Autologous breast reconstruction using the latissimus dorsi flap remains a widely used and effective technique, particularly for patients who have undergone radiation therapy. However, the procedure is associated with significant postoperative pain due to extensive tissue dissection, contributing to prolonged hospital stays. Traditional analgesic approaches, such as surgeon-administered local infiltration and systemic opioids, often fall short in optimizing recovery.
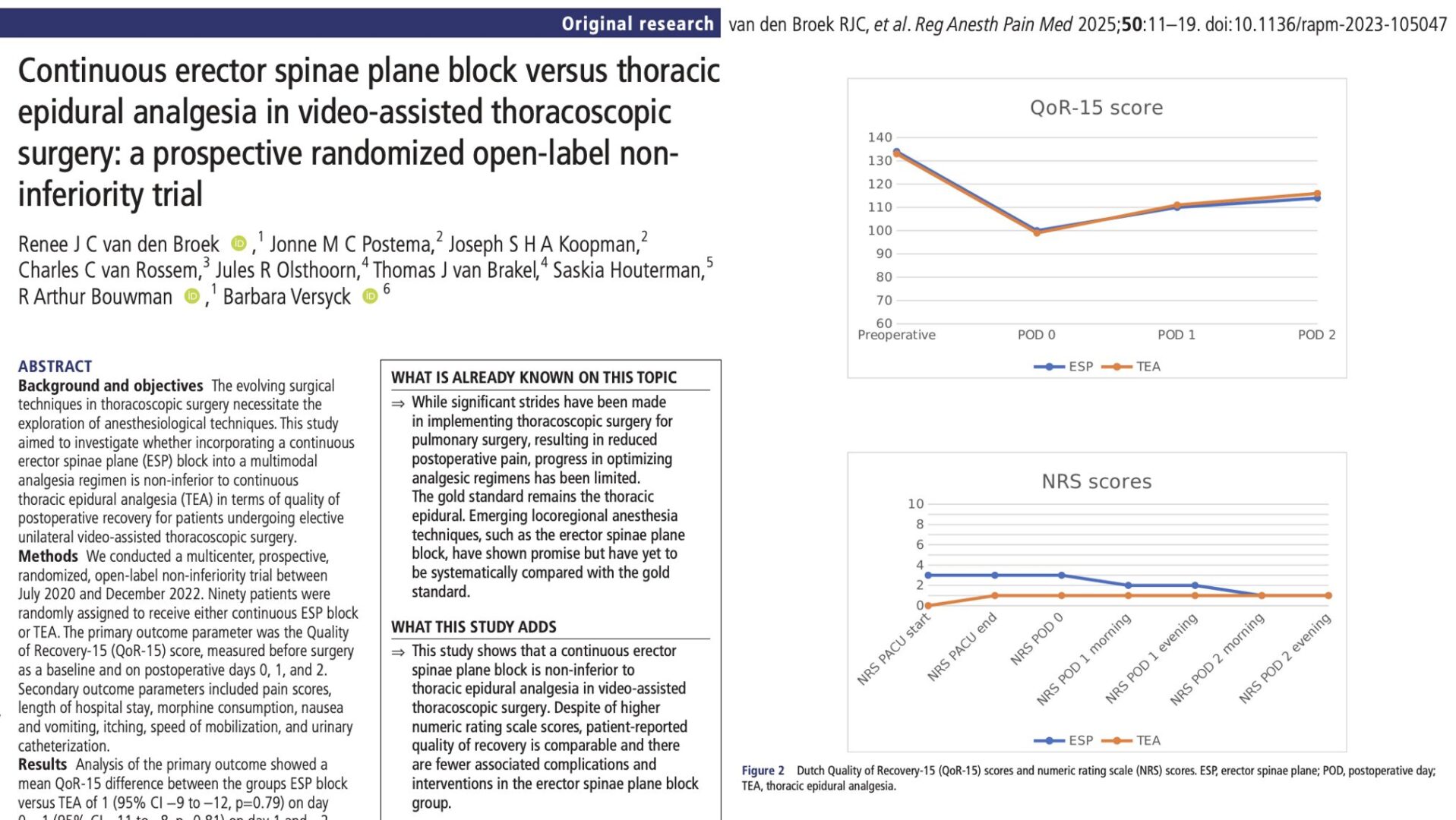
