Lumbar periradicular infiltrations (nerve root blocks) are well established in the diagnosis and management of lumbar radiculopathy [1]. Lumbar periradicular injections are preferentially performed as fluoroscopically or computed tomography (CT)-controlled interventions [2, 3]. However, both guidance modalities have significant radiation exposure, at least in part, expensive equipment. As an alternative guidance method, ultrasound (US) imaging is also applicable for spinal infiltrations [4–8] and for lumbar periradicular injections [9].
1. ULTRASOUND-GUIDED TECHNIQUE
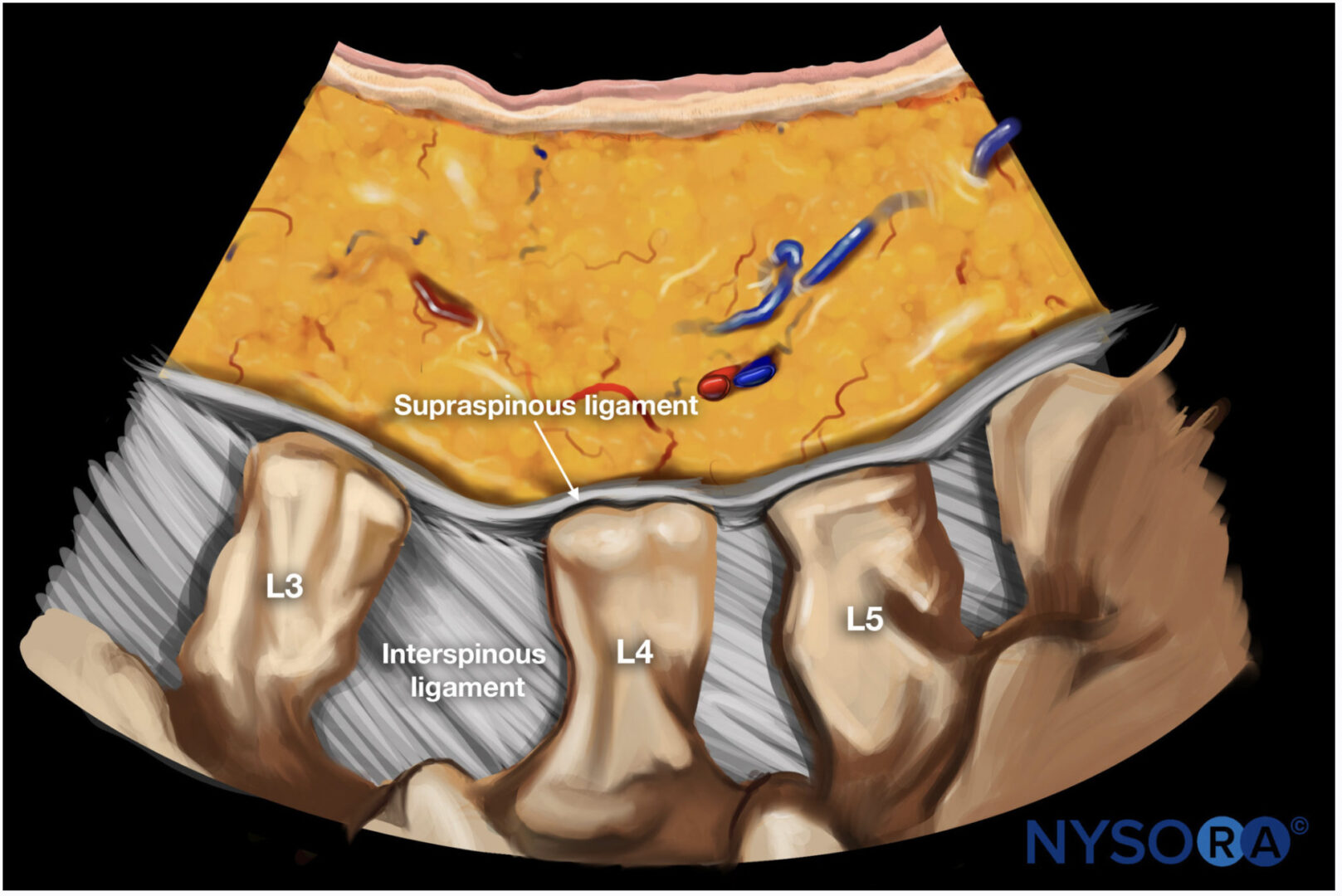
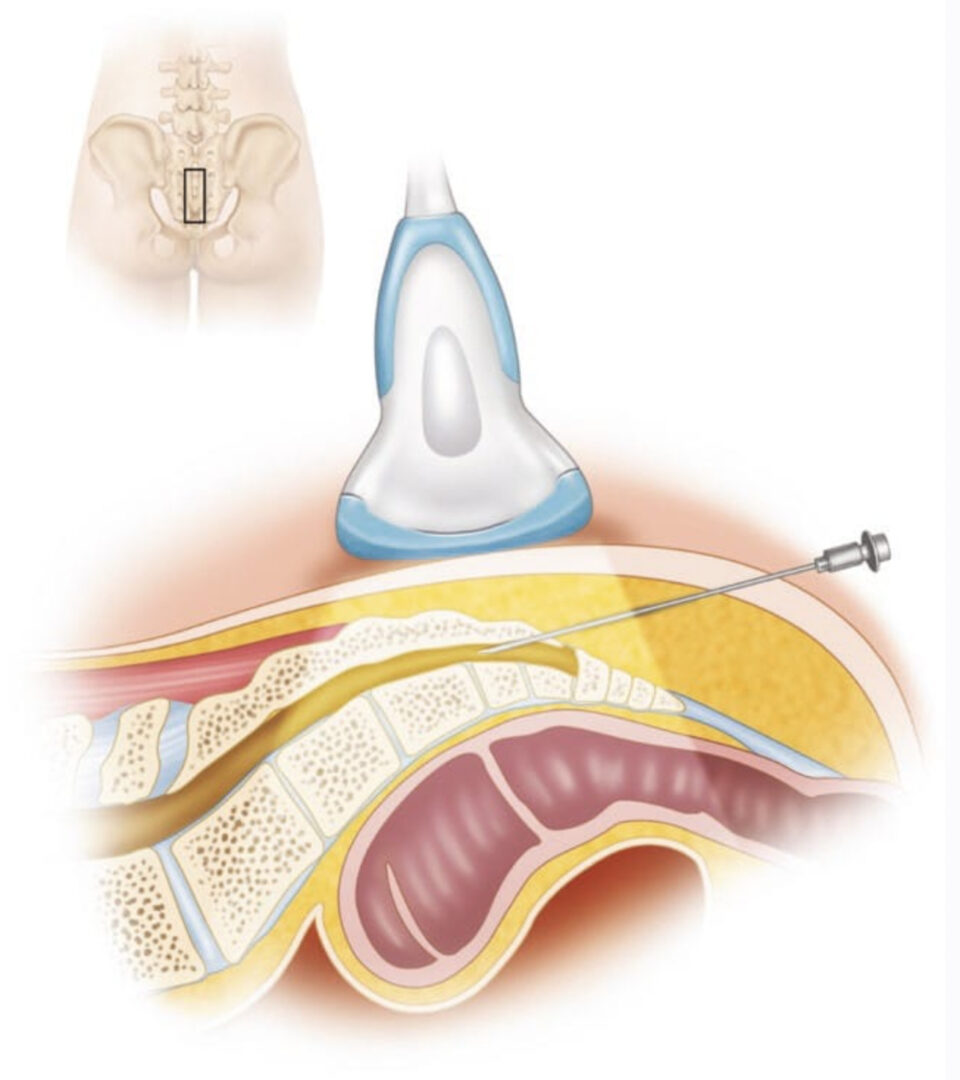
A standard US device with a broadband curved array transducer working at 2–5 MHz is usually used. The patients are positioned prone. To reduce lumbar lordosis, a cushion should be placed under the abdomen. The image gain should be set to maximum penetration as only the bony surfaces are of interest for the depictions. A posterior paravertebral para- sagittal sonogram is first obtained to identify the different spinal levels (Fig. 1). Then a transverse sonogram is obtained at the desired level. The spinous process and adjacent structures (lamina of vertebral arch, zygapophyseal articulations, inferior and superior facet, transverse process, and vertebral isthmus) have to be clearly delineated with Fig. 2.
