The rise in ambulatory surgeries worldwide has transformed the landscape of perioperative care. With millions of outpatient procedures performed annually—ranging from 16 to 20 million in the United States alone—there is a pressing need for structured, safe, and efficient perioperative management strategies. Enhanced Recovery After Surgery (ERAS) programs, originally developed for inpatient surgical care, are now being adapted to the outpatient setting, offering promising results in terms of patient outcomes, cost-effectiveness, and healthcare resource utilization.
This comprehensive article explores the core pillars, recent advancements, and implementation strategies of ERAS in ambulatory anesthesia, emphasizing the pivotal role anesthesiologists play in driving patient-centered care across all perioperative phases.
Why ambulatory surgery demands enhanced recovery protocols
Ambulatory surgical centers (ASCs) have expanded rapidly due to:
- Advancements in minimally invasive surgical techniques.
- Improvements in anesthesia safety and efficiency.
- A growing focus on cost-effectiveness and value-based care.
- Positive outcomes demonstrated in same-day discharge protocols for procedures like mastectomy and joint arthroplasty.
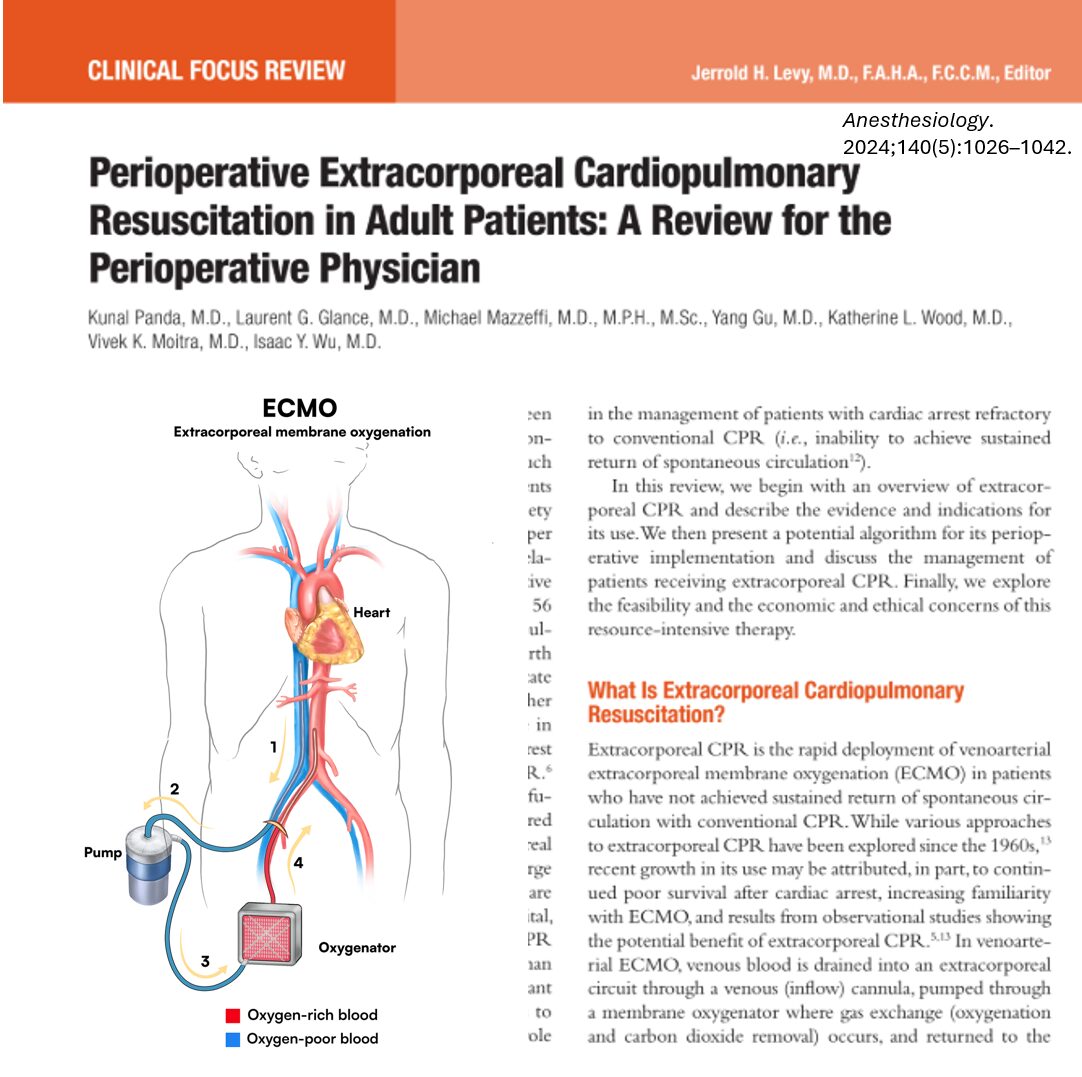
Despite reduced hospital resource use, ambulatory procedures carry risks of complications such as postoperative nausea and vomiting (PONV), pain mismanagement, delayed recovery, and readmission. ERAS protocols offer structured, evidence-based solutions that anticipate and mitigate these risks by optimizing care before, during, and after surgery.
