Learning objectives
- Difference between intra-abdominal pressure (IAP) and abdominal compartment syndrome (ACS)
- Recognize ACS and the pathophysiological consequences of ACS
- Management of ACS
Definition and mechanisms
- Normal intra-abdominal pressure (IAP) ranges between 0-5 mmHg while in critically-ill patients, an IAP of 5-7 mmHg is considered normal
- Intra-abdominal hypertension is defined as a sustained intra-abdominal pressure (IAP) ≥12 mmHg
- Abdominal compartment syndrome (ACS) is defined as IAP rises > 20 mmHg thereby leading to new organ dysfunction
- Abdominal perfusion pressure (APP) is calculated as the mean arterial pressure (MAP) minus the IAP
- A critically ill patient with high mortality & morbidity
Signs and symptoms
- Malaise
- Weakness
- Dyspnea
- Abdominal bloating
- Abdominal pain
- Hypoxia
- Hypercabia
- Oliguria
Etiology
Acute ACS
- Primary: due to injury or disease in the abdominopelvic region (e.g., pancreatitis, abdominal trauma)
- Secondary: does not originate in the abdomen or pelvis (e.g., fluid resuscitation, sepsis, burns)
Chronic ACS
- In association with peritoneal dialysis or chronic ascites
Artificially raised IAP
- External compression, for example, prolonged prone positioning for spinal surgery with insufficient provision for abdominal movement
Risk factors
| Diminished abdominal wall compliance | Acute respiratory failure, especially with elevated intrathoracic pressure Abdominal surgery with subjectively tight primary closure Major trauma/burns Prone positioning, head of bed elevated > 30° High BMI, central obesity |
| Increased intra-luminal contents | Gastroparesis Ileus Colonic pseudo-obstruction |
| Increased abdominal contents | Hemoperitoneum/pneumoperitoneum Ascites/liver dysfunction |
| Capillary leak/fluid resuscitation | Metabolic acidosis ( pH < 7.2) Hypotension Perioperative hypothermia Polytransfusion (>10 units of blood/24 h) Coagulopathy (platelets < 55 000 mm-3, prothrombin time > 15 s, partial thromboplastin time > 2 times normal, or international standardized ratio >1.5) Massive fluid resuscitation (> 5 litre/24 h) Pancreatitis Oliguria Sepsis Trauma Burns Damage control laparotomy |
Pathophysiological effects of raised IAP
| Central nervous system | Increased intra-cranial pressure |
| Cardiovascular system | Increased systemic vascular resistance Pulmonary vascular resistance Decreased venous return with concomitant venous congestion |
| Gastrointestinal and hepatic system | Decreased coeliac, mesenteric, hepatic and hepatic portal blood flow Increased oedema, bacterial translocation and liver dysfunction |
| Renal system | Increased renal tubular pressure and urinary obstruction Decreased renal blood flow and urine output |
| Respiratory system | Increased ventilation-perfusion mismatch, ventilatory pressure, basal atelectasis and PaCO2 Decreased chest wall and pulmonary compliance and PaO2 |
Diagnosis
- Indirect measurement of IAP using intragastric, intracolonic, intravesical (bladder), or inferior vena cava catheters
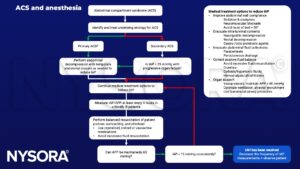
Management
- Patients with two or more risk factors should have IAP monitoring
- Treatment:
- Regimens lowering IAP
- Open the abdominal wound and perform a temporary closure of the abdominal wall with mesh or a plastic bag (Bogota bag)
- Regiments aiming at organ support
- Keep abdominal perfusion pressure (APP) (systemic blood pressure – intra-abdominal pressure) > 60mmHg
Keep in mind
- Consequences of decompression:
- Sudden ↓ cardiac output & SVR
- Reperfusion: risk of systemic acidosis & hyperkalemia
- Possible fatal arrhythmia & arrest
- Sudden change in respiratory compliance (avoid overventilation)
- Avoid bradycardia (preload is compromised & CO may be heart rate dependent)
- Maintain high preload particularly once decompressed
Suggested reading
- Neil Berry, Simon Fletcher, Abdominal compartment syndrome, Continuing Education in Anaesthesia Critical Care & Pain, Volume 12, Issue 3, June 2012, Pages 110–117.
- Mullens W, Abrahams Z, Skouri HN, et al. Elevated intra-abdominal pressure in acute decompensated heart failure: a potential contributor to worsening renal function? J Am Coll Cardiol. 2008;51(3):300-306.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com