As surgical volumes increase globally, the importance of managing patients’ psychological well-being is coming into sharper focus. Mental health disorders, particularly depression and anxiety, are increasingly prevalent and carry significant implications for perioperative outcomes. According to a 2024 review by Rolfzen et al., integrating mental health care into surgical workflows can lead to better pain management, faster recovery, and reduced mortality.
The silent burden of mental illness in surgery
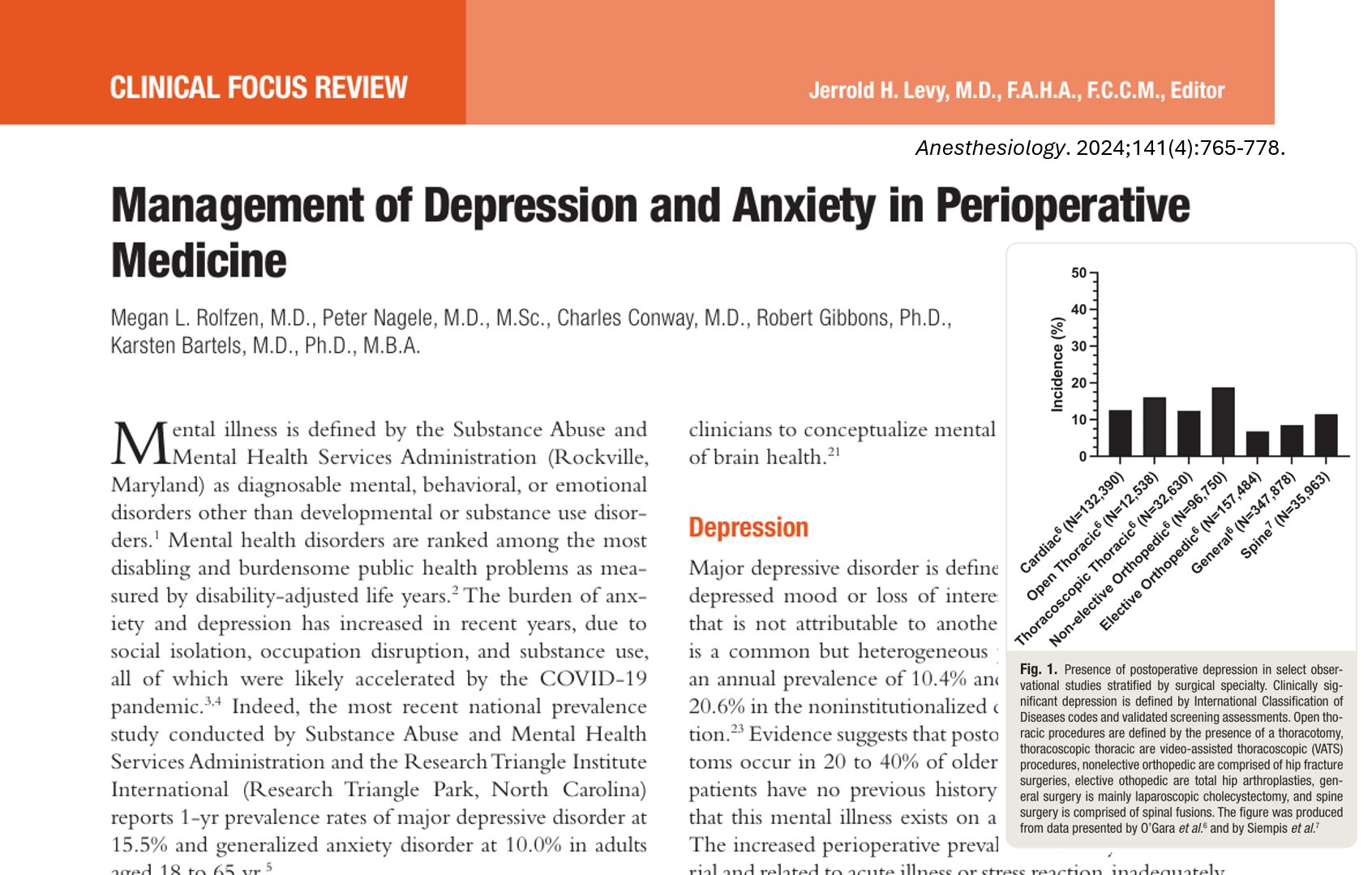
Mental illness is a major contributor to global disability. In the U.S., the prevalence of major depressive disorder and generalized anxiety disorder in adults aged 18–65 stands at 15.5% and 10%, respectively. Yet, the burden is even higher among surgical patients due to stressors related to surgery, including pain, hospitalization, and uncertainty.
