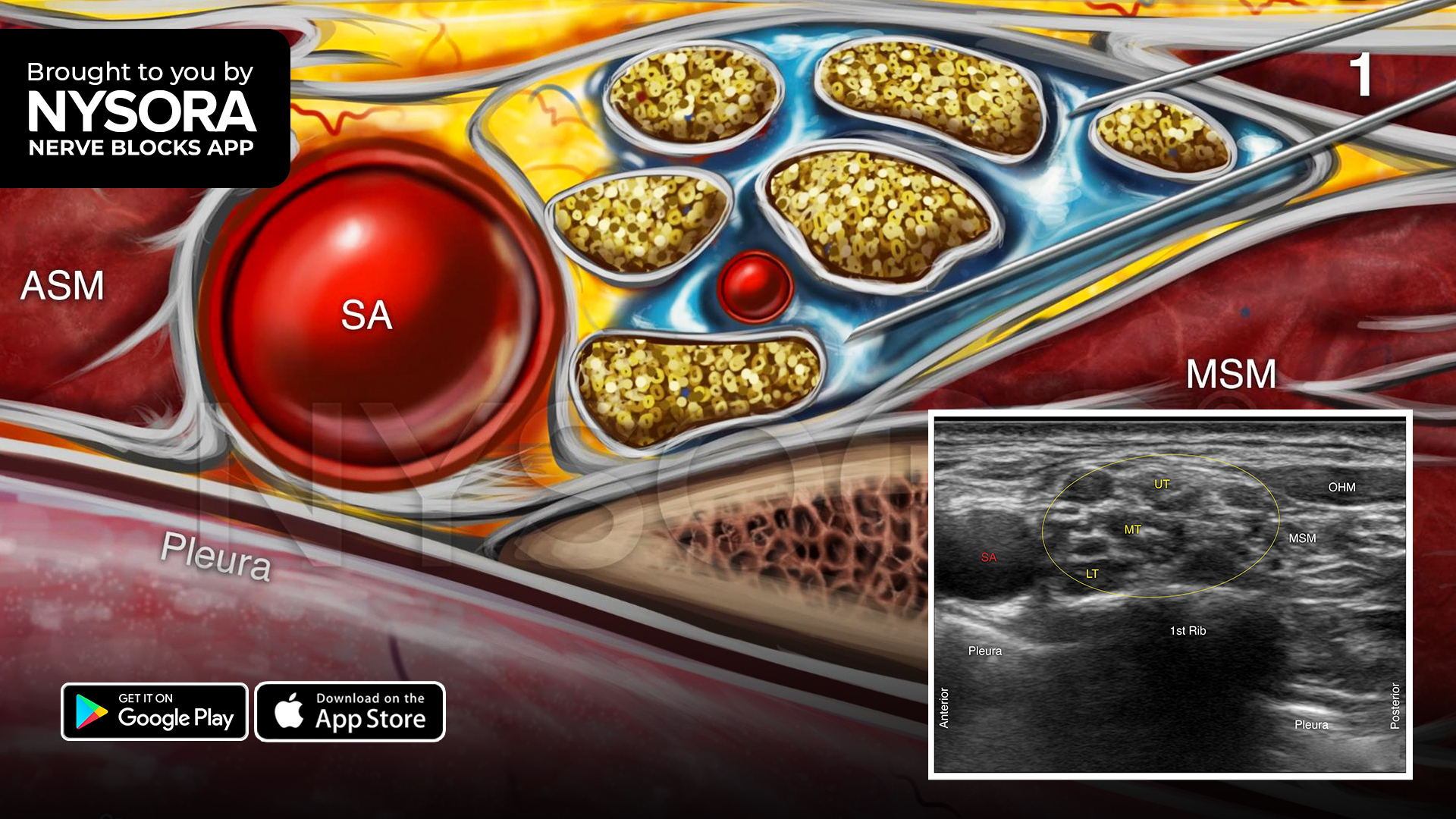
Regional anesthesia has become an essential technique in managing perioperative pain, particularly for upper limb surgeries. Among these, the supraclavicular brachial plexus block offers reliable and dense anesthesia for procedures on the forearm and hand. However, one persistent challenge in regional anesthesia is extending the duration of analgesia without compromising safety.