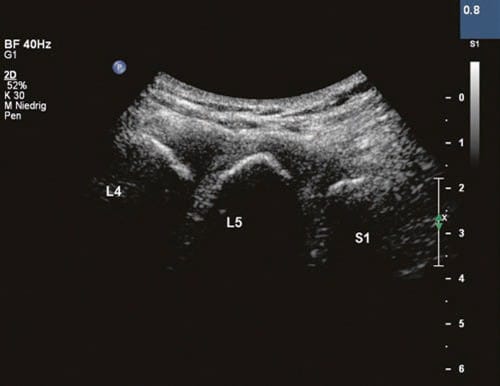
Fig. 1 Sagittal sonogram of the lumbar spine. S1 superficial part of spinous process S1, L5 superficial part of spinous process L5, L4 superficial part of spinous process L4
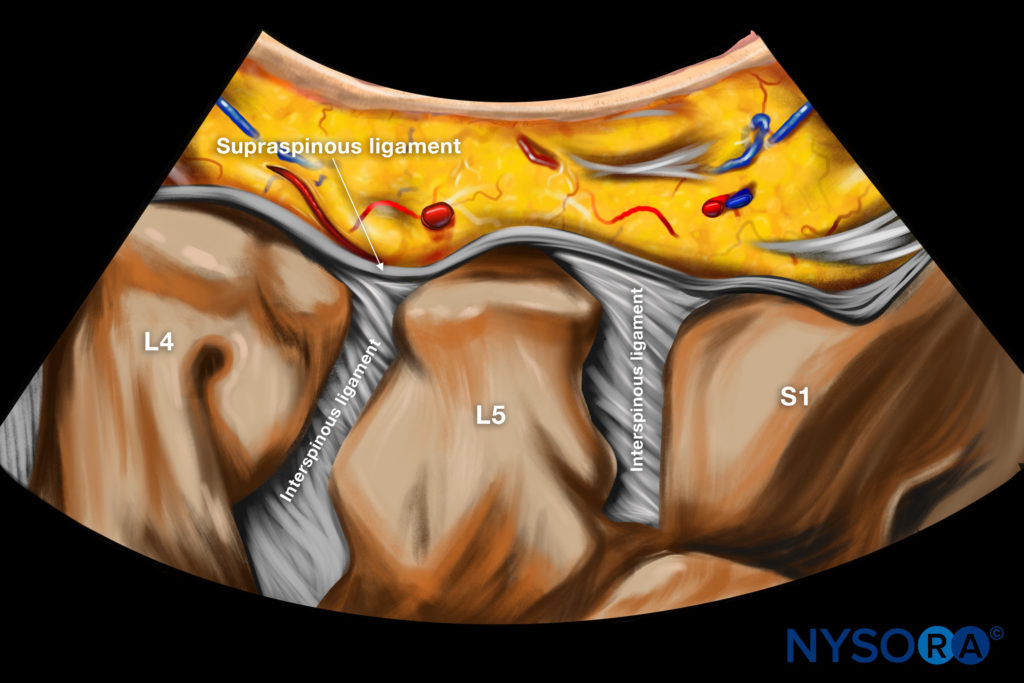
Reverse Ultrasound Anatomy illustration of figure 1.
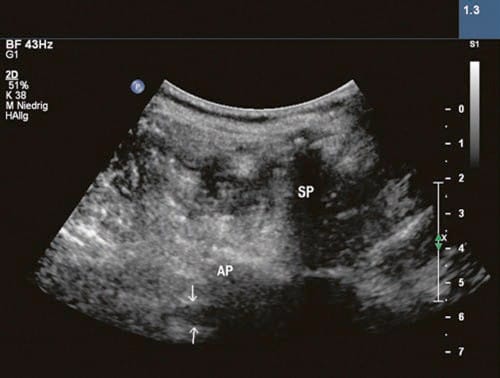
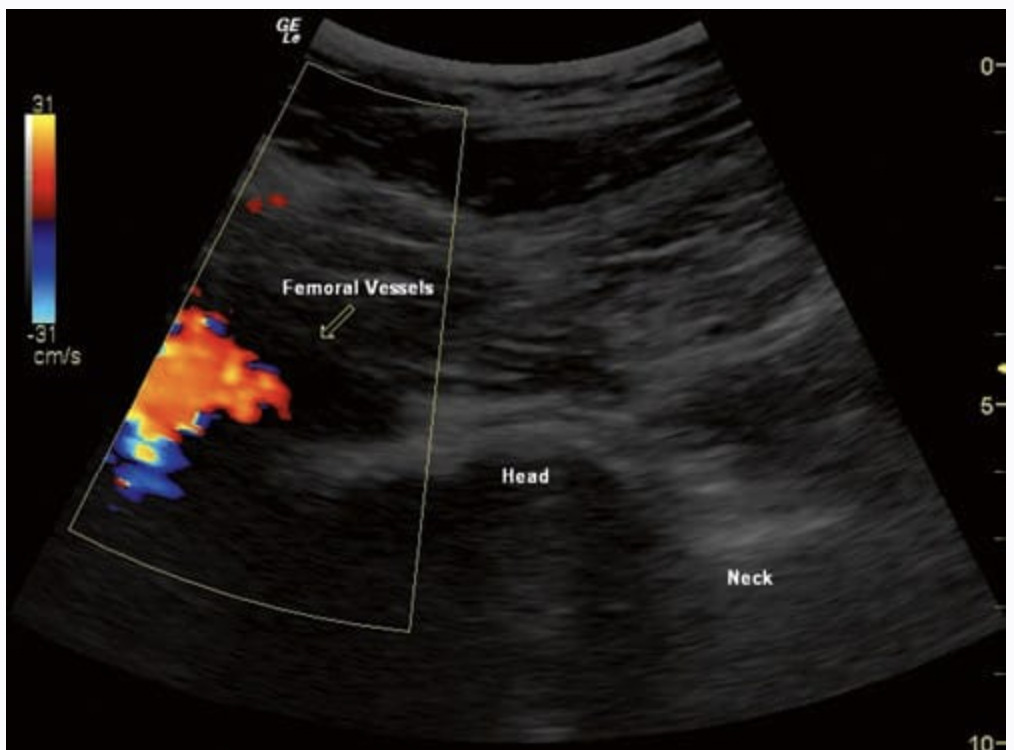
Fig. 2 Axial transverse sonogram of the intervertebral foramen at L4–L5 level. Arrows point at the exiting nerve root. SP spinal process, AP articular process
Once the correct level is identified in the sagittal plane, the transducer is rotated, and the corresponding spinous process is traced until the lamina can be delineated. The lamina should be demonstrated in their entire length to assess their lower margin. The next slit laterally is the facet joint space. Starting from this imaging, the intervertebral foramen and the corresponding spinal nerve can be traced [9] (Fig. 2).
The nerve root leaves the neuroforamen under the ligament between the transverse processes. The needle should be advanced very slowly when approaching the neuroforamen and going under the transverse processes, because radicular pain can be provoked. Sometimes the nerve root in the neuroforamen cannot be clearly depicted. In this case, we try to demonstrate both adjacent transverse processes before advancing the needle tip very slowly toward the neuroforamen. On approaching the nerve root, the patients will feel slight paresthesia along the corresponding nerve root territory (clinical control), at which point the needle is slightly withdrawn and the medication delivered.
