Explore NYSORA knowledge base for free:

Perioperative pulmonary complications are among the most frequent causes of morbidity and extended hospital stays following surgery. With the advent of point-of-care ultrasound (POCUS), clinicians now have an accessible, noninvasive, and highly sensitive tool to assess lung aeration dynamically. What is lung ultrasound and why is it important? Lung ultrasound is a bedside imaging technique used to assess lung aeration and detect pathological changes in the lungs. Unlike static imaging modalities such as chest X-ray or CT scans, lung ultrasound provides real-time visualization of lung dynamics, making it an ideal tool during and after surgical procedures. Why it’s gaining traction Diagnostic accuracy: Detects pneumothorax, pleural effusion, pulmonary edema, and atelectasis more sensitively than X-rays. Accessibility: Portable, affordable devices that connect to tablets and smartphones. Safety: No radiation exposure. Usability: Easy integration into standard perioperative protocols. During the COVID-19 pandemic, LUS proved vital in the bedside assessment of lung conditions, reinforcing its relevance in routine and emergency care settings. Ultrasound techniques and transducer types Transducer orientation Longitudinal (sagittal) orientation: Marker faces cephalad; visualizes intercostal muscles and pleura. Transverse (axial) orientation: Rotated 90°; enhances detection of subtle atelectasis and extends pleural visibility. Transducer selection Linear (high-frequency): Superior resolution for pleural line and lung sliding. Curvilinear or phased-array (low-frequency): Better for deep structures and B-lines; phased array is ideal for intercostal spaces. Interpreting lung ultrasound: What does normal vs. abnormal look like? Normal findings Lung sliding: A shimmering of the pleural line as visceral and parietal pleura move during respiration. A-lines: Horizontal reverberation artifacts; signify well-aerated lung tissue. Lung pulse: Rhythmic motion synchronized with the heart; excludes pneumothorax. Indicators of impaired aeration B-lines: Vertical, laser-like artifacts indicating interstitial syndrome or fluid. Subpleural consolidations: Small focal areas of collapse beneath the pleural line. Dense consolidations: “Lung hepatization” – lung tissue resembling liver in echotexture […]
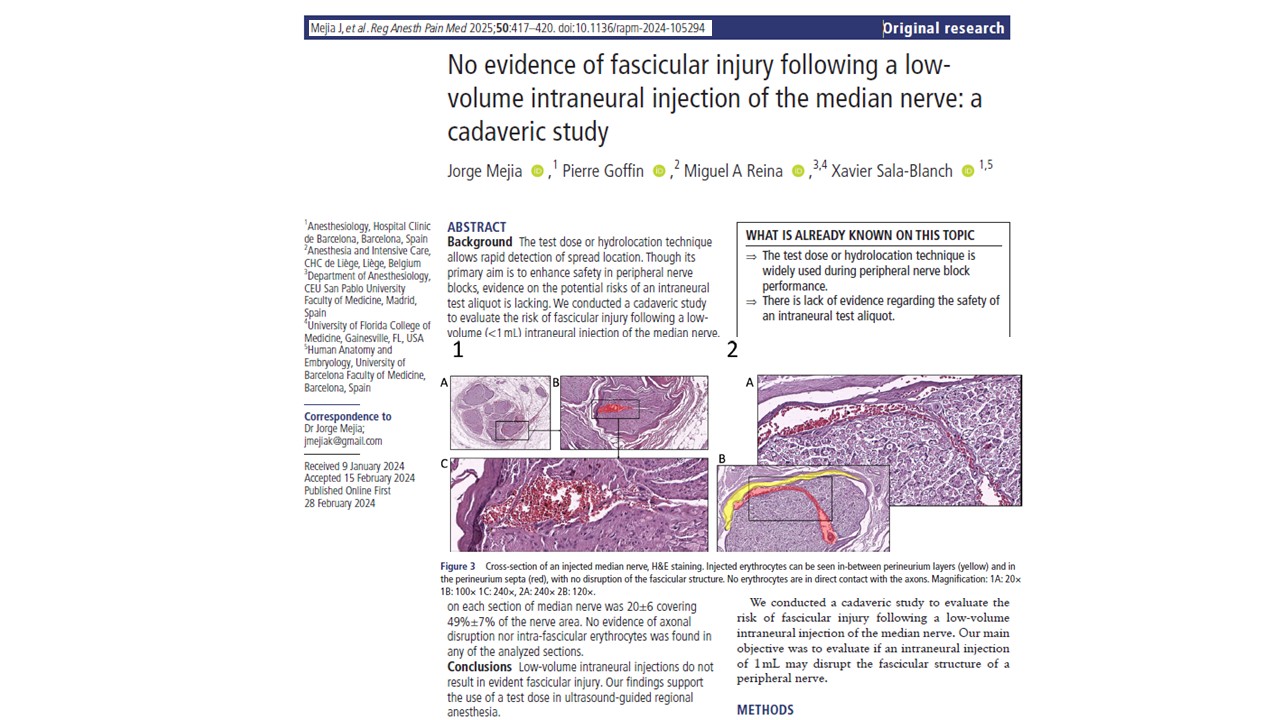
A recent cadaver-based investigation by Mejia et al. 2025, published in RAPM, provides new insights into the structural effects of low-volume intraneural injections in regional anesthesia. The study investigated whether administering a small volume of fluid, 1 mL, into the median nerve resulted in any fascicular damage. Despite longstanding concerns that intraneural injections can cause nerve injury, the study’s findings suggest that under controlled conditions, low-volume intraneural injections do not result in structural disruption of the nerve fascicles. Background and rationale Peripheral nerve blocks (PNBs) are widely used in anesthetic practice for intraoperative and postoperative analgesia. Ultrasound guidance has improved the precision of these blocks, yet inadvertent intraneural injection remains a concern. Estimates suggest that intraneural needle placement occurs in 15% to 20% of cases using