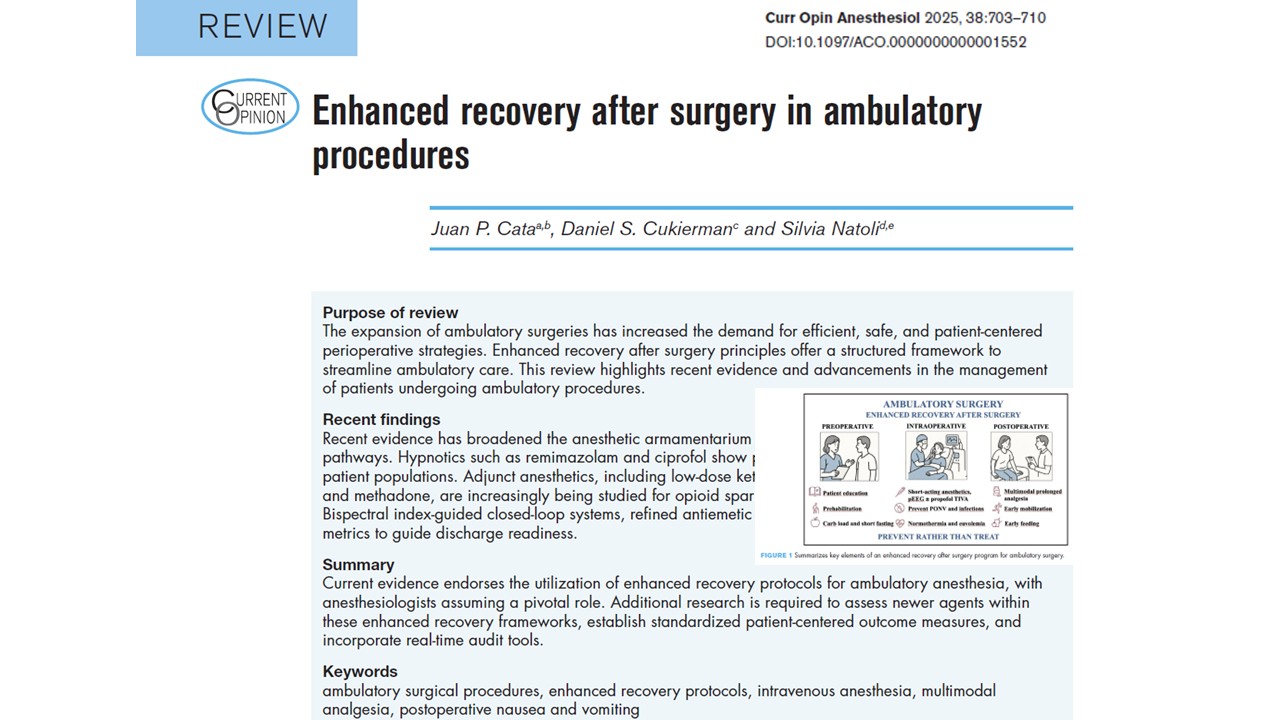
Core pillars of enhanced recovery in ambulatory anesthesia
ERAS protocols for outpatient procedures are designed around five core principles:
- Preoperative optimization and education
- Multimodal analgesia and PONV prevention
- Fluid management and normothermia
- Early nutrition and mobilization
- Opioid-sparing pain control
These components work synergistically to limit the physiological stress of surgery, support functional recovery, and enable same-day discharge. Below, we break down each element and explore the latest findings supporting its use in outpatient settings.