Dexamethasone, a potent glucocorticoid, has been increasingly used as an adjunct to local anesthetics to prolong nerve block duration. It can be administered either perineurally (directly at the nerve site) or systemically (intravenously). While previous studies have shown benefits from both approaches, there has been ongoing debate over which route is more effective, and whether combining both could offer improved outcomes. In this context, a randomized controlled trial sought to explore the additive or synergistic effects of administering dexamethasone both systemically and perineurally, alongside ropivacaine in supraclavicular brachial plexus blocks.
Study objective and methods
The primary objective of the study was to evaluate whether the combination of systemic and perineural dexamethasone offers additive or synergistic benefits in patients receiving supraclavicular brachial plexus blocks for distal upper limb surgeries. The primary outcome was the duration of sensory block. Secondary outcomes included motor block duration, rebound and worst pain scores, opioid consumption, and side effects such as nausea or burning sensation.
This double-blinded, randomized controlled trial enrolled 104 adult patients scheduled for open reduction and internal fixation of distal radius fractures or carpometacarpal (CMC) arthroplasty. All participants received a supraclavicular block using 20 mL of 0.5% ropivacaine. They were randomly allocated to one of three groups:
- Group A (IV; n = 37): Received 8 mg of dexamethasone intravenously.
- Group B (IV + PN; n = 34): Received 4 mg intravenously and 4 mg perineurally.
- Group C (control group; n = 33): Received no dexamethasone.
Blinding was maintained across patients and investigators, and assessments were performed at regular intervals for up to 48 hours postoperatively.
Key findings
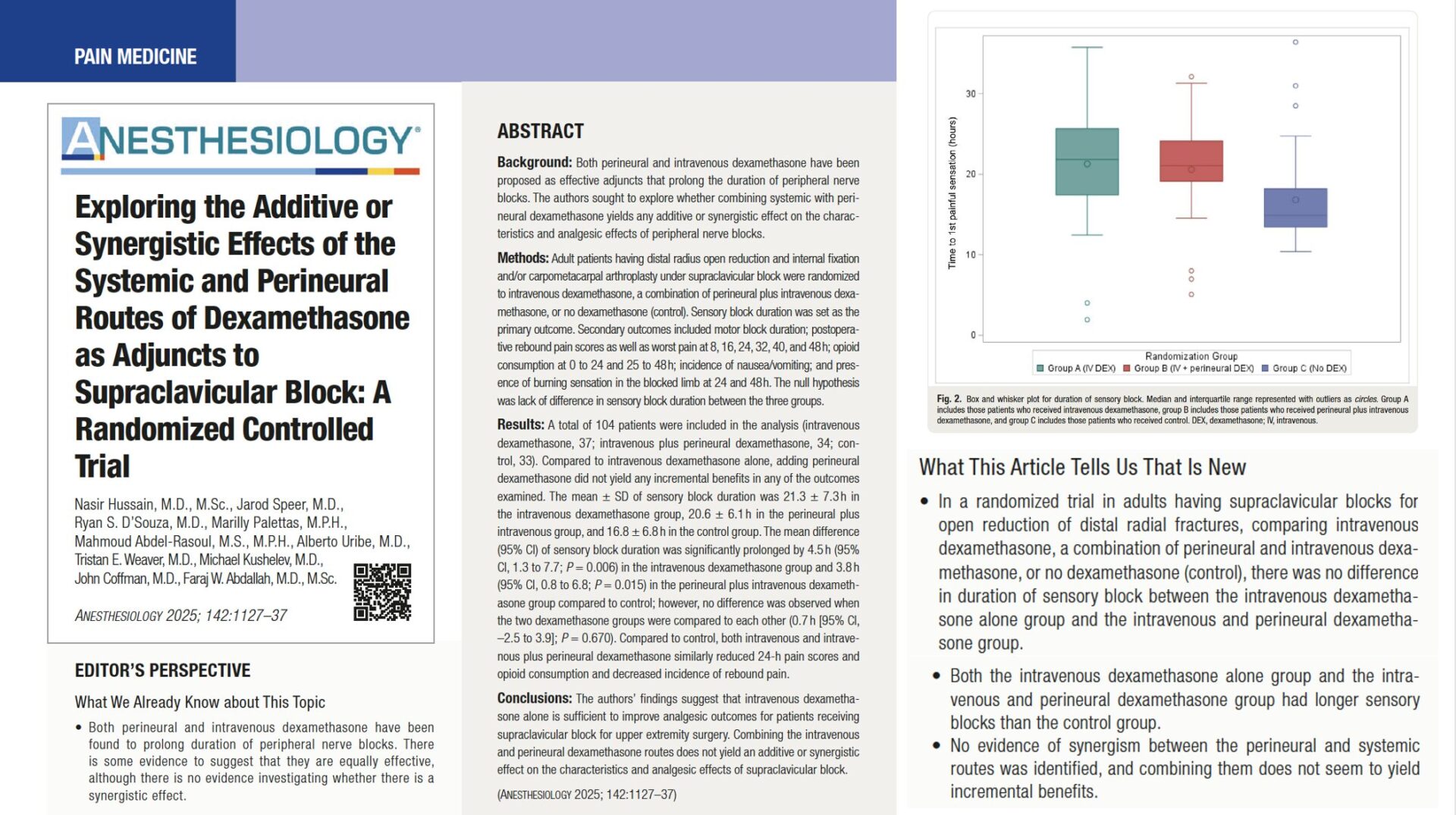
Primary outcome: Sensory block duration
The core result of the study was unambiguous: adding perineural dexamethasone to systemic administration did not extend the duration of sensory block beyond that achieved with intravenous dexamethasone alone. Both dexamethasone groups had significantly longer blocks than the control group, but there was no statistically significant difference between the IV and IV + PN groups.
This finding effectively refutes the idea of a synergistic or even additive benefit from using dual routes of dexamethasone administration. It confirms that IV dexamethasone alone is sufficient to achieve optimal sensory block duration in this surgical context.
Secondary outcomes
- Motor block duration was similarly prolonged in both dexamethasone groups relative to control but did not differ significantly between IV and IV + PN groups.
