Explore NYSORA knowledge base for free:

The rise in ambulatory surgeries worldwide has transformed the landscape of perioperative care. With millions of outpatient procedures performed annually—ranging from 16 to 20 million in the United States alone—there is a pressing need for structured, safe, and efficient perioperative management strategies. Enhanced Recovery After Surgery (ERAS) programs, originally developed for inpatient surgical care, are now being adapted to the outpatient setting, offering promising results in terms of patient outcomes, cost-effectiveness, and healthcare resource utilization. This comprehensive article explores the core pillars, recent advancements, and implementation strategies of ERAS in ambulatory anesthesia, emphasizing the pivotal role anesthesiologists play in driving patient-centered care across all perioperative phases. Why ambulatory surgery demands enhanced recovery protocols Ambulatory surgical centers (ASCs) have expanded rapidly due to: Advancements in minimally invasive surgical techniques. Improvements in anesthesia safety and efficiency. A growing focus on cost-effectiveness and value-based care. Positive outcomes demonstrated in same-day discharge protocols for procedures like mastectomy and joint arthroplasty. Despite reduced hospital resource use, ambulatory procedures carry risks of complications such as postoperative nausea and vomiting (PONV), pain mismanagement, delayed recovery, and readmission. ERAS protocols offer structured, evidence-based solutions that anticipate and mitigate these risks by optimizing care before, during, and after surgery. Core pillars of enhanced recovery in ambulatory anesthesia ERAS protocols for outpatient procedures are designed around five core principles: Preoperative optimization and education Multimodal analgesia and PONV prevention Fluid management and normothermia Early nutrition and mobilization Opioid-sparing pain control These components work synergistically to limit the physiological stress of surgery, support functional recovery, and enable same-day discharge. Below, we break down each element and explore the latest findings supporting its use in outpatient settings. Preoperative care: setting the stage for success Patient education and psychological preparation Early counseling reduces anxiety and aligns expectations. Interventions such as preoperative visits and surgical […]
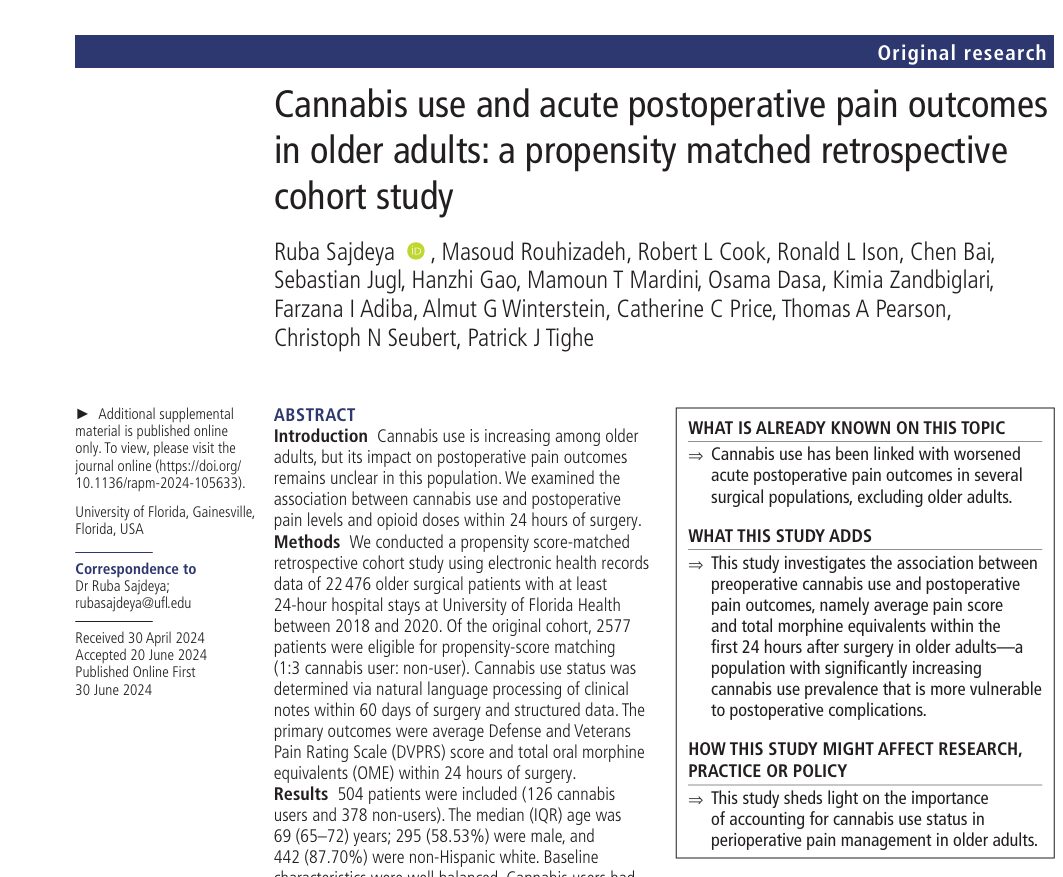
Understanding cannabis’s impact on surgery recovery Cannabis use is increasingly common among older adults, often for medical reasons like chronic pain. But how does this trend affect postoperative recovery? A new study from the University of Florida sheds light on this pressing question, showing that cannabis use is linked to worse pain outcomes and increased opioid requirements after surgery. Key findings at a glance Study type: Propensity-matched retrospective cohort study Population: 504 patients aged ≥65 years undergoing major inpatient surgery Exposure: Cannabis use within 60 days prior to surgery Outcomes: Higher average postoperative pain scores (DVPRS) Increased total oral morphine equivalents (OME) Timeframe assessed: First 24 hours after surgery What the study found Increased pain and opioid needs Compared to non-users, cannabis users experienced significantly more pain and required higher doses of opioids: Pain score (DVPRS): Cannabis users: 4.68 (IQR: 2.71–5.96) Non-users: 3.88 (IQR: 2.33–5.17) Median