Preoperative care: setting the stage for success
Patient education and psychological preparation
- Early counseling reduces anxiety and aligns expectations.
- Interventions such as preoperative visits and surgical recovery coaching have been shown to enhance compliance and satisfaction.
- Educating patients about pain management, early mobilization, and return-to-activity plans improves postoperative outcomes.
Preoperative fasting and nutrition
- Guidelines recommend fasting for 6 hours (solids), 4 hours (breast milk), and 2 hours (clear fluids).
- Oral carbohydrate loading (200 ml, administered up to 2 hours before surgery) is safe and can help reduce preoperative thirst, hunger, and insulin resistance.
- Malnutrition remains an underrecognized risk; prehabilitation programs combining nutritional, physical, and psychological support show promise, especially in vulnerable patients.
Intraoperative care: modern anesthetic strategies
Fluid and temperature management
- Maintaining euvolemia with balanced crystalloids minimizes PONV, dizziness, and delayed discharge.
- Use of 5% dextrose solutions can lower PONV rates in high-risk patients.
- Prewarming protocols improve thermal comfort and reduce recovery times.
Anesthetic techniques: propofol, remimazolam, and beyond
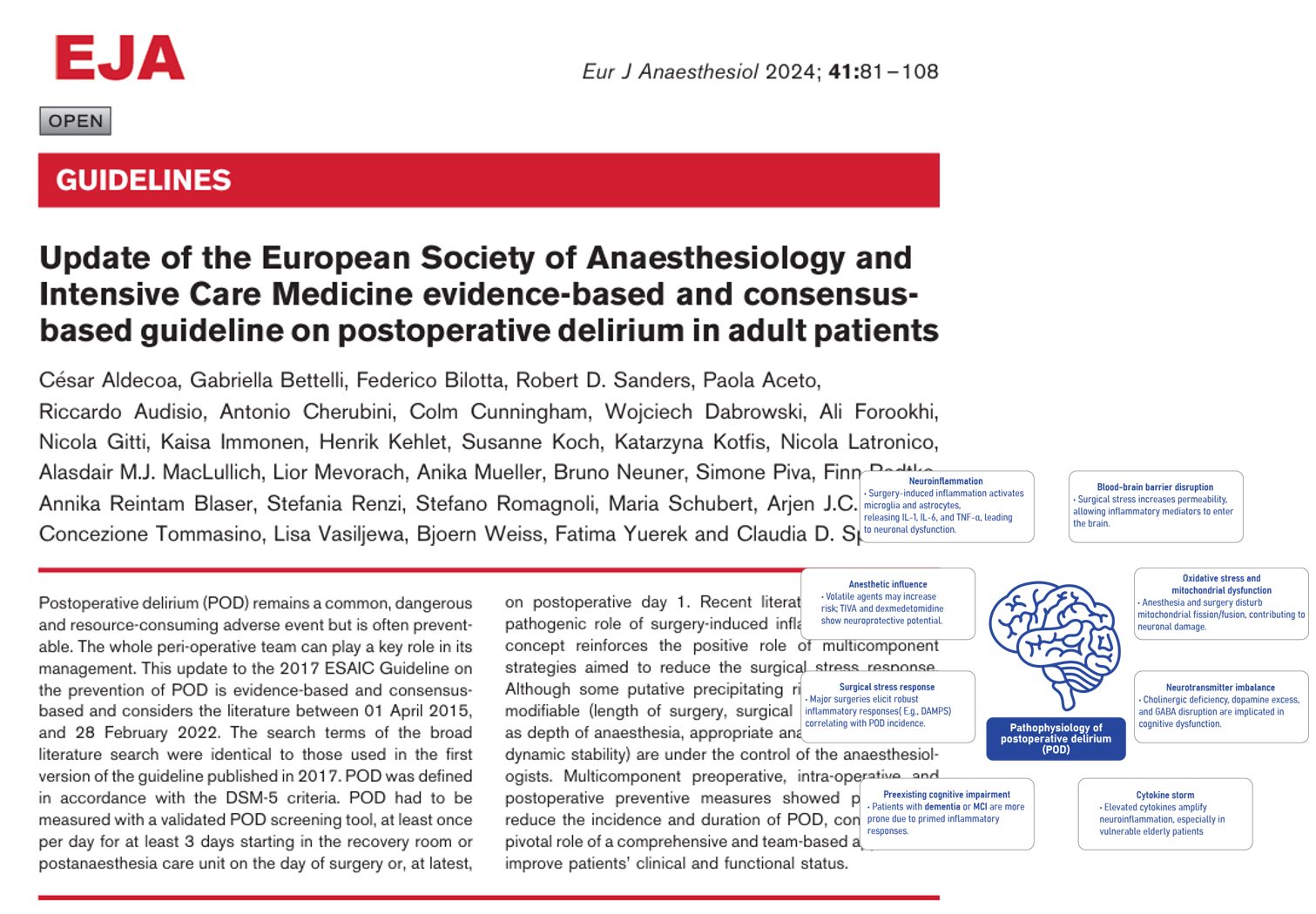
- Propofol-based total intravenous anesthesia (TIVA) is favored due to antiemetic properties and better recovery scores compared to volatile agents.
