As pediatric anesthesia advances, one drug has risen rapidly in popularity, dexmedetomidine. Touted for its sedative and analgesic effects without respiratory depression, this agent has become a mainstay in operating rooms worldwide. But a new hospital registry study by Azimaraghi et al. raises critical questions about whether this off-label use in children may cause more harm than benefit.
Published in the British Journal of Anaesthesia in 2024, the study is among the largest of its kind. It examined over 18,000 pediatric surgical cases to assess the hemodynamic, economic, and recovery-related impacts of dexmedetomidine in children under general anesthesia.
What is dexmedetomidine?
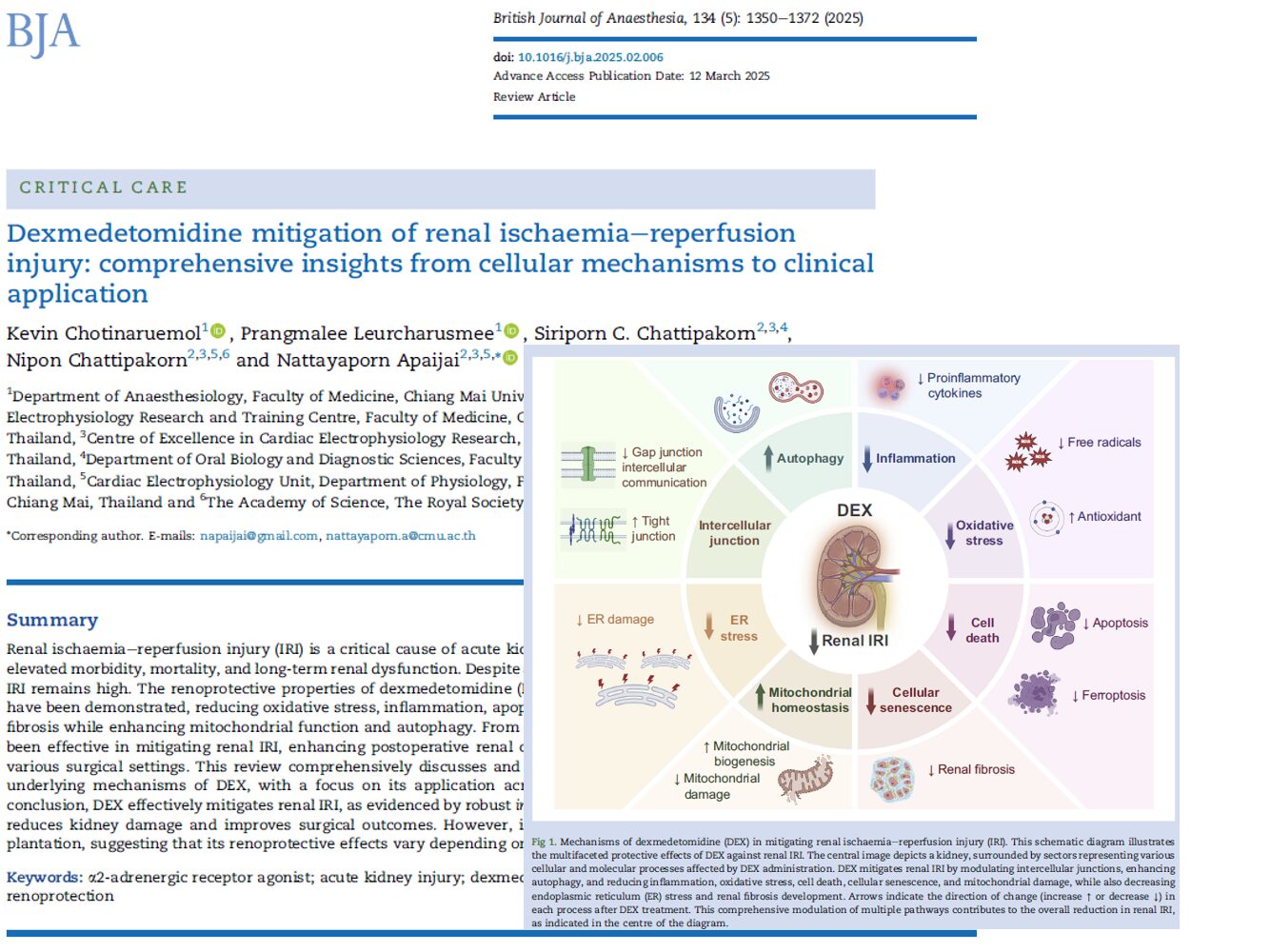
Dexmedetomidine is an α2-adrenergic receptor agonist used to sedate patients in critical care settings. It offers sedation without suppressing breathing, which makes it attractive for use in children. However, it is not approved by the U.S. FDA for pediatric use.
