Anatomy of the Cervical Facet Joints Cervical facet joints are diarthrodial joints formed by the superior articular process of one cervical vertebra articulating with the inferior articular process of the vertebrae above at the level of the junction of the lamina and the pedicle. The angulation of the facet joint increases caudally, being about 45 degrees superior to the transverse plane at the upper cervical level to assuming a more vertical position at the upper thoracic level. The superior articular process also faces in a more posteromedial direction at the upper cervical level, and this changes to a more posterolateral position at the lower cervical level, with C6 being the most common transition level [1, 2]. Each facet joint has a fibrous capsule and is lined by a synovial membrane. The joint also contains varying amounts of adipose and fibrous tissue, forming different types of synovial folds contributing to different pathophysiologies for joint dysfunction [3]. Excessive facet joint compression and capsular ligament strain have been implicated in neck pain after whiplash injury [4]. The facet joint and capsule have been shown to contain nociceptive elements suggesting that they may be an independent pain generator [5]. Facet joint degeneration is more common in the elderly, and the prevalence of facet joint involvement in chronic neck pain has been reported to be from 35% to 55% [6, 7].
1. INDICATIONS FOR CERVICAL ZYGAPOPHYSEAL JOINT INTRA-ARTICULAR INJECTION
Facet joint-mediated pain cannot be diagnosed based only on clinical examination or radiologic imaging. Cervical facet intra-articular injection has been utilized in the diagnosis and management of facetogenic pain [8]. However, evidence for effective relief of neck pain with cervical zygapophyseal injections is lacking [9, 10]. Cervical medial branch block is still considered the gold standard to diagnose pain stemming from the facet joints [11].
2. LITERATURE REVIEW OF ULTRASOUND-GUIDED CERVICAL FACET INJECTIONS
Galiano and colleagues [12] reported the feasibility of ultrasound (US)-guided cervical facet joint intra-articular injections in cadavers using a lateral approach. The facet joints from C2–C3 to C6–C7 were accurately identified in 36 of 40 cases. CT confirmed needle tip placement inside the joint space. The same group later studied and advocated the use of an ultrasound-guided CT-assisted navigation system as a teaching tool for performing facet injections [13].
Obernauer and coworkers [14] conducted a prospective randomized clinical trial to evaluate accuracy, timesaving, radiation doses, and pain relief of US guided cervical facet joint injections versus computed tomography (CT)-controlled interventions. Forty adult patients were consecutively enrolled and randomly assigned to the US or CT group. The accuracy of US-guided interventions was 100%. The mean time (min/sec) to final needle placement in the US group was 04:46 versus 11:12 (p < 0.05) in the CT group for one injected level and 05:49 in the US group versus 14:32 (p < 0.05) in the CT group for two injected levels. Both groups showed the same significant visual analog scale (VAS) relief in pain. The authors concluded that US-guided cervical facet intra-articular injections show the same therapeutic effect as CT-guided intra-articular injections and result in a significant reduction of procedure duration without any exposure to radiation [14].