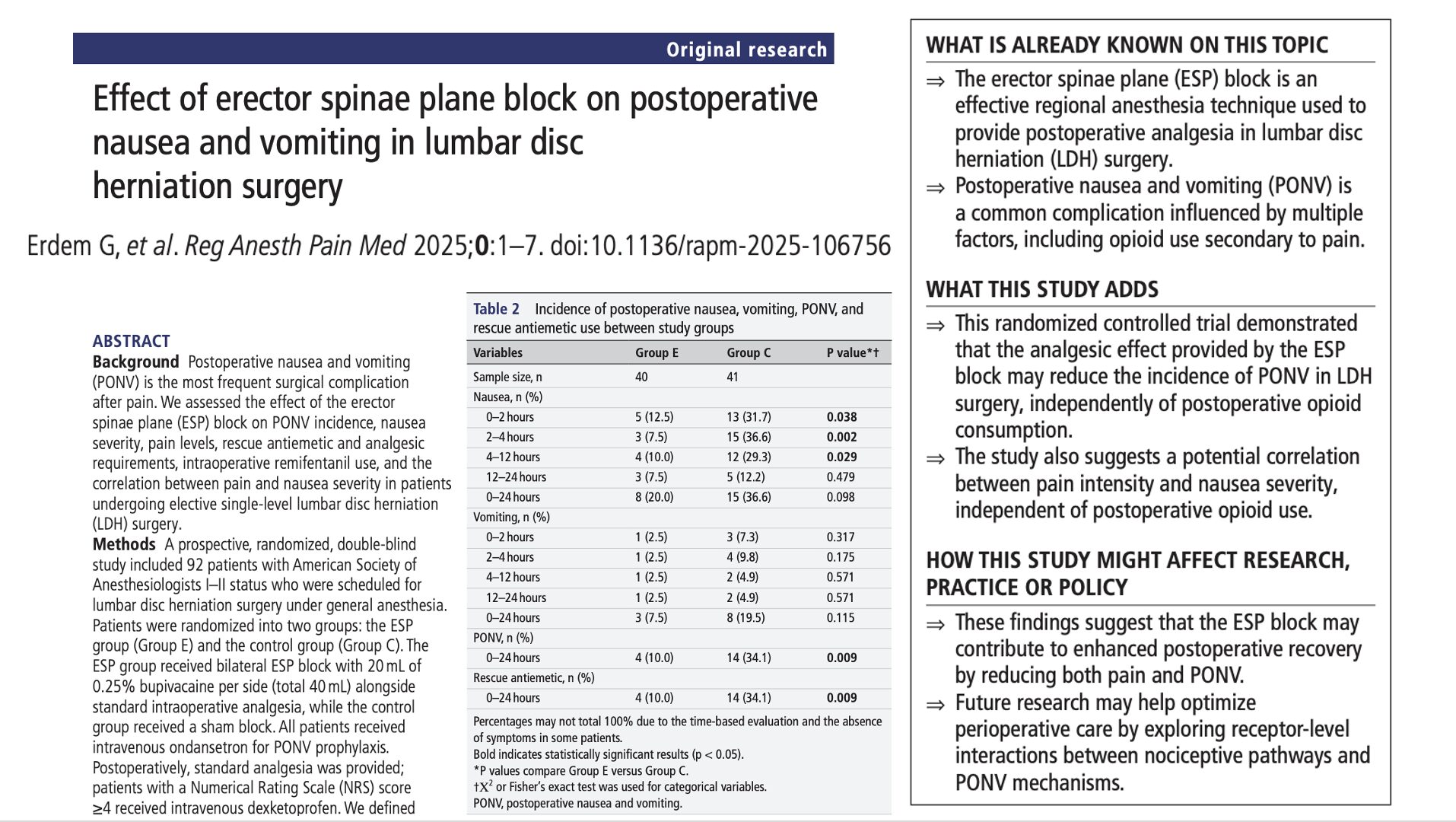
Recently, the use of regional anesthesia—particularly the paravertebral block (PVB) and erector spinae plane (ESP) blocks—has gained popularity in breast surgery. These techniques promise improved analgesia, reduced opioid use, and improved recovery. While prior studies have examined their utility in implant-based reconstruction, limited data exist on their effectiveness in autologous breast reconstruction. This study aimed to fill that gap.