Key properties:
- Short-acting in adults (half-life ~2–4 hours)
- Prolonged half-life in neonates and preterms (up to 7 hours)
- Provides anxiolysis and analgesia
- Minimal respiratory depression
Despite its benefits, real-world data suggest its effects may be more complex in pediatric patients.
Major findings from the study

- PACU stay: Prolonged by 20 minutes on average
- Bradycardia odds (HR < 100 bpm): Increased by 32%
- Hypotension odds (MAP < 55 mm Hg): Increased by 27%
- Hospital cost: Higher by $1,311
- Emergence delirium: No preventive effect observed
Clinical concerns: sedation with side effects
-
Longer PACU recovery time
Patients given dexmedetomidine stayed ~20 minutes longer in the PACU. The delay was most pronounced in:
- Children aged ≤ 2 years
- Undergoing ambulatory procedures
- With surgical times under 60 minutes
In these high-risk groups, PACU times increased by over 33 minutes, a significant delay in a busy pediatric hospital.
-
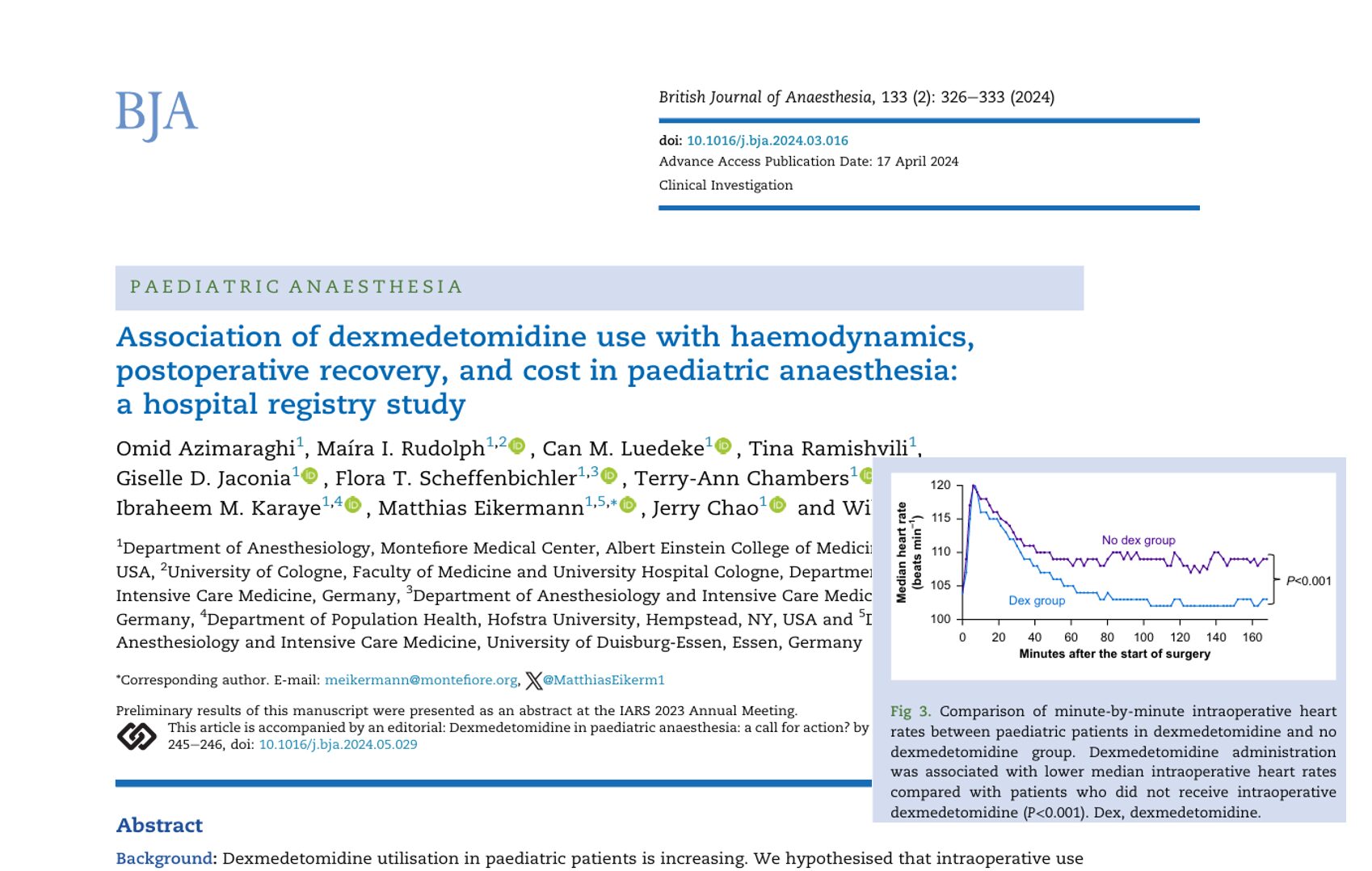
Hemodynamic instability
The study confirmed concerns about bradycardia and hypotension:
- Median heart rate was significantly lower throughout surgery.
- Odds of HR <100 bpm increased by 32%.
- Odds of MAP <55 mm Hg increased by 27%.
Such changes, while not always dangerous, could complicate management in vulnerable patients.
-
No benefit in emergence delirium
Despite common assumptions, dexmedetomidine did not reduce postoperative delirium. In fact, patients receiving it were more likely to require additional sedatives in the PACU.
-
Cost implications
Hospital costs rose by an average of $1,311 per patient. The cost increase correlated strongly with longer PACU stays and the use of high doses of dexmedetomidine.
Step-by-step guide for clinicians
Safer use of dexmedetomidine in pediatric surgery:
- Evaluate necessity
Use only if the benefits outweigh the potential complications, especially in short or minor procedures. - Screen high-risk patients
Be cautious in children <2 years or those with cardiac conditions. - Adjust the dose wisely
Stay below 0.54 mg/kg when possible to minimize prolonged sedation. - Avoid late administration