3. ULTRASOUND-GUIDED TECHNIQUE FOR CERVICAL FACET INTRA-ARTICULAR INJECTION
Lateral Approach
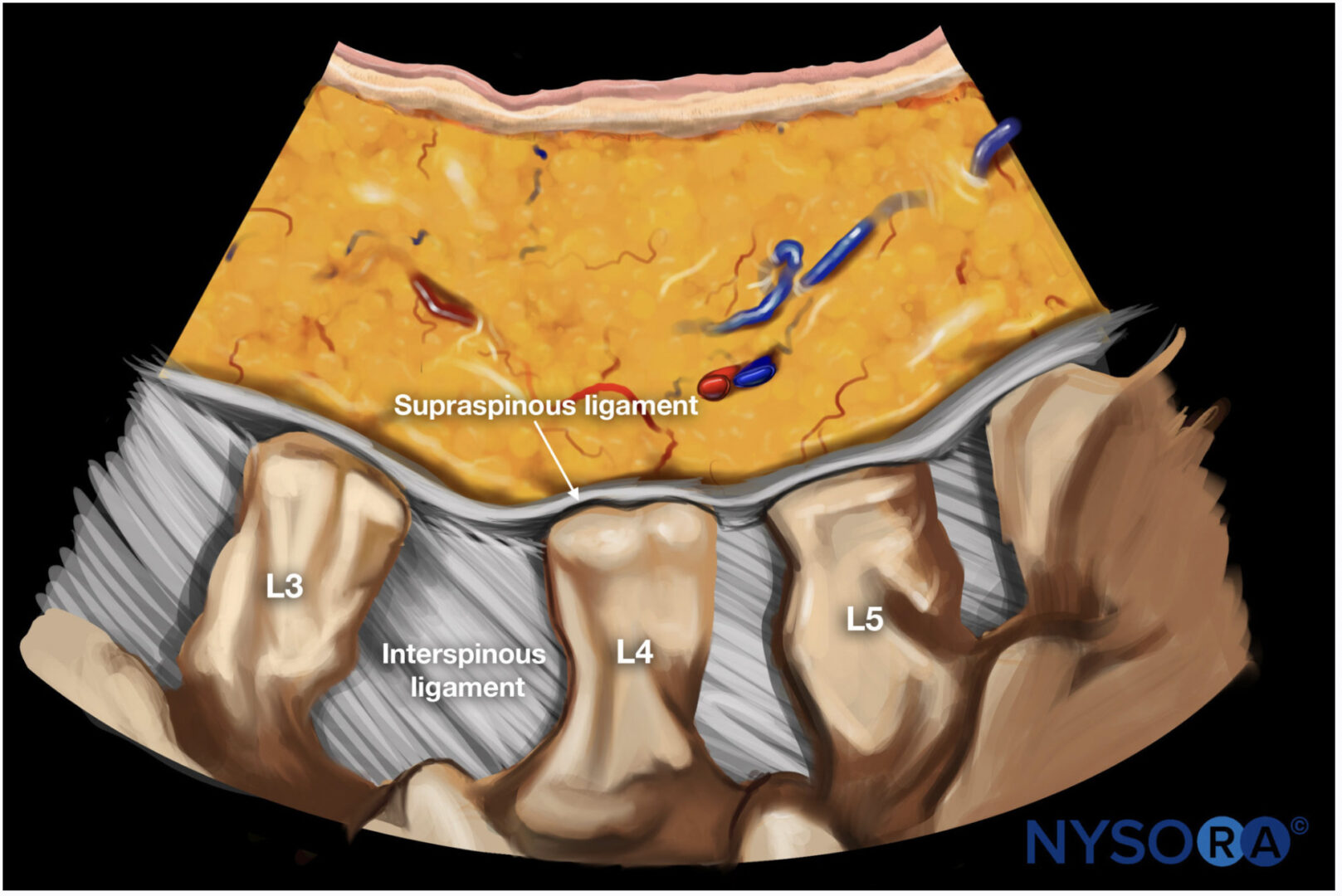
The patient is placed in the lateral position, and the correct cervical level is identified (see Chap. 8). A high-frequency linear transducer is used to obtain a short-axis view. The superior articular and the inferior articular processes forming the facet joint appear as hyperechoic signals and the joint space in between as an anechoic gap (Fig. 1). The needle is inserted at the lateral end of the transducer and advanced from posterior to anterior—in plane—under real-time ultrasonography to the target (joint space) [15].