difference: 0.80 (p=0.01) Opioid use (OME): Cannabis users: 42.50 mg (IQR: 15.00–60.00) Non-users: 30.00 mg (IQR: 7.50–60.00) Median difference: 12.5 mg (p=0.02) On average, cannabis users were 58% to 71% more likely to experience moderate-to-severe pain than non-users, even after adjusting for opioid dosage. Clinical and policy implications What this means for healthcare Pain management should be personalized for older adults with a cannabis use history. Preoperative screening for cannabis use should become routine. Providers should anticipate the potential need for higher opioid dosages or multimodal analgesia strategies. The ASRA-PM (American Society of Regional Anesthesia and Pain Medicine) guidelines recommend multimodal approaches for cannabis users, reserving opioids as rescue therapy. Conclusion This landmark study adds to a growing body of evidence suggesting that cannabis use before surgery may lead to higher postoperative pain and opioid requirements, especially in older adults. Reference: Sajdeya R et al. Cannabis use and acute postoperative pain outcomes in older […]

The BRUGANAES study, recently published in the European Journal of Anaesthesiology (2025), provides valuable insights into the anesthetic management of patients with Brugada syndrome (BrS), a rare but potentially lethal cardiac condition. BrS poses unique perioperative challenges, especially given the long-standing concern that standard anesthetic drugs might trigger malignant arrhythmias. The BRUGANAES study challenges this assumption with data spanning 18 years and involving 189 anesthetic procedures. What is Brugada syndrome? Brugada syndrome is a genetic channelopathy associated with sudden cardiac death due to life-threatening ventricular tachyarrhythmias. It’s characterized by: Abnormal ECG findings (notably, type 1 coved ST elevation in right precordial leads) Mutations, particularly in the SCN5A gene, affecting cardiac sodium channels Symptoms such as syncope, seizures, or nocturnal agonal breathing Increased risk during fever, bradycardia, electrolyte imbalances, or under certain drugs (e.g., local anesthetics, propofol) Study overview: BRUGANAES Objective: To assess the incidence of malignant arrhythmias during and up to 30 days post-anesthesia in BrS patients. Design: Retrospective cohort (2006–2023) Conducted at Hospital Clínic of Barcelona Included 111 patients undergoing 189 procedures Primary outcome: Occurrence of malignant ventricular arrhythmias or sudden cardiac death (SCD) Secondary outcomes: Hospital complications 30-day readmissions 30-day mortality Key findings Only 2 procedures (1%) led to intraoperative malignant arrhythmias No post-operative arrhythmias or deaths were reported within 30 days 129 (68.3%) procedures used non-recommended drugs like propofol, ketamine, or local anesthetics Propofol was used in 50.3% of all procedures No arrhythmias occurred in patients receiving neuraxial or peripheral blocks Anesthetic approaches in BrS Drug classifications Non-recommended drugs: Propofol, ketamine, tramadol, and local anesthetics Recommended drugs: Opioids, inhalational anesthetics, thiopental, etomidate Types of anesthesia used: General anesthesia: 45.5% Procedural sedation: 31.2% Regional/neuraxial alone: 12.7% Mixed techniques: 10.6% Regional anesthesia details: Drugs used: Bupivacaine (36.4%) Levobupivacaine (22.7%) Mepivacaine (20.9%) Ropivacaine (13.9%) No associated malignant arrhythmias despite sodium […]