Study objective and methods
This retrospective cohort study evaluated the impact of PVB and ESP blocks compared to local infiltration analgesia on postoperative outcomes in women undergoing mastectomy with latissimus dorsi flap reconstruction.
Participants:
122 patients who underwent surgery from January 2018 to February 2022 were included. Patients were grouped as follows:
- No block (local infiltration): n = 72
- Paravertebral block (PVB): n = 26
- Erector spinae plane block (ESP): n = 24
Patients receiving other block types (e.g., serratus, pectoral, or epidural) or combinations of blocks and local infiltration were excluded.
Techniques:
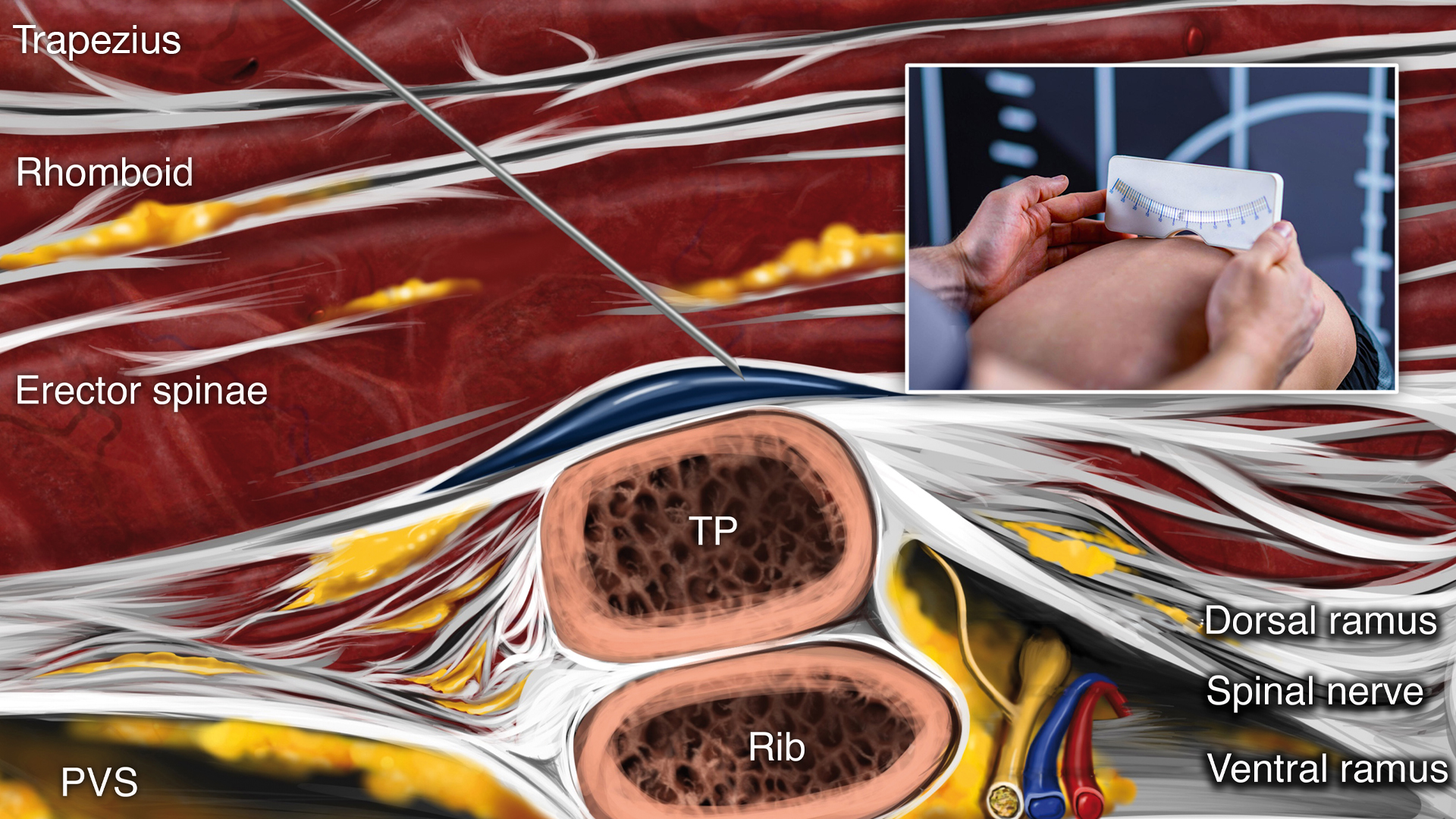
- PVB: Performed preoperatively at T4, T7, and T10 using a high-frequency linear ultrasound transducer, with 10 mL of bupivacaine or ropivacaine injected per level.