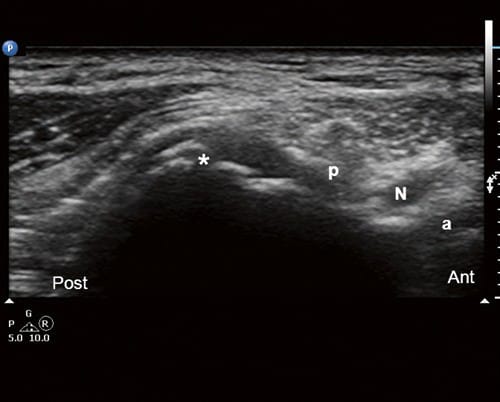
Fig.1 Short-axis (transverse) US image at the level of the articular pillar showing the C5-C6 joint space (asterisk). a anterior tubercle; N nerve root; p posterior tubercle
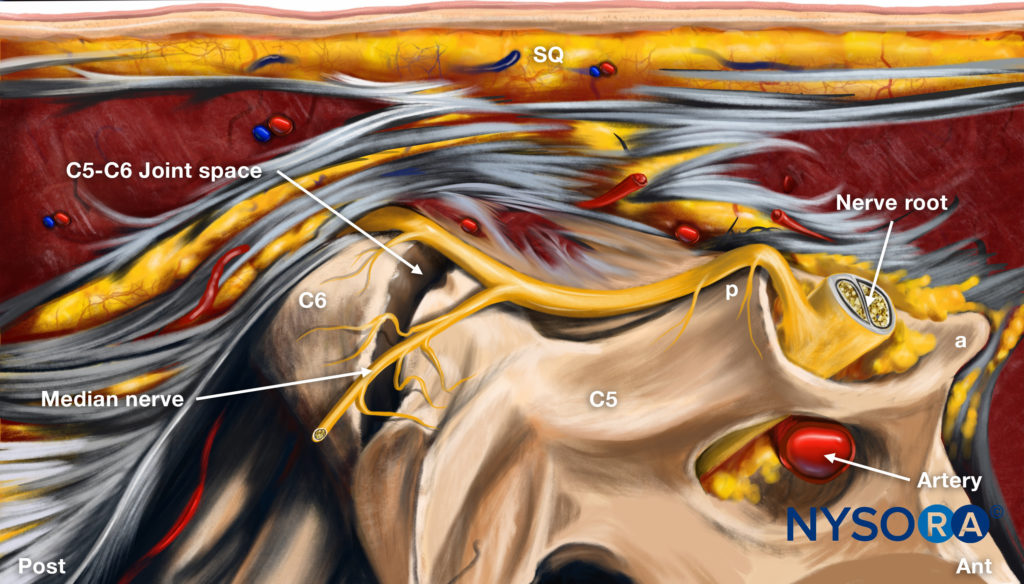
Reverse Ultrasound Anatomy illustration of figure 5. SQ, subcutaneous tissues; p, posterior tubercle; a, anterior tubercle.
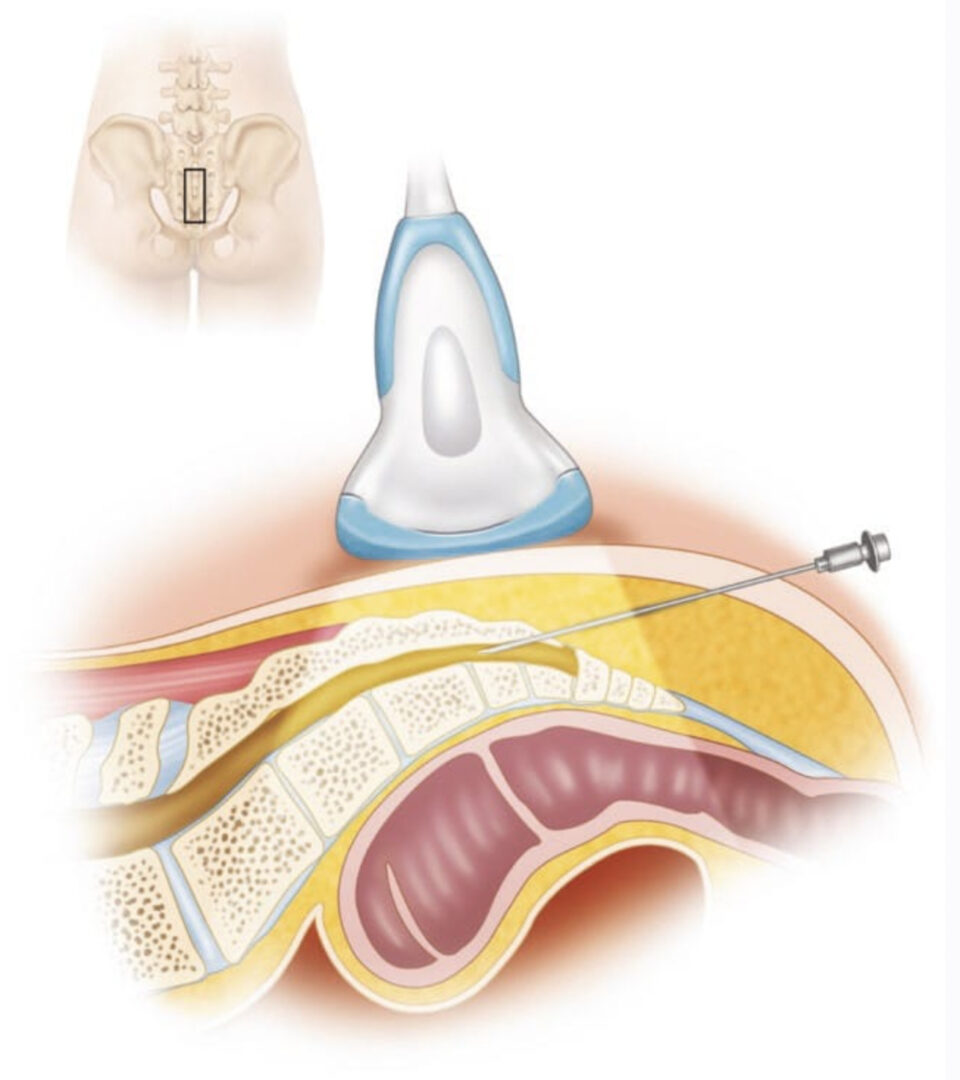
4. POSTERIOR APPROACH
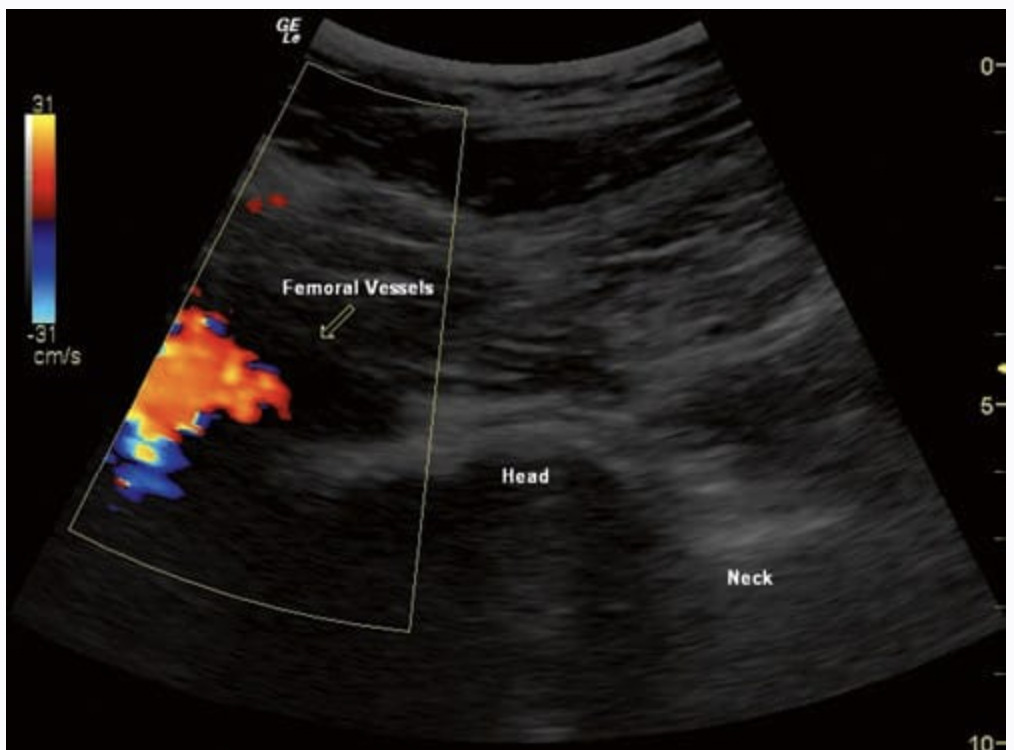
