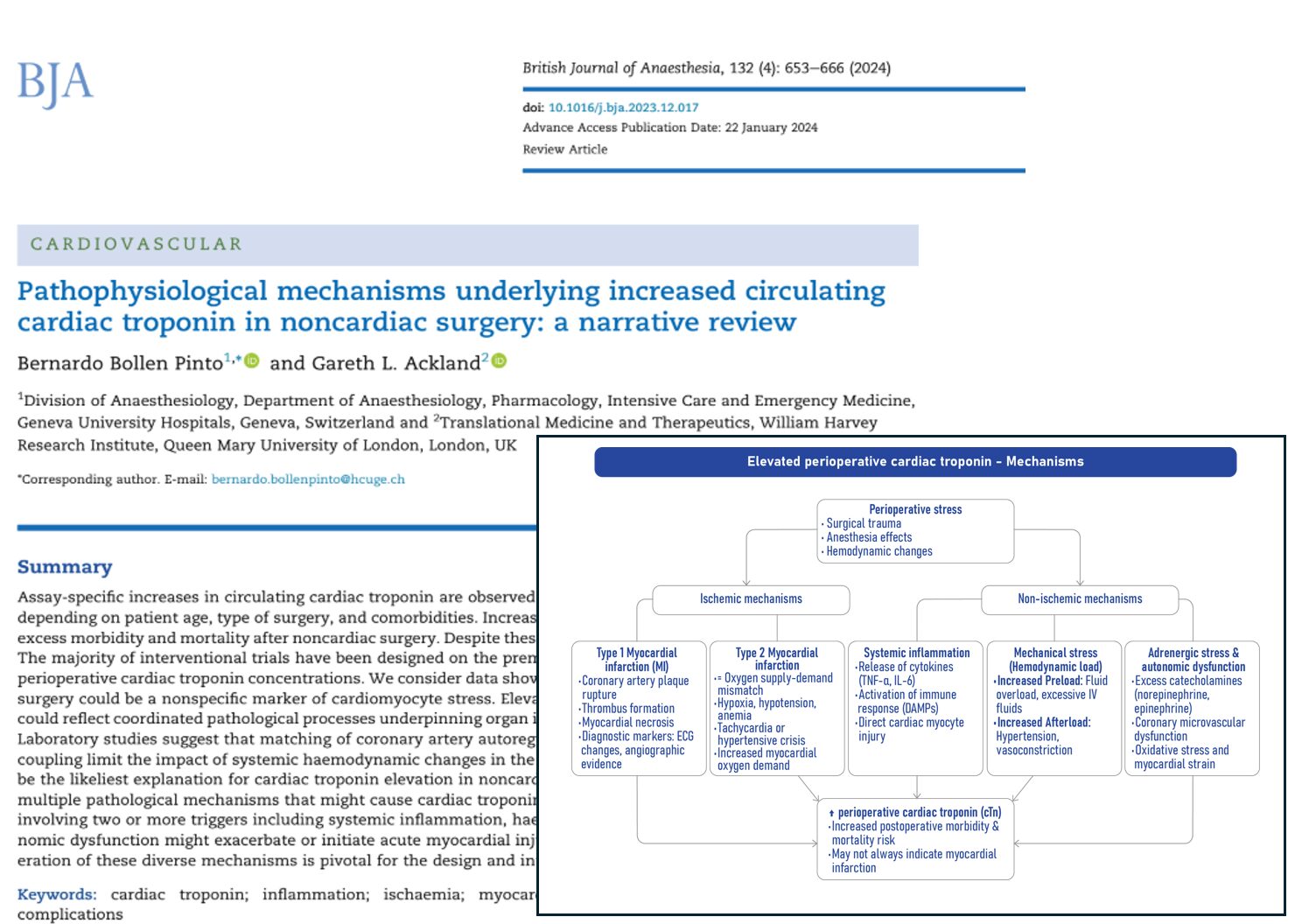
The detection of elevated cardiac troponin (cTn) levels following noncardiac surgery is a common and concerning clinical finding. As reported in the British Journal of Anaesthesia by Bollen Pinto and Ackland (2024), 20–40% of surgical patients exhibit increased cTn levels postoperatively, a biomarker traditionally associated with myocardial injury. However, the mechanisms behind this rise are multifaceted and not necessarily linked to classic cardiac ischemia.
What is cardiac troponin and why does it matter?
Cardiac troponins I (cTnI) and T (cTnT) are structural proteins that regulate cardiac muscle contraction. When heart muscle cells (cardiomyocytes) are injured, troponin is released into the bloodstream. High-sensitivity cardiac troponin (hs-cTn) assays can detect even minute levels, identifying cardiac stress or injury well before clinical symptoms appear.
