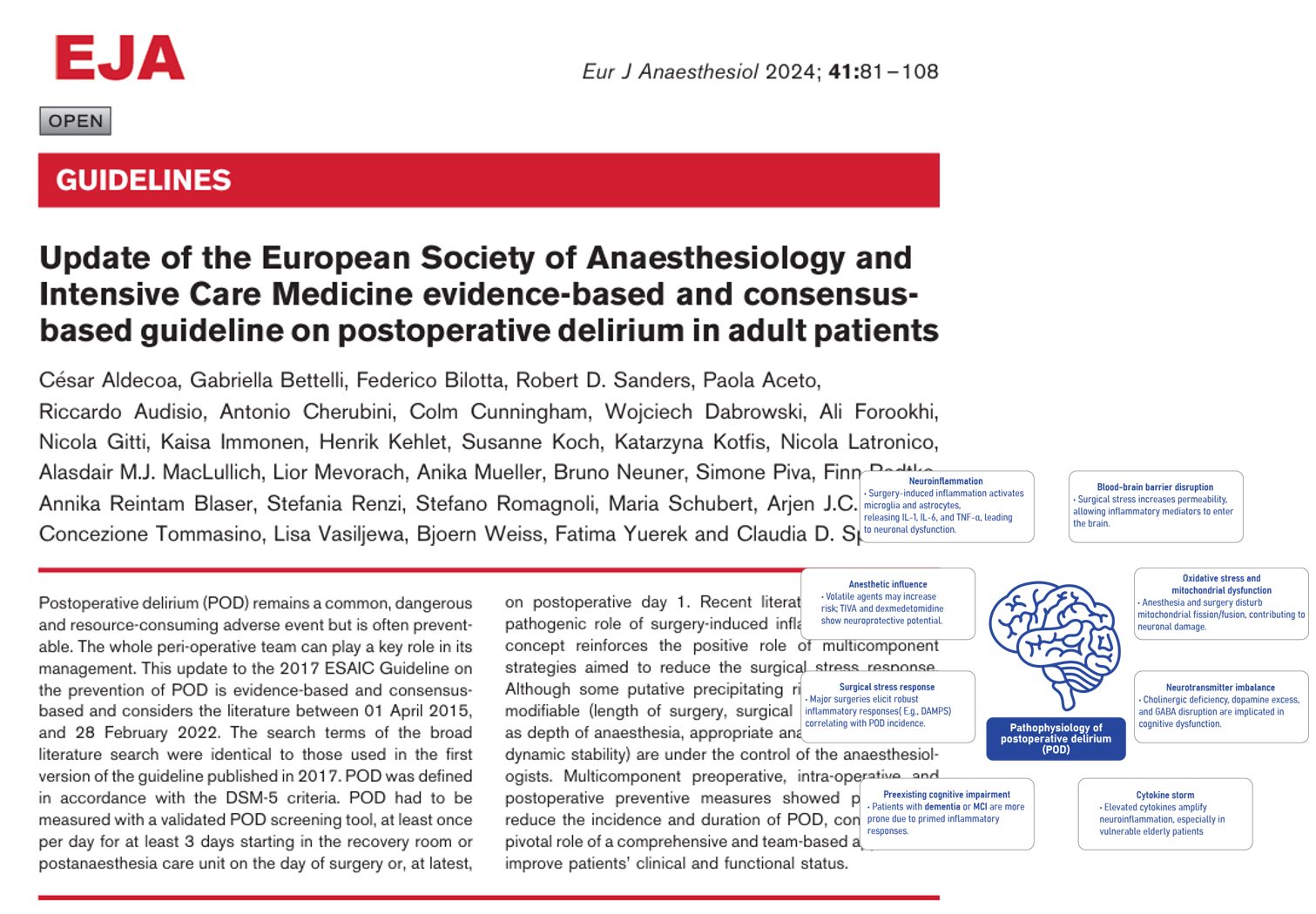
Postoperative delirium (POD) is a frequent and serious complication in older adults undergoing surgery, marked by acute cognitive disturbances. In recent years, electroencephalography (EEG) has emerged as a promising non-invasive tool to identify patients at risk of POD. A new systematic review by Bruzzone et al. (2025) offers a comprehensive examination of EEG’s role across the perioperative continuum; before, during, and after surgery.
