The atlanto-axial joint accounts for up to 16% of patients with occipital headache. In human volunteers, distending the lateral atlanto-axial joint with contrast agent produces occipital pain, and injection of local anesthetic into the joint relieves the headache [1, 2]. The clinical presentation of atlanto-axial joint pain is not specific and therefore cannot be used alone to establish the diagnosis. The only means of establishing a definite diagnosis is a diagnostic block with intra-articular injection of local anesthetic [1]. Intra-articular steroids are effective in short-term relief of pain originating from the lateral atlanto-axial joint [3].
1. ANATOMY OF THE ATLANTO-AXIAL AND ATLANTOOCCIPITAL JOINTS
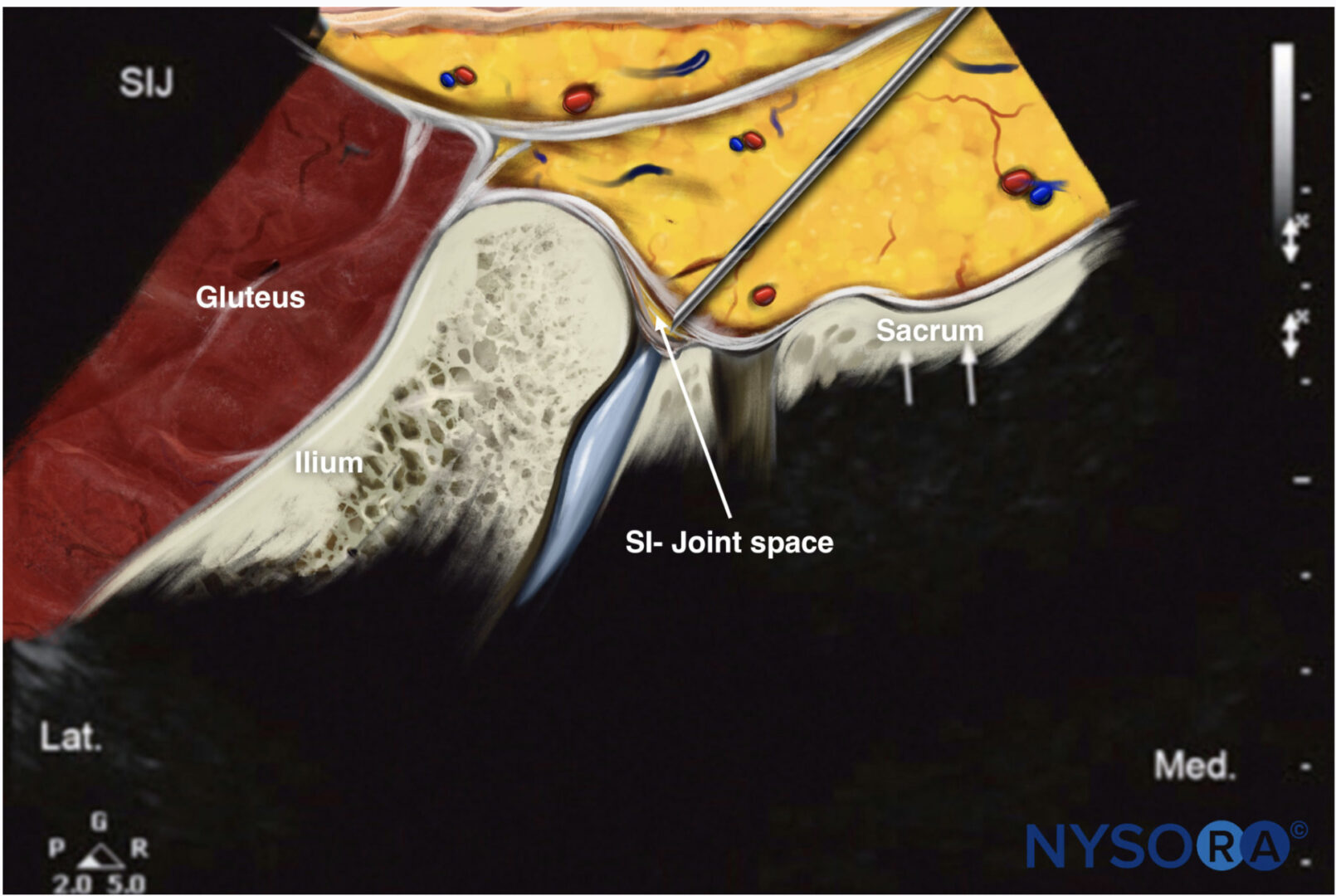
Atlanto-axial and atlanto-occipital joint intra-articular injections have the potential for serious complications, so it is imperative to be familiar with the anatomy of those joints in relation to the surrounding vascular and neural structures. The vertebral artery lies lateral to the atlanto-axial joint as it courses through the C2 and C1 foramina. Then it curves medially to go through the foramen magnum crossing the medial posterior aspect of the atlanto-occipital joint.
