Learning objectives
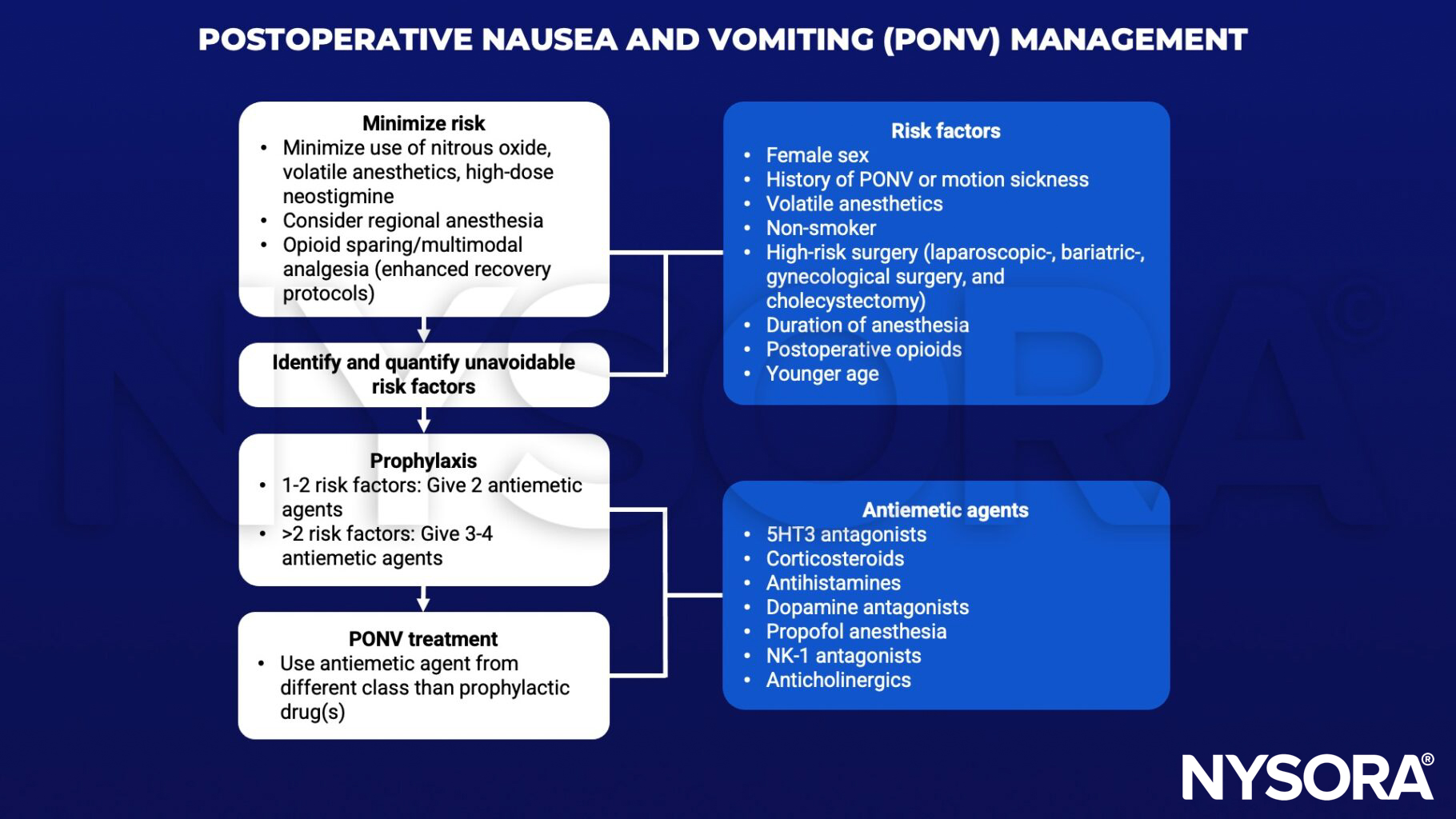
- Prevent and treat postoperative nausea and vomiting (PONV)
Definition
- Postoperative nausea and vomiting (PONV) is the second most common postoperative complication after pain
Scoring
Scoring systems like the Apfel simplified risk score can help raise awareness of PONV and thus increase prophylaxis use. The incidence of PONV, with the presence of 0, 1, 2, 3, and 4 risk factors is approximately 10%, 20%, 40%, 60%, and 80%, respectively.
