Learning objectives
- Describe and classify mitral regurgitation
- Describe the causes and mechanisms of mitral regurgitation
- Manage patients with mitral regurgitation
Definition & mechanisms
- Mitral regurgitation (MR) can be acute or chronic in onset, and primary or secondary in nature
- Primary MR is due to pathology of the valve preventing normal closure
- Secondary MR is caused by left ventricle dysfunction that affects the closing of the mitral valve
- The left atrium dilates as blood is ejected back into it
- Atrial fibrillation is common
- Overload of the pulmonary circulation causes dyspnea
- The LV is volume overloaded in, with dilation of the ventricle further worsening MR
- Acute MR:
- Can be caused by any disruption to the normal mechanism of the valve (growth of vegetations on the leaflets in infective endocarditis, chordae rupture in patients with pre-existing degenerative disease, or papillary muscle rupture due to an ST-elevation)
- The left atrium is unable to compensate acutely for the increased pressure caused by blood refluxing back into it
- Patients can present with sudden-onset dyspnea and require rapid stabilization and treatment
- Chronic MR:
- Primary: Abnormality of the leaflets that prevents them from closing normally
- Secondary: Anatomy of the valve is normal, but its function is impaired due to left ventricle pathology
Classification
Transoesophageal echocardiography remains the gold standard for defining the severity of the MR:
| Mild | Moderate | Severe | |
|---|---|---|---|
| Regurgitant fraction | <30% | 30–49 | ≥50% |
| Regurgitant orifice area | <0.20 cm2 | 0.2–0.39 cm2 | ≥0.40 cm2 |
| Regurgitant volume | <30 mL/beat | 30–59 mL/beat | ≥60 mL/beat |
Treatment
- Medical
- Acute MR: Filling pressure reduction with nitrates or diuretics and afterload reduction with vasodilators or an intra-aortic balloon pump as bridging to definitive treatment
- Chronic MR: Treatment is in line with standard heart failure management including β-blockers, angiotensin-converting enzyme inhibitors, and aldosterone antagonists, with diuretics where heart failure is present
- Surgical
- Primary MR:
- Surgery is indicated if the MR is severe and acute in nature and if the MR is chronic and causing symptoms, with no contraindications to surgery
- Valve repair, rather than replacement, is preferred
- Secondary MR:
- In symptomatic patients with severe left ventricle failure, the benefits of surgery are controversial unless the underlying condition can be reversed
- Primary MR:
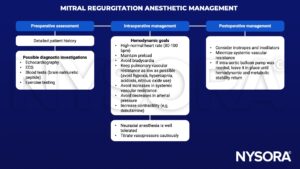
Anesthetic management
Suggested reading
- Holmes K, Gibbison B, Vohra HA. Mitral valve and mitral valve disease. BJA Education. 2017;17(1):1-9.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com