Key implications of untreated perioperative mental illness:
- Increased postoperative pain
- Higher hospital readmission rates
- Elevated risk of postoperative delirium
- Reduced quality of life and prolonged recovery
- Increased 30-day postoperative mortality
Despite these risks, only 47.2% of patients with a diagnosed mental illness receive any treatment.
Preoperative considerations: screening and risk assessment
Mental health screening tools for surgical patients:
- PHQ-9 / PHQ-2: Quick assessments for depression severity
- GAD-7 / GAD-2: Widely used for anxiety detection
- Amsterdam Preoperative Anxiety and Information Scale: Tailored for surgical patients
- Computerized Adaptive Tests: AI-driven tools for personalized assessment
Digital innovation: Adaptive computerized tools enable rapid screening (3–5 minutes) and can be embedded in electronic health records to prompt early intervention.
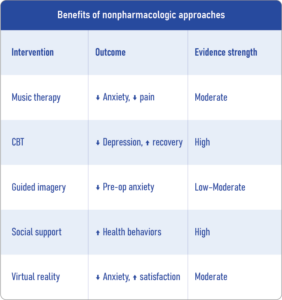
Nonpharmacologic interventions
Behavioral therapies are essential in managing preoperative and postoperative psychological distress. These include:
- Cognitive Behavioral Therapy (CBT): Four short sessions can significantly reduce depressive and anxiety symptoms in cardiac surgery patients.
- Group psychotherapy: Eight weekly sessions cut depression and anxiety by over 60% in lung cancer patients.
- Music medicine: Passive music listening reduces anxiety and improves satisfaction in diverse surgical populations.
- Mindfulness and guided imagery: Improve coping and pain perception.
- Virtual reality: Effective for reducing anxiety through distraction and education.
- Social support: Lack of strong social ties doubles the risk of perioperative depression.
Pharmacologic considerations
-
Continuing existing antidepressants
- Recommended unless contraindicated (e.g., NPO status).
- Sudden cessation can cause withdrawal or relapse.
- Coordinate with psychiatry and pharmacy teams.
-
Potential risks
- Serotonin syndrome: Caution with combining serotonergic drugs and anesthetics.
- Increased bleeding risk: Especially with SSRIs during major surgeries like mastectomy.
-
Rapid-acting agents
- Ketamine (IV): Rapid onset antidepressant, effective in treatment-resistant cases.
- Esketamine (nasal): FDA-approved for treatment-resistant depression.
- Nitrous oxide: Promising antidepressant properties with fewer side effects than ketamine.
Note: These agents are not yet standard perioperative treatments and require more research.
Managing perioperative mental health
-
Preoperative phase
- Use brief screening tools (e.g., PHQ-2, GAD-2)
- Educate patients on what to expect during recovery
- Offer CBT, music therapy, or guided imagery
- Involve family for emotional support
-
Intraoperative phase
- Continue existing medications when possible
- Coordinate care with psychiatry if complex
- Avoid serotonin-increasing anesthetics if the patient is on SSRIs
-
Postoperative phase
- Reassess mental status using brief tools
- Provide structured support, possibly via telehealth
- Consider ketamine/nitrous oxide for severe depression (research setting)
-
Discharge planning
- Set up mental health follow-up (telemedicine or in-person)
- Provide digital mental health resources (apps, virtual CBT)
- Encourage sustained social engagement
Conclusion
Depression and anxiety are not side issues. They are central to surgical success. Recognizing and addressing these conditions through a multidisciplinary, evidence-informed approach is no longer optional; it’s essential. As we reshape surgical care for the 21st century, integrating mental health could become the most impactful innovation in perioperative medicine.
Reference: Rolfzen ML et al. Management of Depression and Anxiety in Perioperative Medicine. Anesthesiology. 2024;141:765-778.
Read more about this topic in the Anesthesia Updates section of the Anesthesia Manual App. Prefer a physical copy? Get the latest literature and guidelines in book format. For an interactive digital experience, check out the Anesthesia Updates Module on NYSORA360!