The posterior approach is more practical than the lateral one because the patient is in the prone position, and bilateral injections can be performed without the need to change position. A sagittal scan is obtained first at the midline to identify the correct cervical level. C1 spine has no or rudimentary spinous process, and the first identified bifid spinous process belongs to C2 (Fig. 2).
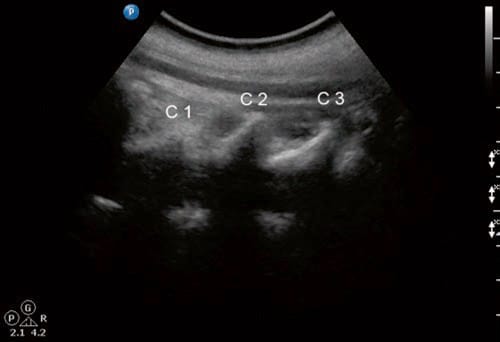
Fig.2 A midline longitudinal scan through the cervical spinous processes level. Note that the C1 immediately caudal to the occiput has only a rudimentary spinous process compared to the bifid spinous process of C2
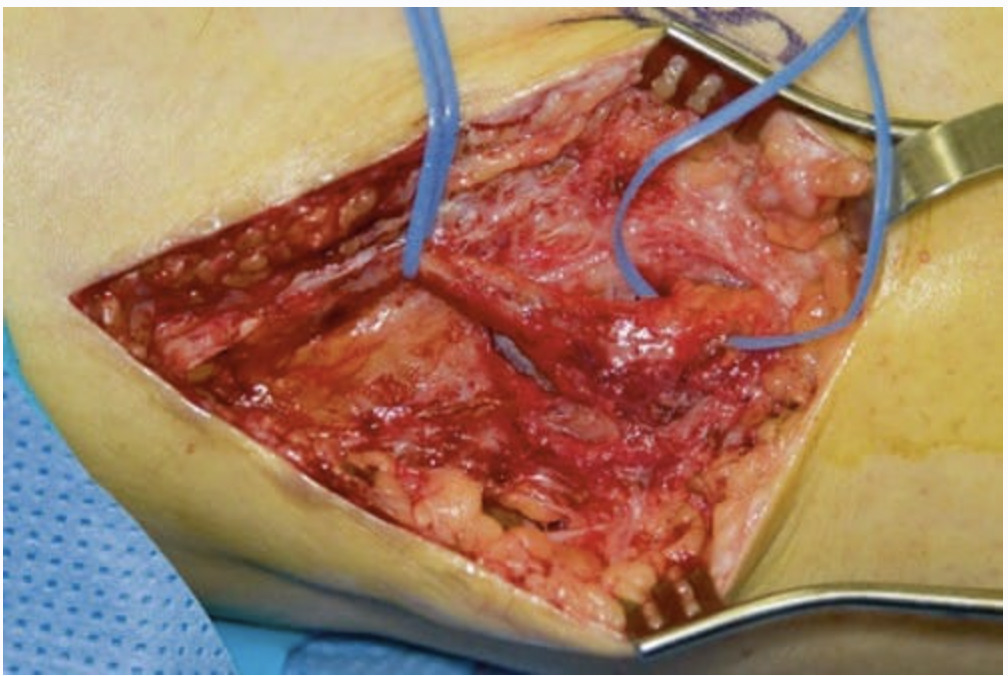
Following this one can continue counting caudally. A linear or a curved transducer may be used, depending on the size of the patient. A longitudinal scan is obtained initially at the midline (spinous process); then by scanning laterally, one can easily see the lamina, and further laterally the facet column will appear in the image as the characteristic “saw sign” (Fig. 3).