The C2 dorsal root ganglion and nerve root with its surrounding dural sleeve cross the posterior aspect of the middle of the joint. Therefore, during atlanto-axial joint injection, the needle should be directed toward the posterolateral aspect of the joint. This will avoid injury to the C2 nerve root medially or the vertebral artery laterally. On the other hand, the atlanto-occipital joint should be accessed from the most superior posterior lateral aspect to avoid the vertebral artery medially. Meticulous attention should be paid to avoid intravascular injection as the anatomy may be variable. Inadvertent puncture of the C2 dural sleeve with CSF leak or high spinal spread of the local anesthetic may occur with atlanto-axial joint injection if the needle is directed only a few millimeters medially [4].
Ultrasound allows visualization of soft tissues, nerves, and vessels (abnormal anatomy), which has the potential to improve the safety of atlanto-axial and atlanto-occipital joint injections by decreasing the incidence or by avoiding injury of nearby structures [5]
2. ULTRASOUND-GUIDED ATLANTO-AXIAL AND ATLANTO-OCCIPITAL JOINT INJECTION TECHNIQUE
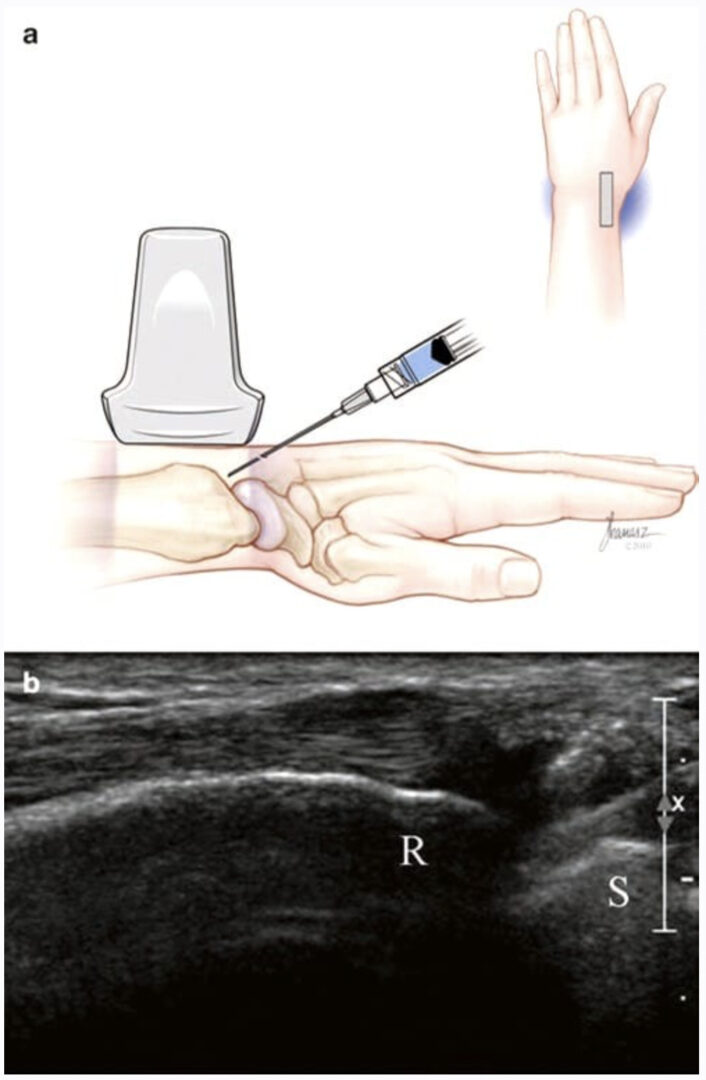
The procedure is performed with the patient in the prone position, using a high-frequency ultrasound transducer (low-frequency transducer may be used depending on body habitus). A transverse short-axis view is obtained by applying the transducer in the midline over the occiput and then scanning caudally to identify C1–C2 level. C1 lacks a spinous process, and the first bifid spinous process encountered is C2.