Understanding postoperative delirium
What is POD?
- POD is a transient neuropsychiatric condition with fluctuating attention and cognitive impairments.
- It typically arises within 1 to 3 days after surgery.
- Incidence in older adults ranges between 11% and 51%.

Why is POD important?
- Associated with longer hospital stays, increased mortality, and lasting cognitive decline.
- Risk is higher in patients with preexisting cognitive vulnerabilities or neurodegenerative disorders.
The role of EEG in POD
What is EEG?
- EEG measures brain electrical activity using scalp electrodes.
- Frequency bands include delta (1–3 Hz), theta (4–7 Hz), alpha (8–13 Hz), and beta (13–20 Hz).
- EEG slowing, particularly increased delta and theta activity, is associated with delirium.
Why use EEG for POD?
- Offers real-time insight into brain function.
- Can potentially identify at-risk individuals before symptoms develop.
Key findings from the systematic review
Study overview
- Total studies reviewed: 55
- Participants: 13,046
- POD incidence: 21% (n = 2,706)
Preoperative EEG
- 16 studies investigated preoperative EEG.
- Most used power spectral analysis; results were inconsistent.
- Common findings in patients who developed POD:
- Lower spectral edge frequency (SEF)
- Reduced gamma band power
- Changes in alpha connectivity
- Several studies found no significant EEG changes before surgery.
Intraoperative EEG
- 38 studies examined intraoperative EEG data.
- Most used BIS (bispectral index) or SedLine monitors.
- Main EEG indicators associated with POD:
- Increased burst suppression (BS) duration
- Lower alpha power during anesthesia
- Absence of spindle activity during emergence
Burst suppression and POD
- Seen as a marker of brain hypoactivity.
- Strongly associated with higher POD risk.
- Studies showed conflicting results about BIS-guided anesthesia reducing POD.
Postoperative EEG
- 13 studies assessed EEG post-surgery.
- Findings in delirious patients included:
- Increased delta activity
Decreased alpha and beta power - Loss of functional connectivity
- Presence of seizures in some cardiac surgery patients
- Increased delta activity
Practical applications and challenges
Can EEG help predict POD?
- Yes, especially intraoperative EEG showing burst suppression or alpha power reduction.
- No, if relying solely on preoperative data due to inconsistent results.
Challenges
- Wide variability in EEG methods and measures across studies.
- Differences in patient demographics, surgery types, and delirium assessment tools.
- Lack of standardized EEG protocols in clinical practice.
Steps for future research
- Standardize EEG protocols: Use common devices and analysis methods.
- Focus on high-risk populations: Elderly patients with cognitive impairment.
- Integrate biomarkers: Combine EEG with Alzheimer’s disease markers for better prediction.
- Large multicenter trials: Validate EEG measures across diverse patient groups.
- Develop algorithms: Use AI to analyze EEG and predict POD in real-time.
Conclusion
EEG has significant potential as a tool for understanding, predicting, and perhaps even preventing postoperative delirium. While intraoperative EEG shows the most promise currently, standardized research is needed to translate these insights into clinical practice. Integrating EEG with cognitive assessments and biomarkers could pave the way for early identification and improved outcomes in vulnerable surgical populations.
Reference: Bruzzone MJ, et al. Electroencephalographic Measures of Delirium in the Perioperative Setting: A Systematic Review. Anesth Analg. 2025;140:1127-1139.
For more information on postoperative delirium, check out Anesthesia Updates on the NYSORA Anesthesia Assistant App.
Get access to step-by-step management algorithms, the latest research, and peer-reviewed insights—all in one place. Download the app today and experience the future of anesthesia education and decision-making.
AI On Call: Case of the Week
We asked the NYSORA’s Anesthesia Assistant what to consider when planning anesthesia for a 76-year-old man with hypertension and mild cognitive impairment (MoCA score: 23) scheduled for laparoscopic cholecystectomy.