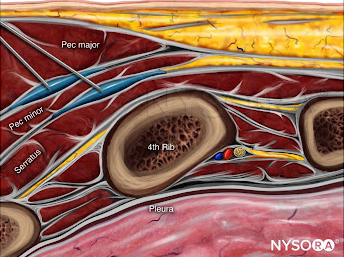
Total knee arthroplasty (TKA) is a common orthopedic procedure with a significant focus on optimizing postoperative pain management while preserving motor function. Regional anesthesia techniques that spare motor nerves are central to multimodal analgesia strategies that enable early ambulation and improved recovery.
While the femoral triangle block (FTB) effectively covers anterior knee pain, it does not adequately target the posterior knee. The interspace between the popliteal artery and capsule of the posterior knee (IPACK) block has become a valuable motor-sparing adjunct to FTB, yet its reproducibility may be affected by anatomical variation and technical complexity.
A recent randomized, double-blind, non-inferiority trial paired with cadaveric evaluation investigated whether the popliteal plexus block (PPB), a newer and technically simpler approach, is non-inferior to the IPACK block when combined with FTB.
Study objective and methods
The primary objective was to evaluate whether PPB is non-inferior to the IPACK block in preventing moderate-to-severe posterior knee pain 8 hours after TKA. The study also included a cadaveric investigation of injectate spread following PPB.
Design and participants
- Prospective, randomized, double-blind, non-inferiority trial.
- Conducted between October 2023 and August 2024.
- 90 participants enrolled; 86 included in final analysis (43 per group).
- All participants received general anesthesia and FTB, followed by either PPB or IPACK.
Inclusion and exclusion
Eligible participants were adults aged 20–85 years undergoing elective primary TKA. Exclusion criteria included BMI >40, cognitive dysfunction, contraindications to nerve blocks, and pre-existing motor dysfunction.
Intervention techniques
- FTB: Administered in both groups using 10 mL of 0.25% levobupivacaine near the saphenous nerve.
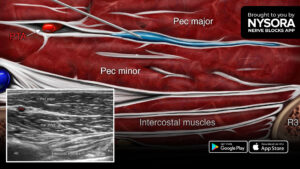
- PPB: Performed without leg repositioning; 15 mL of 0.25% levobupivacaine was injected near the superficial femoral artery before it enters the adductor hiatus.
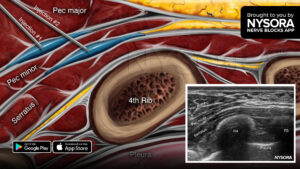
- IPACK: Administered via a distal approach with 15 mL of 0.25% levobupivacaine between the popliteal artery and posterior capsule.
Primary outcome
Incidence of moderate-to-severe posterior knee pain at 8 hours post-op (defined as NRS ≥4)
Secondary outcomes
- Pain scores at 8, 24, and 48 hours
- Fentanyl consumption
- Block performance time
- Motor and sensory function (tibial and common peroneal nerves)
- Nausea, complications, quality of recovery, and patient satisfaction
Cadaveric study
- PPB was performed on seven legs of four cadavers.
- Methylene blue dye was used to trace the spread of injectate.
- Dissections assessed coverage of articular nerve branches.
Key findings
-
Primary outcome
Incidence of moderate-to-severe posterior knee pain:
- PPB group: 6.7%.
- IPACK group: 11.6%.
- Difference (4.7%) met the pre-defined non-inferiority margin of 17%.
- Non-inferiority confirmed (p<0.001).
Non-inferiority was also confirmed at 48 hours postoperatively (p=0.037).
-
Secondary outcomes
- Pain scores: No significant difference between groups at any time point.
- Fentanyl consumption: Significantly lower in the PPB group at 24 hours (p = 0.031).
- Block performance time: PPB group median 3 minutes vs. IPACK group 5 minutes (p < 0.0001).
- Motor and sensory function: No complete motor block was observed in either group; some participants experienced mild ankle weakness.
- Nausea: Significantly lower in the PPB group at 24 hours (p = 0.014).
- Complications: One arterial puncture in the PPB group, resolved without sequelae; no falls or serious complications.
-
Cadaveric findings
- Dye spread consistently stained posterior articular branches in over 80% of specimens, except the inferior tibial nerve branch (28.6%).
- Anterior structures such as the saphenous nerve, nerve to vastus medialis, and nerve to vastus intermedius were also stained.
- No spread to the main sciatic nerve trunk was observed.
- Mean distance from injection site to sciatic bifurcation: 1.5 cm.
These findings suggest that PPB reliably reaches the popliteal plexus and may offer additional anterior capsule coverage through involvement of the nerve to vastus intermedius.
Conclusion
This study demonstrates that the popliteal plexus block is non-inferior to the IPACK block in managing posterior knee pain within 8 hours of TKA. PPB also offers potential benefits, including:
- Shorter block performance time.
- Lower postoperative opioid use.
- Reduced incidence of nausea.
Given its technical simplicity and consistent anatomical coverage, PPB may be a valuable motor-sparing technique in TKA multimodal analgesia protocols. However, the authors caution that results were obtained in a controlled setting by an experienced anesthesiologist, and wider validation is necessary.
Future research
The authors recommend further studies to explore:
- Functional recovery metrics (e.g., early ambulation, physical therapy milestones).
- Optimal injectate volume for balancing analgesia and motor preservation.
- Comparative effectiveness of distal versus proximal PPB approaches.
- Broader implementation across patient populations and anesthesia providers.
Clinical implications
The findings of this study have practical relevance for anesthesiologists and surgical teams involved in perioperative care for TKA. The PPB offers a technically straightforward, reproducible method for achieving posterior knee analgesia without the need for leg repositioning. Given its non-inferiority to the IPACK block, and its shorter block performance time and reduced postoperative opioid use, PPB could serve as a preferred option in busy clinical settings or for providers with limited experience in complex posterior approaches. Furthermore, by avoiding motor blockade and minimizing complications, PPB aligns well with ERAS principles, particularly in elderly or high-risk patients where early ambulation is critical. These advantages support the integration of PPB into multimodal analgesia protocols for TKA, although broader validation across diverse clinical environments is warranted.
Clinical pearls
- PPB non-inferior to IPACK for posterior knee pain (NRS ≥4) at 8h postop.
- Faster to perform: PPB 3 min vs IPACK 5 min.
- Lower fentanyl use and less nausea with PPB.
- Cadaveric study: PPB reliably stains posterior articular branches.
Practical tip: For TKA cases where time efficiency matters, PPB offers comparable pain relief to IPACK with faster setup and fewer side effects.
For more detailed information, refer to the full article in RAPM.
Fujino T. et al. Analgesic efficacy of popliteal plexus block versus infiltration between the popliteal artery and capsule of the posterior knee block combined with femoral triangle block after total knee arthroplasty: a randomized non-inferiority trial and cadaveric evaluation. Reg Anesth Pain Med. Published online August 12, 2025.
Subscribe to the NYSORA Nerve Blocks App for 60+ techniques, PRO tips, clinical videos, and the latest updates.