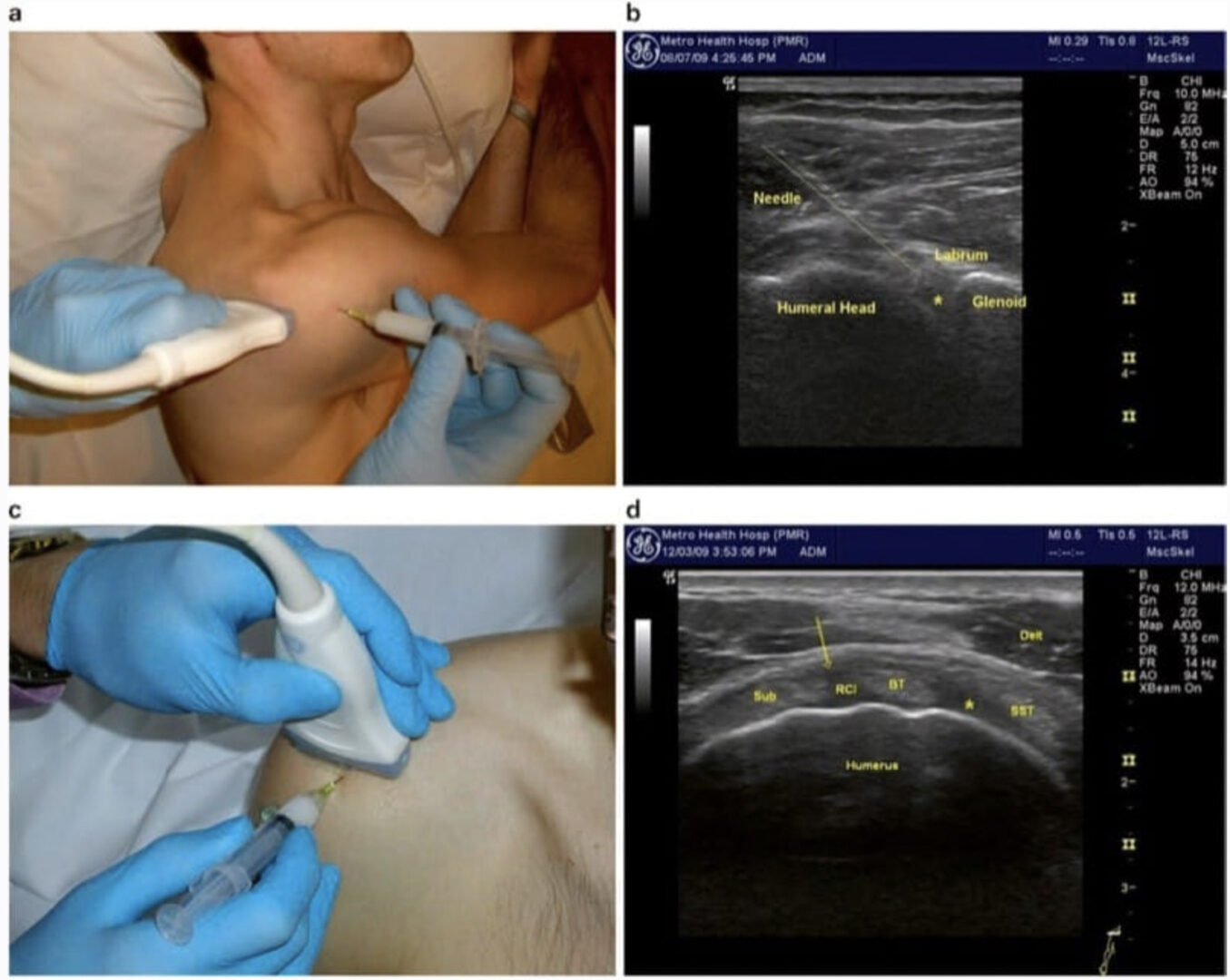
Then the transducer is moved laterally till the C2 nerve root and dorsal root ganglion (DRG) are seen; more laterally the C1–C2 joint (AA joint) appears in the image between the C2 DRG medially and the vertebral artery laterally (Figs. 1, 2, and 3). The transducer is adjusted so that the AA joint is in the middle of the picture, and a 22-gauge blunt tip needle is advanced usually out-of-plane under real-time ultrasound guidance to target the AA joint just medial to the vertebral artery (Fig. 4). The transducer is then shifted to obtain a longitudinal scan at the C1–C2 joint, and the needle tip may need to be adjusted slightly to enter the joint cavity under vision [6].