- ESP: Similar level injections deep to the erector spinae muscle and above the transverse process.
- Both blocks included adjuvants (dexamethasone and clonidine) to prolong the analgesic effect.
Outcomes:
- Primary: Postoperative length of stay (LOS) from PACU entry to discharge.
- Secondary: Postoperative pain scores, intra- and postoperative opioid use (measured in morphine milligram equivalents, MMEs), time to first analgesic, and need for postoperative antiemetics.
Key findings
- Length of stay (LOS): Patients who received either a PVB or ESP block had a significantly shorter hospital stay, with a median LOS of 26 hours in both groups compared to 48 hours in the local infiltration group. After adjusting for confounding factors, PVB was associated with a 20-hour reduction in LOS (p < 0.001), while ESP reduced LOS by 24 hours (p < 0.001).
- Intraoperative opioid use: Both regional blocks led to a similar and significant reduction in intraoperative opioid requirements. Patients in the PVB and ESP groups received 23 mg less MME on average compared to those who had only local infiltration (p < 0.001).
- Postoperative opioid use and pain: Although differences were not statistically significant, clinically relevant trends were observed. In the ESP group, only 12% of patients required high-dose opioids postoperatively (> 40 MMEs), compared to 31% in the local infiltration group. Additionally, patients who received a PVB had a 30% lower likelihood of experiencing severe pain (NRS scores of 9–10).
- Antiemetic use and safety: Rates of postoperative nausea and vomiting were similar across all groups, and no block-related complications were reported, confirming the safety of both techniques.
Conclusion
Replacing local infiltration with PVB or ESP blocks significantly reduced hospital stay and intraoperative opioid use in patients undergoing autologous breast reconstruction. While both techniques were similarly effective in reducing LOS, ESP blocks offer a technically simpler and potentially safer alternative to PVB, particularly in settings prioritizing outpatient surgical recovery.
These findings support the integration of regional anesthesia into multimodal analgesic protocols for breast reconstruction and suggest that ESP blocks may be suitable replacements for PVB in appropriate clinical scenarios.
Future research
Future research should focus on conducting randomized controlled trials to directly compare ESP and PVB in autologous breast reconstruction, allowing for stronger evidence of comparative efficacy. Additionally, studies assessing patient-reported outcomes—such as satisfaction, return to daily activities, and the incidence of chronic pain—would offer a more comprehensive view of long-term benefits. Evaluating the cost-effectiveness of ESP, PVB, and local infiltration, particularly in the context of ambulatory surgery, could inform clinical decision-making and resource allocation. Finally, further investigation into single-injection versus catheter-based ESP techniques is warranted, especially for patients with higher pain sensitivity or those undergoing bilateral procedures, to determine the optimal approach for sustained analgesia.
For more detailed information, refer to the full article in RAPM.
Ayyala HS et al. Paravertebral and erector spinae plane blocks decrease length of stay compared with local infiltration analgesia in autologous breast reconstruction. Reg Anesth Pain Med. 2025;50:339-344.