- Key functions: Regulate calcium-mediated interactions during myocardial contraction and relaxation.
- Diagnostic role: Elevations > 99th percentile upper reference limit (URL) suggest myocardial injury.
- Assay sensitivity: Current hs-cTn assays can detect release from as little as 40 mg of myocardial tissue.
Scope of the problem: How common is troponin elevation after surgery?
More than 300 million surgeries are performed annually worldwide. Troponin elevations occur in:
- 20–40% of patients post-noncardiac surgery.
- Up to 73% in high-risk populations, or depending on assay sensitivity.
These elevations are significantly associated with:
- 8.1% in-hospital mortality, compared to 0.4% in patients without elevated cTn.
- 20.6% 1-year mortality, versus 5.1% in patients without cTn increases.
- Greater rates of postoperative complications, disability, and major adverse cardiovascular events (MACE).
The misperception: troponin equals infarction?
While elevated cTn levels typically trigger alarms for myocardial infarction (MI), the perioperative setting introduces complexity. The Fourth Universal Definition of MI requires:
- Clinical evidence of ischaemia.
- ECG changes.
- Imaging confirmation of new myocardial injury.
Yet:
- 80–90% of patients with postoperative myocardial injury lack chest pain or ECG changes.
- Only 15–25% of postoperative myocardial infarctions involve acute coronary occlusion.
This suggests that most troponin elevations post-surgery are not due to classical heart attacks, and alternate mechanisms must be considered.
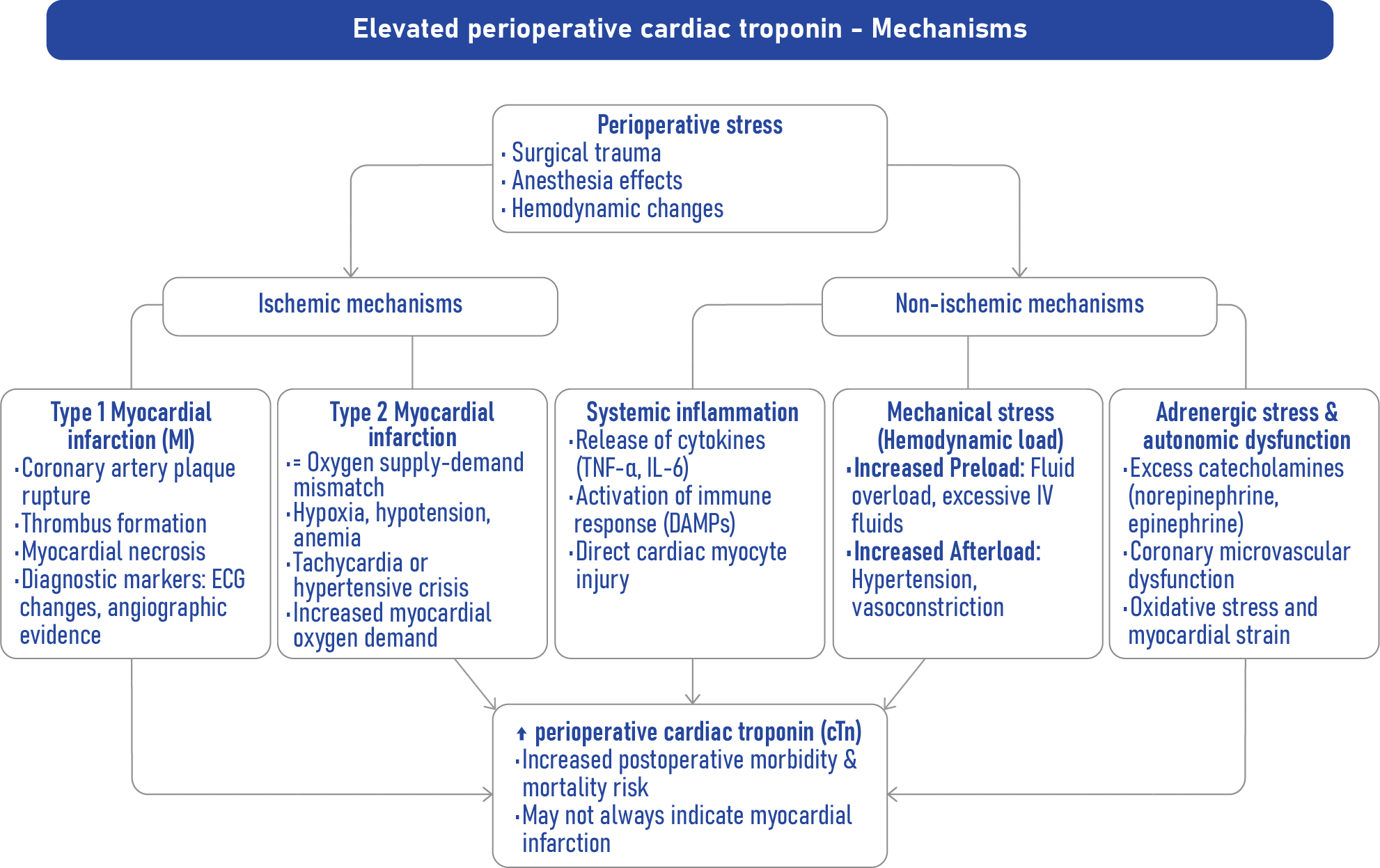
Pathophysiological mechanisms behind troponin elevation
-
Systemic inflammation
Surgical trauma releases danger-associated molecular patterns (DAMPs) that trigger widespread inflammation. These molecules:
- Interact with toll-like receptors (TLRs) on cardiomyocytes.