- Remimazolam, an ultra-short-acting benzodiazepine, is emerging as a safe option for patients with cardiovascular or respiratory comorbidities.
- Comparative studies suggest shorter emergence and extubation times with remimazolam-flumazenil compared to propofol, although large-scale trials, such as THRIVE, are ongoing.
Technological innovations: EEG-guided and closed-loop systems
- Bispectral Index (BIS)-guided anesthesia helps prevent excessive depth, reduces drug consumption, and accelerates recovery.
- Closed-loop Target-Controlled Infusion (TCI) systems with EEG monitoring have demonstrated reduced discharge times and optimized anesthetic delivery.
Pain and PONV management: cornerstone of outpatient recovery
PONV prophylaxis
- Multimodal antiemetic strategies include:
- Dexamethasone
- 5-HT3 receptor antagonists (ondansetron, palonosetron)
- Neurokinin-1 antagonists (aprepitant)
- Scopolamine patches
- Intravenous dextrose
- Propofol TIVA
- Meta-analysis shows a three-drug regimen (aprepitant + dexamethasone + ondansetron) reduces PONV by 66% in high-risk patients.
Multimodal analgesia
- Current best practice promotes opioid-sparing regimens:
- NSAIDs, acetaminophen, COX-2 inhibitors
- Low-dose ketamine and dexmedetomidine
- Intravenous methadone (e.g., 0.25 mg/kg IBW) has been shown to reduce postoperative opioid needs without increasing adverse effects.
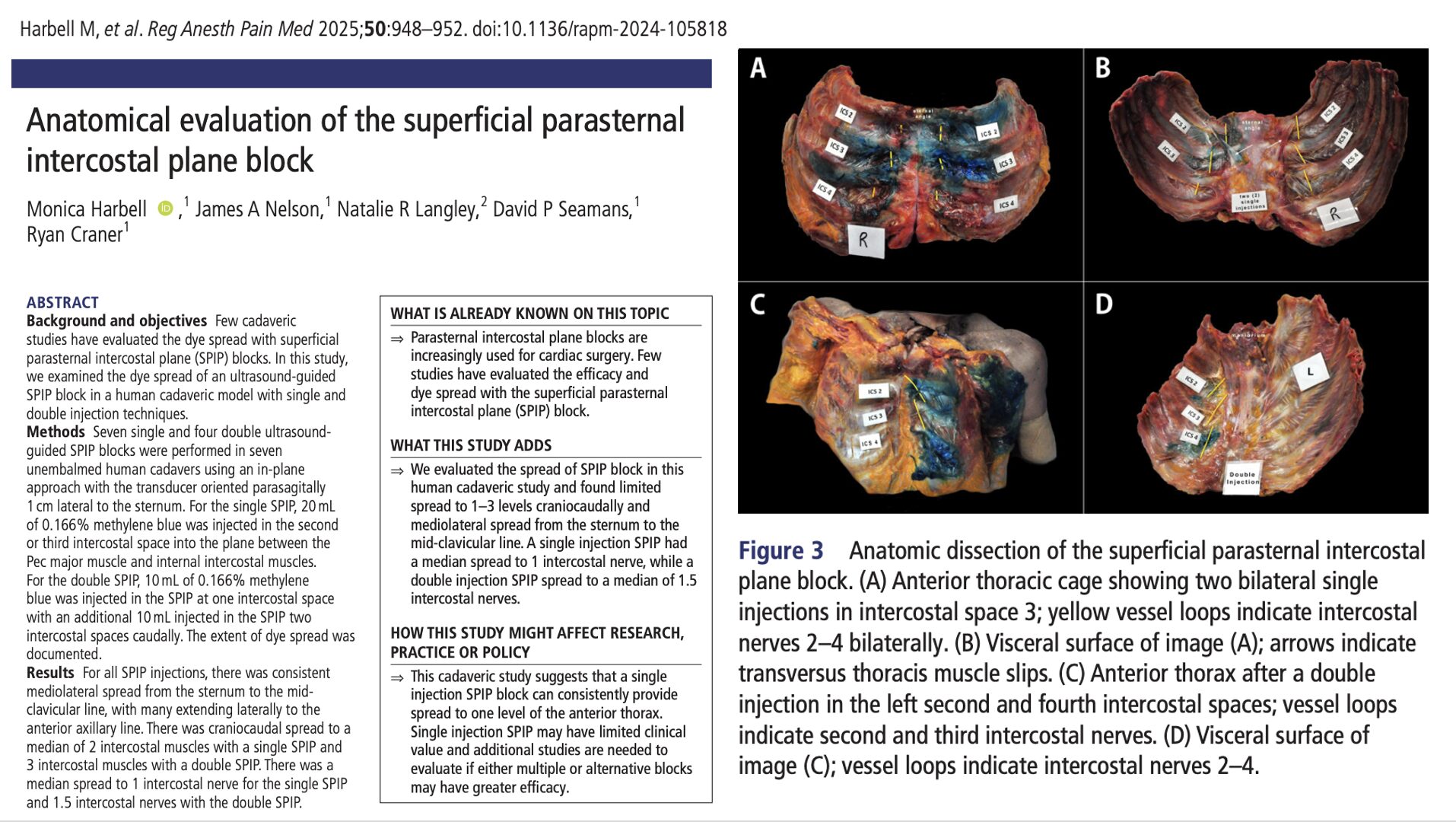
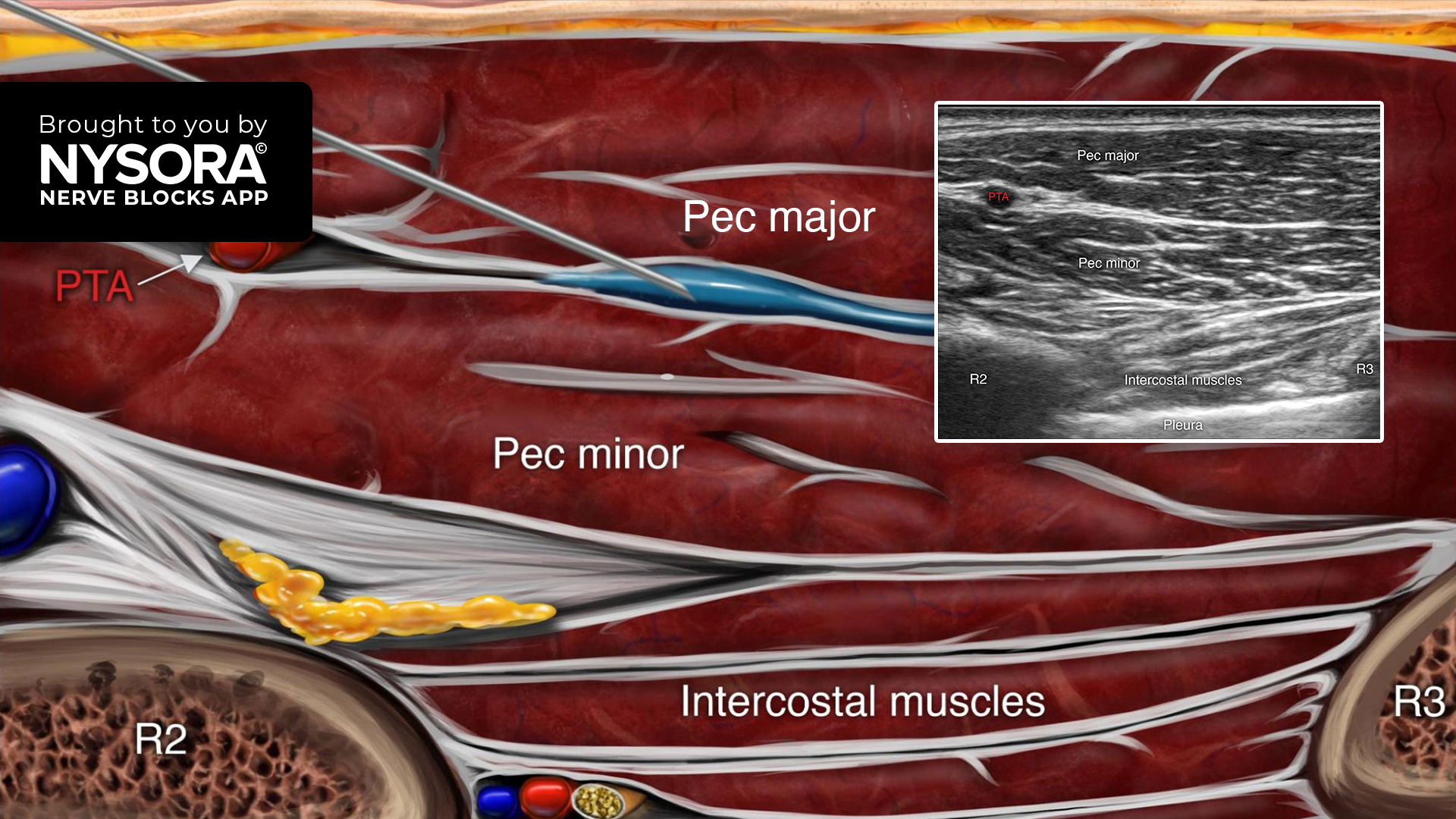
- Regional anesthesia remains integral but is not without challenges:
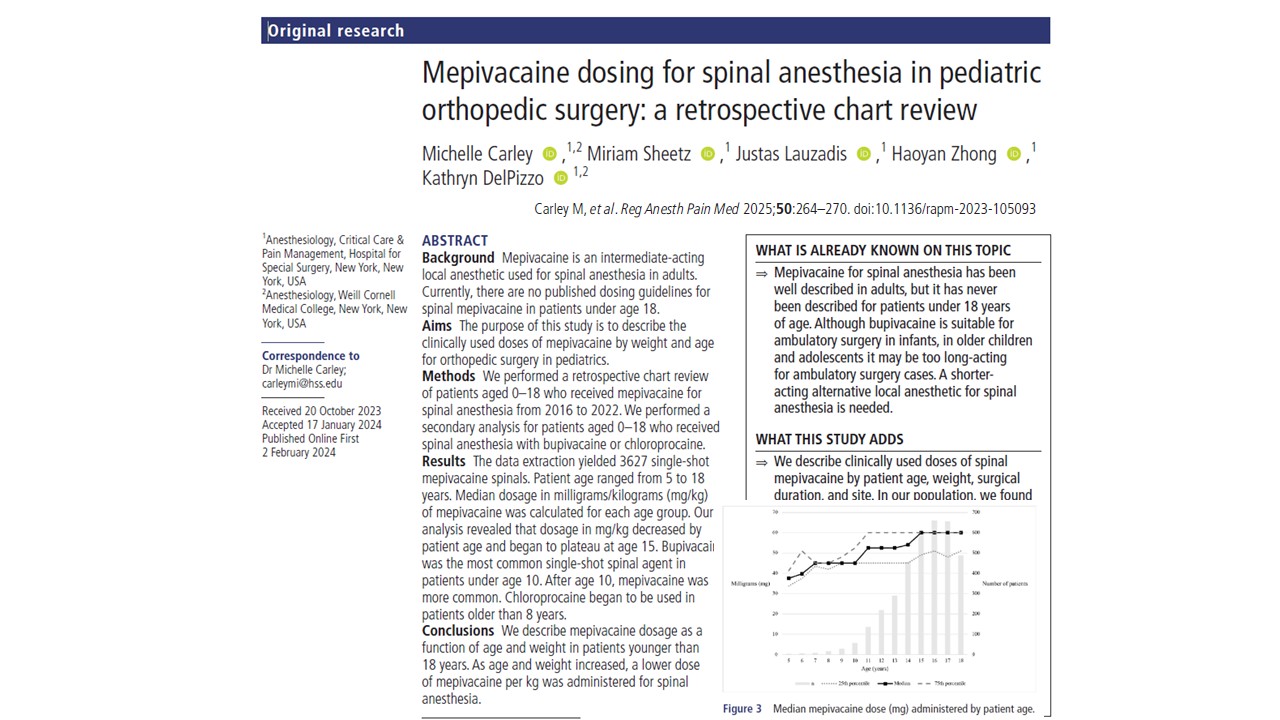
- Rebound pain with single-shot blocks (e.g., ropivacaine 0.5%) can worsen postoperative pain.
