0.25%). With regard to continuous catheters, bacterial contamination of the catheters commonly occurs after 48 hours. However, local or systemic infection remains rare, with the estimated risk of 0.13%, Table 3.
TABLE 3. Femoral nerve block: complications.
| Hematoma | • When the femoral artery or vein is punctured, the procedure should be stopped and pressure applied over the puncture site for 2–3 min |
| Vascular puncture | • Maintain a palpating finger on the femoral pulse and insert the needle just lateral and parallel to the pulse. • The needle should never be directed medially. |
| Nerve injury | • Use a nerve stimulator avoid injection when motor response is present at <0.3 mA (0.1 msec). • Do not seek paresthesia as method of localization of FN because paresthesia is rarely elicited with femoral nerve block and should not be sought or relied on to indicate an intraneural injection. However, should severe pain on injection be reported, abort the injection. • Do not inject when high pressures on injection are encountered. • Use the minimal efficient volume and concentration of local anesthetic (15-20 mL). |
| Catheter infection | • Use strict aseptic technique during catheter insertion. • Sterile drapes should be used with continuous techniques. • Remove the catheter after 48–72 h (risk of infection increases with time). |
| Prevention of Falls | • Instruct patient on the inability to bear weight on the blocked extremity. |
SUMMARY
A femoral nerve block is easy to perform and associated with a low risk of complications. It is suitable for catheter insertion. When used alone, it is effective for surgery on the anterior thigh and for postoperative pain management after femur and knee surgery. When combined with sciatic and/or obturator nerve blocks, anesthesia of almost the entire lower limb from the midthigh level can be achieved.
Supplementary material related to this block can be found at Femoral Nerve Block Video and Ultrasound-guided femoral nerve block
Clinical updates
Tsai et al. (Journal of Clinical Medicine, 2022) report in a retrospective cohort of 607 geriatric ED patients with hip fracture that a lidocaine-based single-shot ultrasound-guided femoral nerve block (USFNB) reduced opioid use by ~80% compared with standard care and achieved meaningful pain relief 2.37× faster. Despite faster and opioid-sparing analgesia, ED and hospital length of stay were unchanged, and no block-related complications were observed, supporting USFNB as a safe, rapid, non-opioid analgesic strategy for early hip fracture pain control in older adults.
- Read more about the study HERE.
Ogawa et al. (Injury, 2021) report in a propensity score–matched pilot study of 78 elderly hip fracture patients (mean age 87 years, ~40% with dementia) that a single-shot femoral nerve block (FNB) performed intraoperatively under spinal anesthesia was associated with better early functional recovery, and improved mobility on postoperative day 2. The benefit was most evident among patients without dementia and those with femoral neck fractures; however, hospital length of stay was unchanged, suggesting that FNB may enhance early mobility rather than accelerate discharge.
- Read more about the study HERE.