- Rebound pain and worst pain scores over 48 hours were lower in both dexamethasone groups compared to control. Pain assessments were performed at 8, 16, 24, 32, 40, and 48 hours, and consistently favored dexamethasone over no adjuvant.
- Opioid consumption, measured in oral morphine equivalents (OME), was significantly reduced in the dexamethasone groups compared to control. However, there was no difference between the two dexamethasone groups.
- Adverse events, including nausea, vomiting, and burning sensations in the blocked limb, were minimal and distributed similarly across all three groups. There was no evidence of neurotoxicity or serious complications related to perineural dexamethasone.
These outcomes strongly support the efficacy and safety of IV dexamethasone as a reliable adjuvant for supraclavicular blocks, without a need for additional perineural administration.
Conclusion
The findings from this randomized controlled trial offer strong evidence that intravenous dexamethasone alone is as effective as a combined systemic and perineural approach in prolonging the analgesic effects of supraclavicular brachial plexus blocks. The lack of a synergistic or additive benefit from using both routes simplifies clinical decision-making and reinforces the IV route as the preferred method of dexamethasone administration.
In a field where every dose, route, and technique matters for optimizing outcomes and reducing complications, this trial brings clarity to an important question in regional anesthesia.
Future research
Future research should examine whether varying the dose or ratio of dexamethasone—such as higher or unequal distributions between routes—might produce a dose-response effect that improves block duration or quality. Investigators should also explore whether the findings from this study apply to other nerve block sites, including interscalene, infraclavicular, or lower-limb blocks, to determine generalizability. Long-term safety remains a key concern, and larger, multicenter trials are needed to monitor outcomes associated with repeated or cumulative dexamethasone exposure. Additionally, future studies should focus on patient-specific factors such as age, comorbidities, and baseline opioid use to determine if specific populations might benefit more from tailored administration strategies.
For more detailed information, refer to the full article in Anesthesiology.
Hussain N et al. Exploring the Additive or Synergistic Effects of the Systemic and Perineural Routes of Dexamethasone as Adjuncts to Supraclavicular Block: A Randomized Controlled Trial. Anesthesiology. 2025;142:1127-1137.