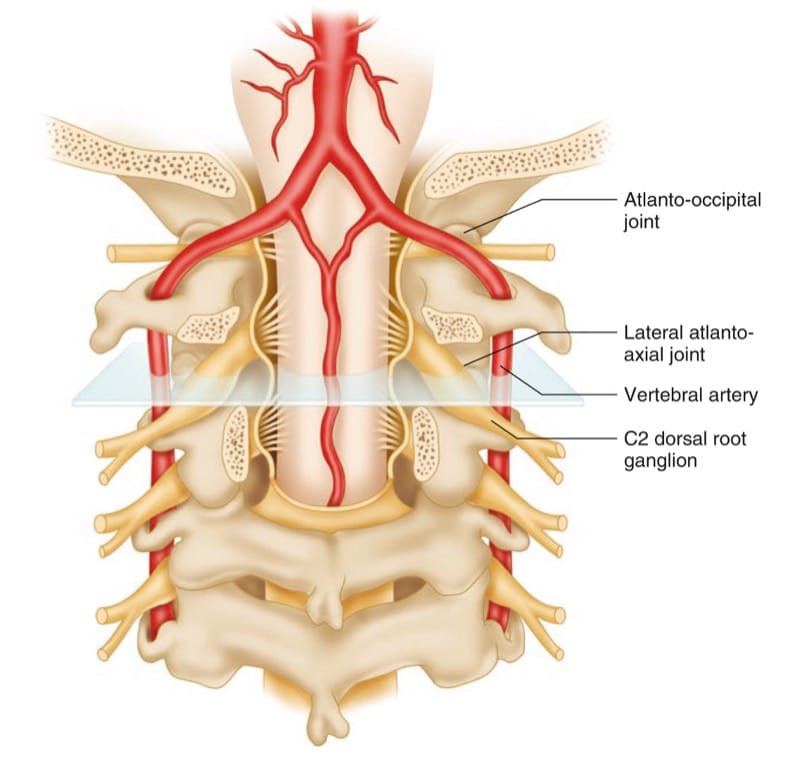
Fig.1 Illustration showing the ultrasound transducer in the transverse plane over the atlanto-axial joint to obtain a short-axis view. (Reprinted with permission from Cleveland Clinic)
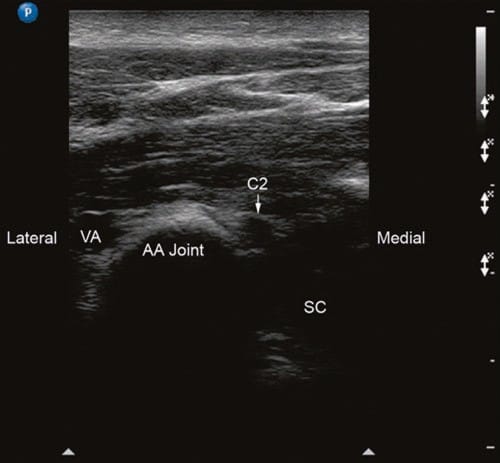
Fig.2 Short-axis sonogram at the level of AA joint. VA vertebral artery, C2 C2 nerve root, DRG C2 dorsal root ganglion, AA joint atlanto-axial joint, SC spinal cord. (Reprinted with permission from Ohio Pain and Headache Institute)
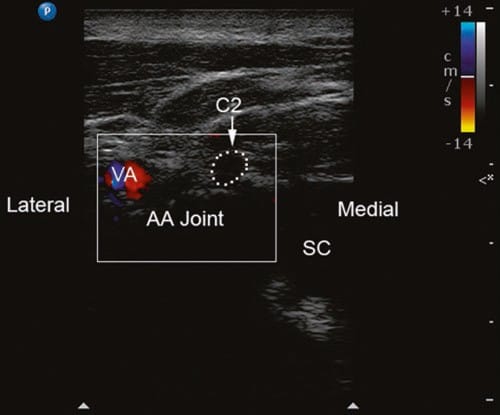