- Use of intermediate-acting agents like mepivacaine may offer a balance between analgesia and recovery.
Emerging options
- Novel agents, such as suzetrigine and TRPV1 antagonists, hold potential for future ERAS pathways.
- Acupuncture has shown efficacy in randomized trials for acute pain and PONV, suggesting it may be an adjunctive option.
Postoperative care: from PACU to home
Avoiding catheters and drains
- Minimizing the use of urinary catheters and wound drains decreases pain, infection risk, and length of stay.
- For neuraxial anesthesia cases, 2-chloroprocaine and low-dose bupivacaine are preferred due to lower urinary retention rates.
Early ambulation and feeding
- Mobilization within 4–6 hours post-op is critical for timely discharge.
- Neuraxial and peripheral blocks must be balanced to avoid motor blockade, which can delay mobility.
- Adequate antiemetic management ensures patients tolerate oral intake and transition smoothly to oral analgesics.
Monitoring, audit, and compliance: ensuring sustainable success
Why audit matters
- Compliance rates of over 70% correlate with improved outcomes.
- High adherence (>90%) has been achieved in ambulatory cancer surgery using real-time dashboards.
- Active patient components (e.g., early ambulation) often lag behind passive ones; targeted interventions are needed to address this gap.
Implementation strategies
- Use of interactive dashboards for tracking outcomes.
- Standardization of metrics and protocols while allowing for patient-specific tailoring.
- Regular review cycles are conducted to identify and correct areas of low compliance.
Cost-effectiveness: maximizing value in outpatient surgery
Implementing ERAS protocols involves upfront costs—team training, technology investments, and patient education—but evidence suggests these are offset by:
- Shorter hospital stays
- Lower complication and readmission rates
- Improved recovery and patient satisfaction
Several studies show that even high-risk surgeries, including total joint arthroplasties and mastectomies, can be safely transitioned to outpatient settings using ERAS protocols. While more research is needed to confirm cost savings across all surgery types, the trend strongly supports ERAS adoption as a cost-effective model.
Conclusion
Enhanced recovery after surgery protocols are revolutionizing outpatient surgical care. As the volume of ambulatory procedures increases, anesthesiologists must lead the development and implementation of evidence-based, patient-centered, and adaptable ERAS pathways that cater to a variety of clinical scenarios.
By leveraging newer anesthetics like remimazolam, advanced monitoring tools, and opioid-sparing multimodal strategies, providers can improve outcomes and enhance patient experience. The integration of rigorous auditing ensures that ERAS protocols remain effective and sustainable across institutions.
Looking ahead, continued innovation and research into novel pharmacological agents, digital recovery tracking, and personalized recovery models will further refine the role of ERAS in ambulatory anesthesia.
Read more in the full article in Current Opinion in Anaesthesiology.
Cata JP, Cukierman DS, Natoli S. Enhanced recovery after surgery in ambulatory procedures. Curr Opin Anaesthesiol. 2025 Dec 1;38(6):703-710.
Learn more about ERAS protocols in our Regional Anesthesiology Module on NYSORA 360 on NYSORA 360—an essential learning resource for residents with practical, up-to-date guidance.