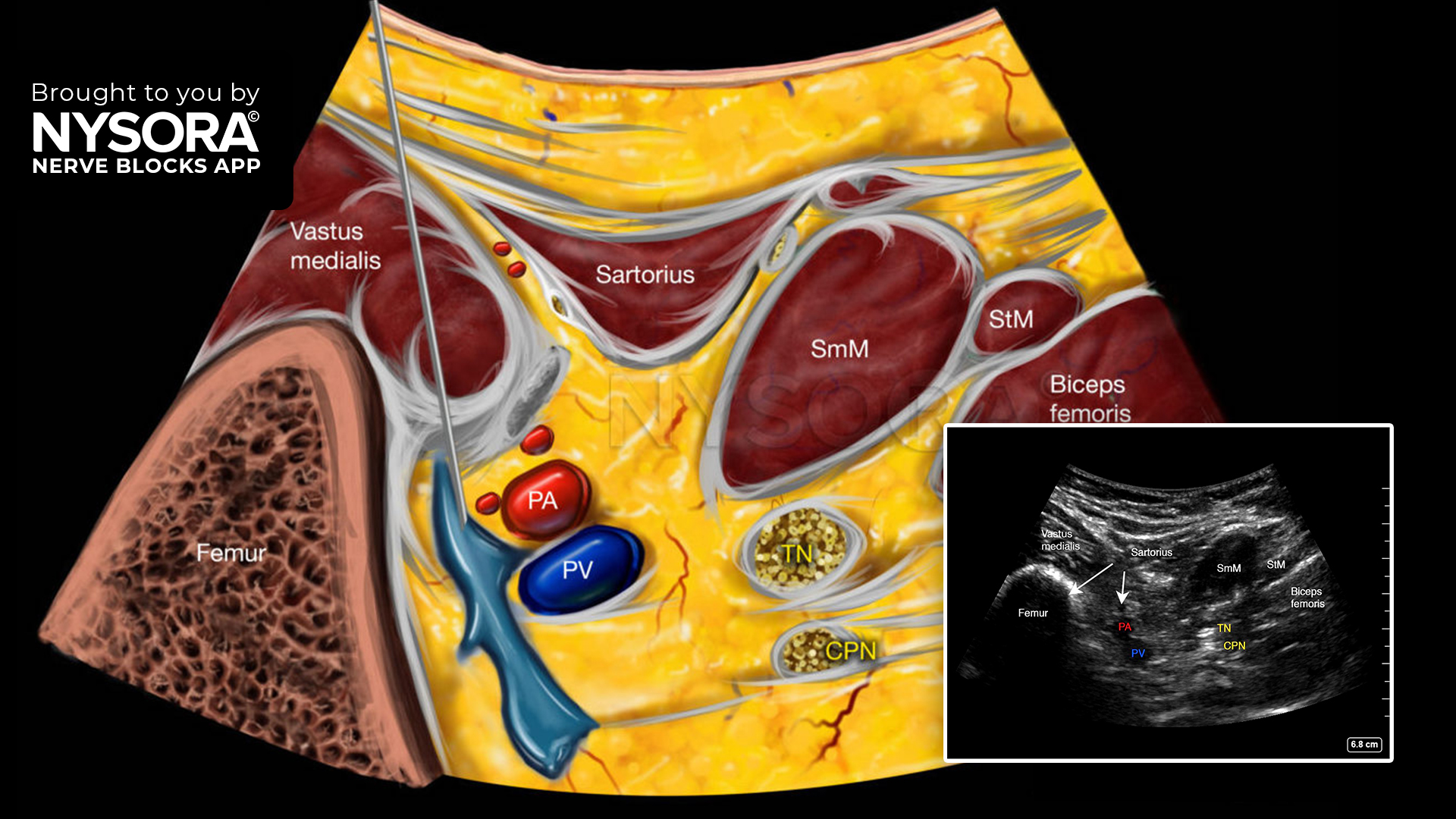
Download the Nerve Blocks App HERE for in-depth insights on the PVB and ESP blocks. Prefer a physical copy? The bestselling NYSORA Nerve Blocks App is available in book format — an essential resource for mastering nerve blocks! And for a digital learning experience, check out the Nerve Block Manual Module on NYSORA360!