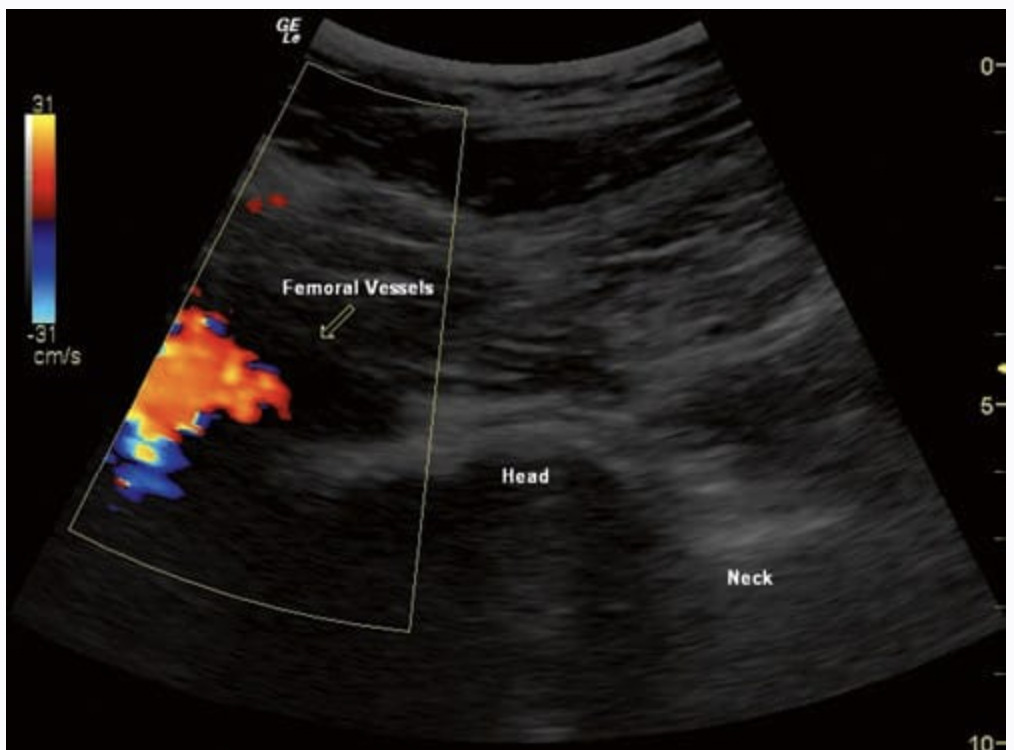
Fig.3 Short-axis sonogram with Doppler to show the vertebral artery (VA) just lateral to the atlanto-axial joint (AA joint). C2 C2 nerve root, DRG C2 dorsal root ganglion, SC spinal cord. (Reprinted with permission from Ohio Pain and Headache Institute)
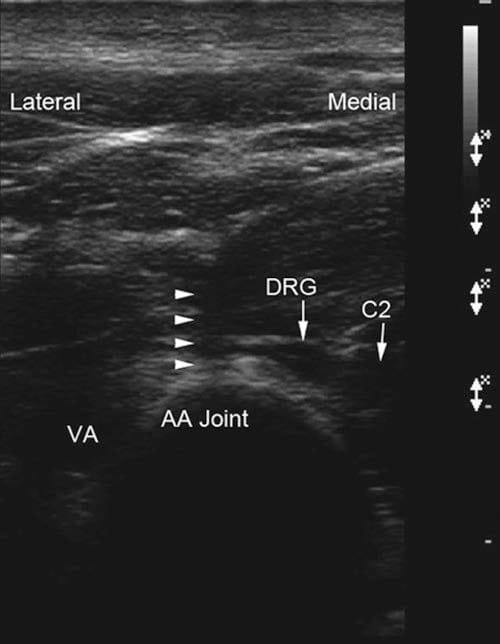
Fig.4 Short-axis sonogram showing the needle (out-of-plane) inside the atlanto-axial joint (arrowheads). VA vertebral artery, C2 C2 nerve root, DRG C2 dorsal root ganglion, AA joint atlanto-axial joint.