| Risk factor | Points |
|---|---|
| Female gender | 1 |
| Non-smoker | 1 |
| History of PONV and/or motion sickness | 1 |
| Postoperative opioids | 1 |
| Sum of points | 0-4 |
Management
PONV in children
- Children have different risk factors for PONV than adults:
- Age ≥3 years
- History of PONV/motion sickness
- Family history of PONV
- Post-pubertal female
- High-risk surgery (strabismus, adenotonsillectomy, otoplasty)
- Surgery <30 minutes
- Volatile anesthetics
- Dexamethasone and 5HT antagonists are the antiemetics of choice in children:
- 0 risk factors
- No prophylaxis or dexamethasone or 5HT3 antagonist
- 1-2 risk factors
- Dexamethasone and 5HT3 antagonist
- >2 risk factors
- Dexamethasone and 5HT3 antagonist + consider total intravenous anesthesia
- 0 risk factors
Keep in mind
- Do not underestimate the severity of PONV, patients report that it’s a worse experience than pain
- PONV can lead to decreased patient satisfaction, aspiration, dehydration, increased length of stay and higher medical costs
Suggested reading
- Gan TJ, Belani KG, Bergese S, et al. Fourth Consensus Guidelines for the Management of Postoperative Nausea and Vomiting [published correction appears in Anesth Analg. 2020 Nov;131(5):e241]. Anesth Analg. 2020;131(2):411-448.
Clinical updates
Erdem et al. (Regional Anesthesia & Pain Medicine, 2025) conducted a prospective randomized double-blind trial in 81 patients undergoing single-level lumbar disc herniation surgery and found that bilateral preoperative ESP block reduced 24-hour PONV incidence from 34.1% to 10%, with significantly lower nausea at 0-12 hours, reduced rescue antiemetic use, and decreased intraoperative remifentanil requirements. Pain scores were significantly lower in the ESP group through 12 hours, rescue analgesic use was reduced, and postoperative pain intensity showed a strong early and moderate later correlation with nausea severity, suggesting analgesia itself may independently modulate PONV mechanisms.
Ao et al. (Anesthesia & Analgesia, 2025) performed a network meta-analysis of 15 RCTs (1310 patients) undergoing laparoscopic bariatric surgery and found that opioid-free anesthesia (OFA) reduced 24-hour PONV compared with opioid-sparing anesthesia (OSA), without improving pain scores or postoperative opioid consumption versus OSA. However, OFA was associated with a higher risk of perioperative bradycardia, while both OFA and OSA similarly decreased postoperative opioid use and pain compared with traditional opioid-based anesthesia.
Zhang et al. (Anesthesiology, 2025) report in a double-blind randomized trial of 240 women undergoing gynecologic laparoscopic surgery that adding 0.2 g intravenous pyridoxine to dexamethasone and ondansetron significantly reduced 24-h postoperative nausea and vomiting, driven mainly by a reduction in nausea, without affecting vomiting frequency, pain scores, opioid use, or inflammatory markers. Pyridoxine also reduced moderate-to-severe nausea and was not associated with adverse neurologic effects, though findings are limited to a single-center, female cohort and require multicenter validation .
Kovac (BJA Education, 2025) synthesizes current understanding of PONV pathophysiology, highlighting the central role of the area postrema, nucleus tractus solitarius, and multimodal receptor activation (5-HT3, D2, NK1, H1, M1, and μ-opioid), and details key modifiable anesthetic risk factors including volatile agents, nitrous oxide, and opioids. The review emphasizes validated risk-stratification tools—such as the Apfel score in adults and the POVOC score in children—to guide risk-adapted or multimodal prophylaxis strategies that can reduce institutional PONV rates from ~50% to <20% when systematically applied.