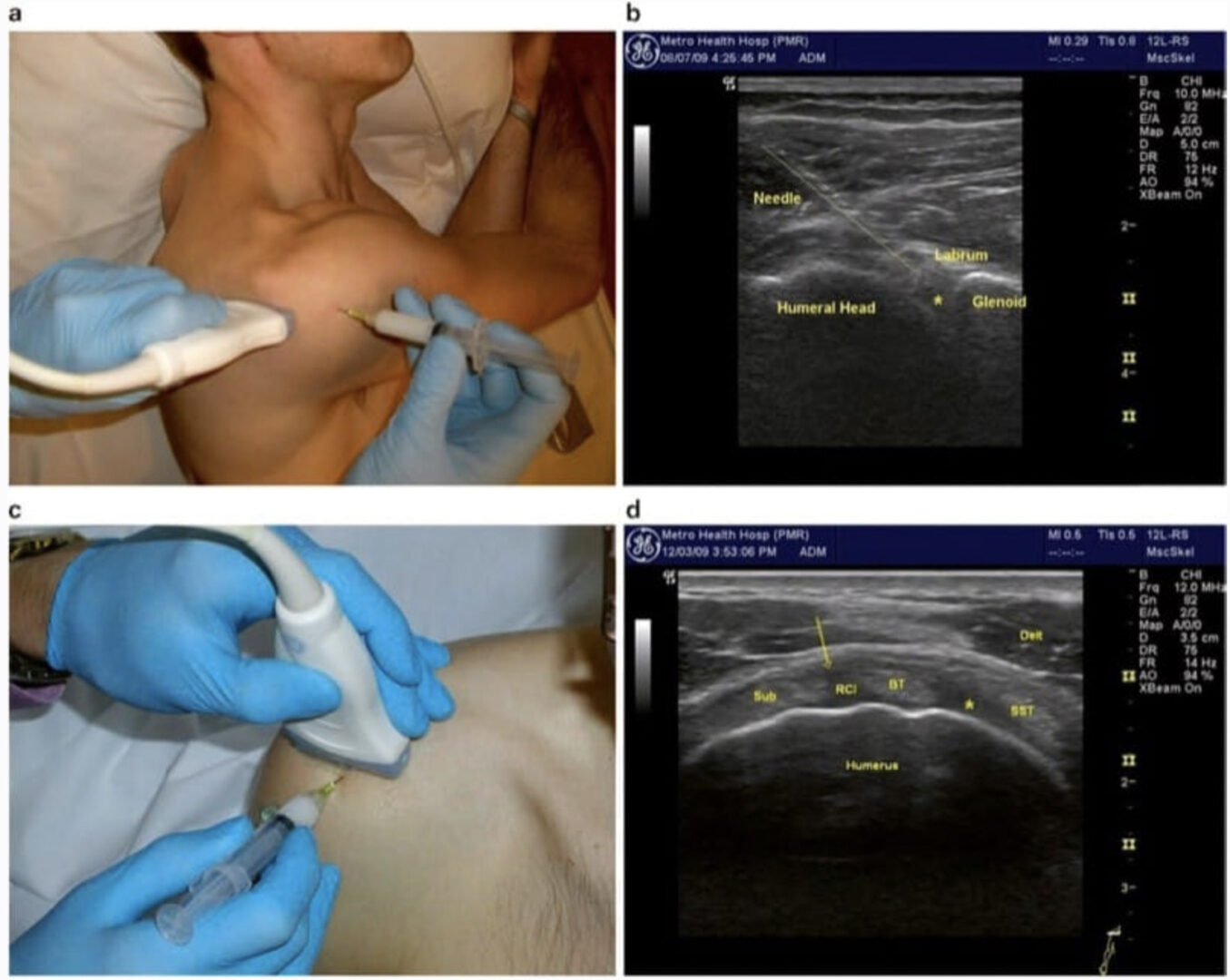
We recommend the “in-plane-technique” in which the whole needle path is under control at any time and no mismatch between needle, needle tip, and target is actually possible (Fig. 3).

Fig. 3 Axial transverse sonogram of the intervertebral foramen at L4–L5 level showing the needle in plan targeting the neuroforamen
2. LIMITATIONS OF THE ULTRASOUND-GUIDED TECHNIQUE
For a successful infiltration, two conditions are required: a clear depiction of the target and a clear delineation of the needle (tip) directed to the target. Therefore, the first step is to adjust the US modalities for the lumbar approach. To visualize the bony surfaces, a hard image (maximum penetration gain) has to be captured by using an appropriate setting with modified gain and persistence. Otherwise, the patient’s tissue shows up differently, compromising the sonoanatomy and the possibility to achieve clear sonographic images. In our experience, the depiction of the target can be particularly demanding in patients with an altered fatty muscle consistency. Such tissue is like foam plastic and cannot be penetrated by the US signal, which results in a low picture quality. Obviously, in obese patients or subjects with prior lumbar surgery (distinct scar formation, instrumentation, laminectomy), to date, the US approach cannot be recommended. Keeping the needle tip in the viewing field as the needle is advanced toward the target requires some practice. Failing to do so was the most common mistake observed in residents being trained on US-guided peripheral nerve blocks. Persistent failure to visualize the needle tip was documented even after performing more than 100 US-guided peripheral nerve blocks, suggesting that experienced practitioners can also face substantial difficulties.
Needle advancements and/or drug injections without adequate needle tip visualization may result in unintentional vascular or neural injuries. Using surrogate markers of tip location, such as tissue movement (jiggling the needle in small, controlled, in-out movements) and hydrolocation (rapid injection of small amount of fluid, 0.5–1 ml), is sometimes very helpful [10]. A promising feature to visualize the needle tip might be the development of needles with a sensor in the needle tip. This sensor would be recognized by the US technology and reported in real-time in the sonographic picture. Nevertheless, this technique and its practical impact still have to be evaluated.
In our experience, lumbar spinal periradicular infiltrations are feasible in most patients. However, intravascular injections cannot be reliably recognized in all patients as the ultrasound will lack enough resolution at such depth.