(Reprinted with permission from Samer Narouze, MD, PhD (Ohio Institute of Pain and Headache))
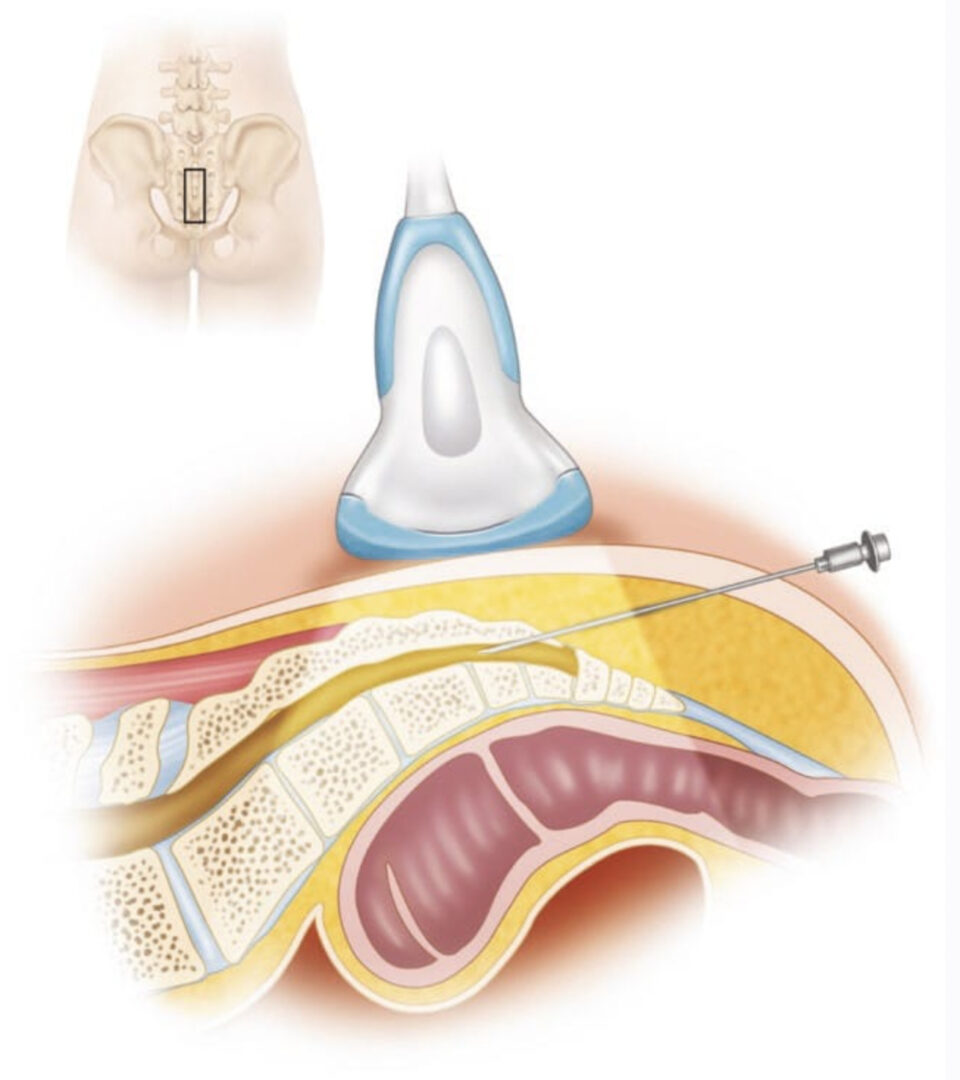
Alternatively, a longitudinal midline scan can be obtained by applying the transducer vertically in the midline over the occiput and cervical spinous processes, and C1– C2 level is identified as above. Then the transducer is moved laterally till the C1–C2 joint (AA joint) appears in the image; slightly laterally one can identify the vertebral artery. The needle is introduced just caudal to the transducer and advanced in-plane under real-time ultrasound guidance to target the AA joint just medial to the vertebral artery (the same approach described for cervical facet intra-articular injection, Chap. 7).
The author prefers the short-axis view (although, it is an out-of-plan approach) as in the same image, one can see the needle advancement – with real-time ultrasonography – into the joint between the C2 DRG medially and the vertebral artery laterally.
To image the atlanto-occipital joint (AO), in the short-axis view, the vertebral artery is followed cranially as it curves medially to enter the foramen magnum. The artery curves posterior and medial to the AO joint, so the joint can be accessed just lateral to the vertebral artery at this point (Fig. 5). However, in some patients the vertebral artery crosses along the whole extent of the posterior aspect of the AO joint from lateral to medial, making it extremely difficult and unsafe to access the joint. If this is the case, the procedure is usually abandoned (Figs. 6 and 7).