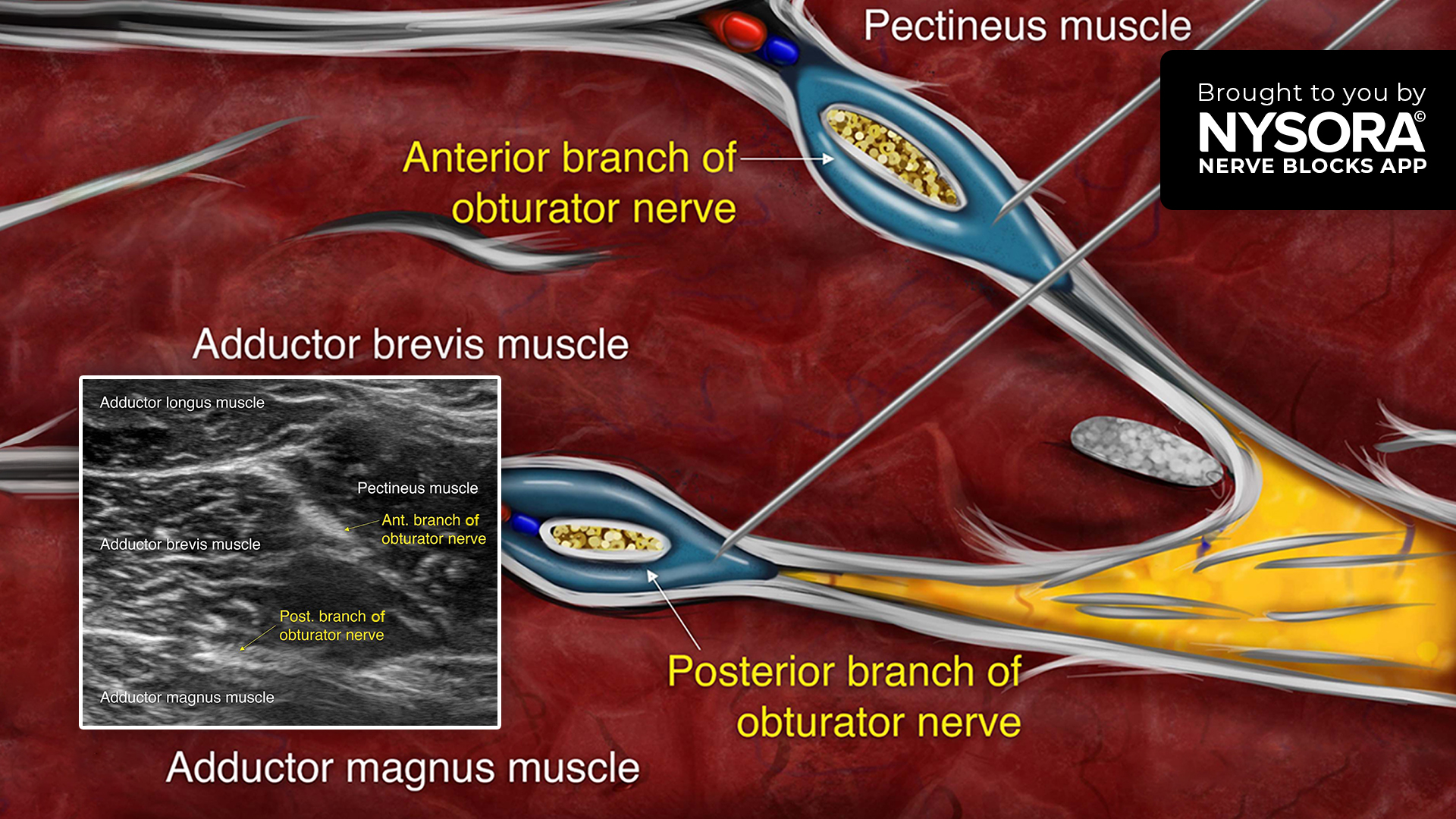
Download the Nerve Blocks App HERE for in-depth insights on the supraclavicular brachial plexus block. Prefer a physical copy? The bestselling NYSORA Nerve Blocks App is available in book format — an essential resource for mastering nerve blocks! And for a digital learning experience, check out the Nerve Block Manual Module on NYSORA360!