- Cause mitochondrial dysfunction, decreased contractility, and direct injury.
- Promote the release of troponin without ischemia or necrosis.
-
Hemodynamic strain
Perioperative hypotension, tachycardia, or hypertension can alter coronary blood flow and stress the myocardium.
- Hypotension: Reduces perfusion pressure; may exceed autoregulatory capacity.
- Tachycardia: Shortens diastole, limiting myocardial perfusion.
- Hypertension: Increases myocardial oxygen demand via elevated afterload.
-
Autonomic dysfunction
Aging, diabetes, and cardiovascular comorbidities impair autonomic regulation. Resulting vagal withdrawal:
- Reduces coronary perfusion efficiency.
- Increases heart rate and myocardial oxygen demand.
- Disrupts immune modulation, potentially exacerbating inflammation.
-
Adrenergic stress
Catecholamines surge in response to surgery and pain, increasing:
- Myocardial oxygen demand.
- Risk of coronary vasospasm or microthrombi.
- Direct cellular toxicity via calcium overload and oxidative stress.
How troponin reaches circulation: cellular mechanisms
a. Necrosis
Classical form of cell death due to prolonged ischaemia. Membrane rupture allows full troponin complexes to enter the bloodstream.
b. Apoptosis and secondary necrosis
Regulated, non-inflammatory cell death. Incomplete clearance may lead to:
- Troponin leakage.
- Small fragment release.
- Systemic inflammation.
c. Intracellular proteolysis
Activated proteases (e.g., calpains) degrade troponin into fragments < 1 kDa, which can:
- Pass through intact membranes.
- Be detected by assays even without cell death.
d. Gap junction alterations (Connexin 43)
Inflammation alters gap junction distribution and function, promoting:
- Unregulated molecule passage.
- Loss of ionic control.
- Direct troponin escape via hemichannels.
e. Extracellular vesicle secretion
Cardiomyocytes may actively secrete troponin in lipid vesicles. Stress or catecholamines increase vesicle release.
Not all troponin elevations signal harm
Studies show:
- 71% of children had elevated cTn after casual football play.
- 28% of healthy adults showed cTn rise after minor orthopedic surgery, without complications.
- Marathon runners exhibit transient cTn increases composed solely of small fragments.
These findings reinforce that context matters in interpreting troponin results.
Diagnostic challenges: why we need better tools
Current assays:
- Detect all cTn forms indiscriminately.
- Cannot differentiate between ischaemic and non-ischaemic injury.
- Are influenced by age, sex, race, and renal function.
Future directions include:
- Fragment-specific assays: Distinguishing intact vs. degraded troponin.
- Molecular fingerprinting: Identifying inflammatory vs. necrotic release patterns.
- Multimodal biomarkers: Incorporating inflammatory cytokines, microRNAs, and metabolic stress markers.
Conclusion
Troponin elevation in the aftermath of noncardiac surgery represents a complex, multifactorial phenomenon that stretches beyond the confines of classical ischemia. Bollen Pinto and Ackland’s review challenges clinicians to rethink the diagnostic framework and encourages the development of refined biomarkers and personalized management strategies.
Ultimately, understanding why troponin rises and what it means is essential for improving postoperative outcomes and avoiding both overtreatment and missed opportunities for intervention.
Reference: Bollen Pinto B et al. Pathophysiological mechanisms underlying increased circulating cardiac troponin in noncardiac surgery: a narrative review. Br J Anaesth. 2024;132:653-666.
Read more about this topic in NYSORA’s Anesthesia Updates.