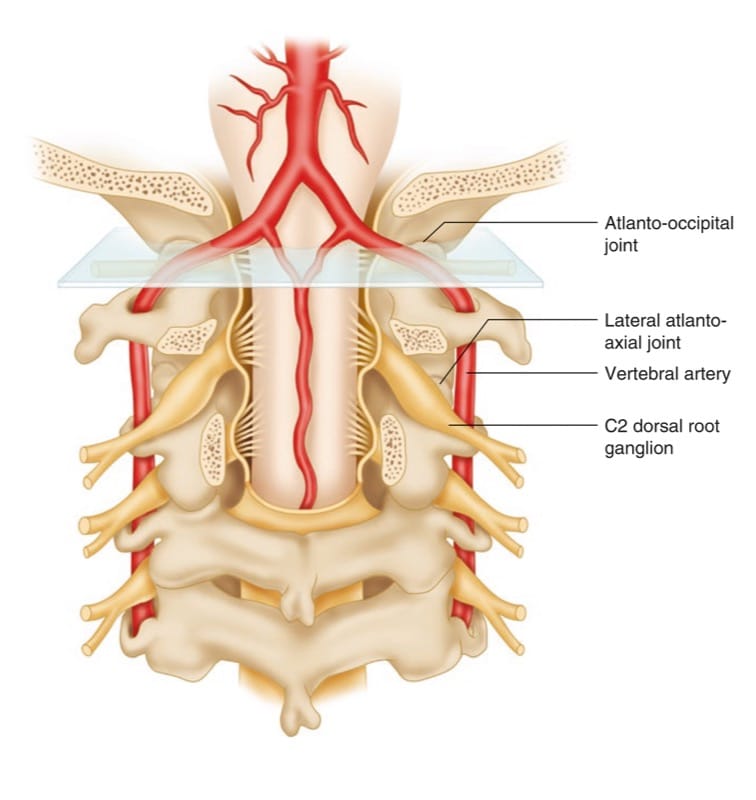
Fig.5 Illustration showing the ultrasound transducer in the transverse plane over the atlanto- occipital joint to obtain a short-axis view. (Reprinted with permission from Cleveland Clinic)
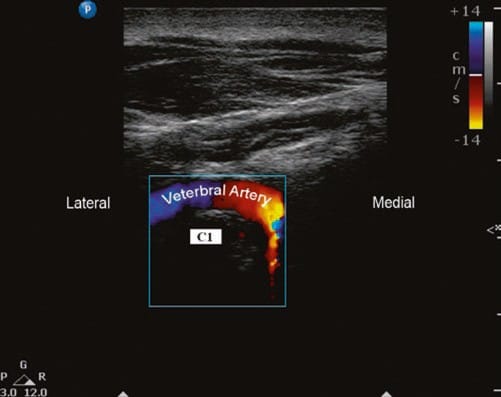
Fig.6 Short-axis sonogram showing the vertebral artery as it crosses medially posterior to the C1 lateral mass in its way to the fora-men magnum. Note the change in the flow direction as the artery curves. (Reprinted with permission from Ohio Pain and Headache Institute)

Fig.7 Long-axis sonogram showing a cross section of the vertebral artery (arrow) as it crosses medially posterior to the C1 lateral mass/atlanto-occipital (AO) joint level. (Reprinted with permission from Ohio Pain and Headache Institute)
3. REFERENCES
1. Aprill C, Axinn MJ, Bogduk N. Occipital headaches stemming from the lateral atlanto-axial (C1-2) joint. Cephalalgia. 2002;22(1):15–22.
2.Busch E, Wilson PR. Atlanto-occipital and atlanto-axial injections in the treatment of headache and neck pain. Reg Anesth. 1989;14(Suppl 2):45.
3. Narouze SN, Casanova J, Mekhail N. The longitudinal effectiveness of lateral atlanto-axial intraarticular steroid injection in the management of cervicogenic headache. Pain Med. 2007;8:184–8.
4. Narouze S. Complications of head and neck procedures. Tech Reg Anesth Pain Manag. 2007;11:171–7.
5. Narouze S. Ultrasonography in pain medicine: future directions. Tech Reg Anesth Pain Manag. 2009;13:198–202.
6. Narouze S. Ultrasound-guided lateral atlanto-axial joint injection for the treatment of cervicogenic headache (abstract). Pain Med. 2009;10:222.