ultrasound guidance. The test dose or hydrolocation technique involves injecting a small aliquot of fluid, typically less than 1 mL, into or around the nerve to confirm needle position. If swelling within the nerve is observed sonographically, the needle can be repositioned before administering a full anesthetic dose. While this method is intended to reduce risk, its safety profile has not been comprehensively evaluated, particularly concerning fascicular integrity. This study was designed to assess whether a 1 mL intraneural injection into the median nerve leads to fascicular injury, using histological methods to detect any signs of perineurium disruption or intrafascicular injectate spread. Study design and methodology The study was conducted using ten fresh, unembalmed human cadaveric upper limbs. These specimens had no history of trauma, surgery, or neurological disease. The limbs were thawed and brought to room temperature before the procedures. Step-by-step procedure Ultrasound identification: The median nerve was located in the forearm using a 6–13 MHz linear ultrasound transducer. The nerve was visualized between the deep and superficial flexor muscles. Injection protocol: A […]

As global health systems increasingly grapple with their environmental impact, the operating room has emerged as a key area for sustainable reform. One of the largest contributors to hospital emissions is the administration of general anesthesia (GA). A new study published in the British Journal of Anaesthesia (2025) by Bernat et al. provides critical new evidence on how different anesthetic techniques compare in terms of greenhouse gas (GHG) emissions and overall ecological footprint. Why this study matters Healthcare globally is responsible for a substantial proportion of GHG emissions. If it were a country, the healthcare sector would be the fifth-largest emitter in the world. Operating rooms are especially resource-intensive, with anesthetic gases accounting for up to 40% of surgical emissions. This study by Bernat et al. stands out due to its real-world, multicentre scope, analyzing over 35,000 adult surgeries across three major French hospitals. It’s the most comprehensive comparison to date of: Total intravenous anesthesia (TIVA) using propofol Target-controlled inhalation anesthesia (TCIA) using sevoflurane Manually optimised sevoflurane anesthesia Overview of anesthetic techniques 1. Total intravenous anesthesia (TIVA) Administered exclusively via IV using propofol Avoids the use of volatile gases 2. Target-controlled inhalation anesthesia (TCIA) Uses automated systems to deliver sevoflurane at ultra-low fresh gas flows (~0.5–0.8 L/min) 3. Manually optimised sevoflurane Inhalation anesthesia is managed manually by anesthetists using protocols to minimize gas waste Key findings: GHG emissions per hour These results show that TIVA with propofol produces 8 to 10 times fewer carbon emissions per hour than either form of sevoflurane-based inhalation anesthesia. Environmental impacts beyond carbon emissions While CO₂ emissions are the main metric, other pollutants were considered: Plastic waste per procedure TIVA: 72 g TCIA: 18 g Manual Sevoflurane: 27 g Aluminium waste per procedure Only in strategies using sevoflurane in aluminium bottles (TIVA group): 0.09 […]