Giving the drug within 60 minutes of surgery end prolongs PACU stay more significantly. - Use adjunctively with caution
When combined with opioids or benzodiazepines, the impact on PACU stay was slightly mitigated. - Monitor closely
Watch for bradycardia and hypotension intraoperatively.
Variability in practice
The study also uncovered wide variation in anesthesiologists’ use of dexmedetomidine:
- Some used it in as few as 17% of cases.
- Others used it in over 85%.
- Use of high doses (≥0.54 mg/kg) varied dramatically, suggesting a lack of standardized protocols.
This inconsistency underscores the need for evidence-based guidelines.
Real-world implications for hospitals
Dexmedetomidine use is skyrocketing, but this comes with a price:
- Longer PACU stays lead to fewer available beds and delays in care.
- Higher costs burden healthcare systems, especially in high-volume pediatric centers.
- Clinical benefits remain unclear, especially for routine or minor procedures.
Conclusion: Caution urged in pediatric use
Dexmedetomidine may offer a non-opioid alternative for sedation, but this large-scale study emphasizes the need for careful consideration. Prolonged recovery, elevated costs, and potential cardiovascular risks make its routine use in children challenging.
Hospitals and practitioners should re-evaluate current protocols, focusing on:
- Patient selection
- Dosing strategies
- Monitoring practices
- Alternatives with better recovery profiles
Final takeaway
Dexmedetomidine is not a one-size-fits-all solution. While it may be effective in specific settings, its off-label use in pediatric anesthesia must be approached with caution. This study sheds light on critical data and calls for a more individualized, evidence-based approach to pediatric sedation.
Reference: Azimaraghi O et al. Association of dexmedetomidine use with haemodynamics, postoperative recovery, and cost in pediatric anesthesia: A hospital registry study. Br J Anaesth. 2024;133:326-333.
Read more about this topic in the Anesthesia Updates section of the Anesthesia Assistant App. Prefer a physical copy? Get the latest literature and guidelines in book format. For an interactive digital experience, check out the Anesthesia Updates Module on NYSORA360!