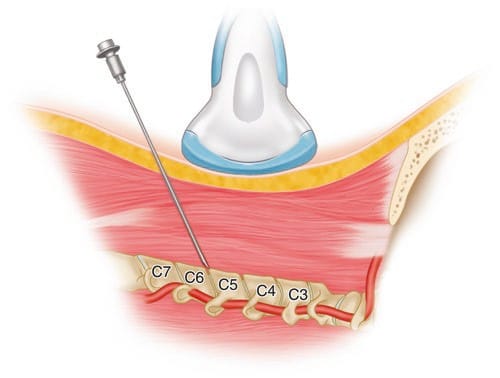
Fig.3 The paramedian position of the ultrasound transducer to obtain a sagittal longitudinal scan through the facet column is shown. The needle is advanced in-plane into the C5–C6 facet joint
If in doubt, one can scan even more laterally until the facet joints are no longer in the image and then come back medially toward them. The inferior articular processes of the level above and the superior articular process of the level below appear as a hyperechoic signals, and the joint space appears as anechoic gap in between (Fig. 4).
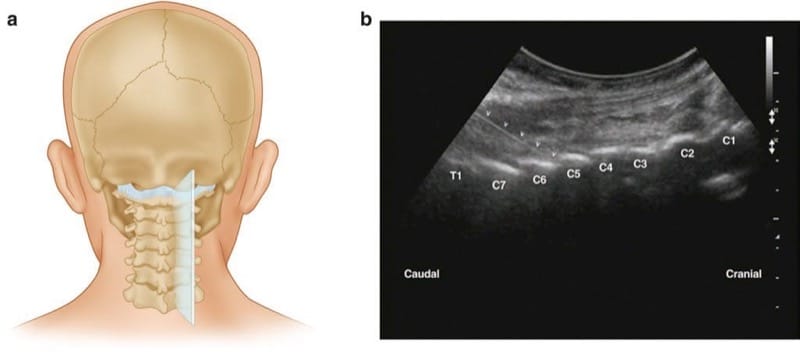
Fig.4 (a) and (b) sagittal longitudinal sonogram showing the articular processes of the facet joints as the “saw sign”
The needle is then inserted inferior to the caudal end of the transducer and advanced from caudad to cephalad—in plane— to enter the caudal end of the joint under real-time ultrasonography (Fig. 5).
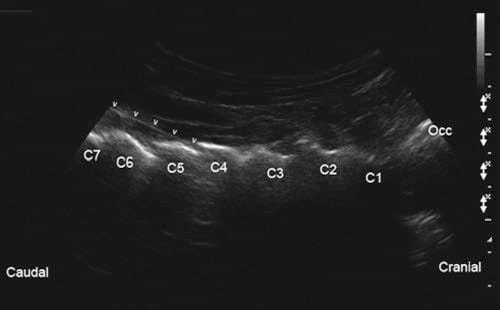
Fig.5 The needle is introduced caudal to the transducer and advanced in-plane into the caudal part of the C4–C5 facet joint (arrowheads). Occ occiput
We believe that this is another advantage of this US approach, as this caudal to cranial direction is matching the caudal angulation of the cervical facet joint, making it easier for the needle to get into the joint space atraumatically [16].