Trigeminal neuralgia (TN) is a debilitating facial pain disorder characterized by severe paroxysmal facial pain that is usually unilateral and abrupt in onset and termination [1]. The pain is characterized as sharp and electric in quality. Patients often experience periods of remission and relapse [2, 3]. A trigger zone or area along part of the face may be triggered or stimulated by everyday activities such as brushing the teeth, applying cosmetics, or even speaking, eating, or feeling a breeze [2, 4]. These patients present with normal neurologic examinations TN is thought to be caused by neurovascular compression in which an aberrant vessel, normally an artery, compresses the trigeminal nerve, causing focal demyelination [5]. The current treatment model for TN generally starts with antiepileptic drugs such as carbamazepine or oxcarbazepine [2, 5]. Patients who continue to have pain or cannot tolerate the medication’s side effects often undergo microvascular decompression surgery in which the offending blood vessel is surgically separated from the trigeminal nerve and a piece of Teflon is placed between the vessel and the nerve to prevent contact and further nerve irritation [2, 4–6]. Other therapies for TN include percutaneous stereotactic neurotomy, glycerol neurotomy, percutaneous balloon compression, stereotactic radiosurgery, and peripheral trigeminal nerve injection. In the management of TN, peripheral injections have traditionally played a role in treating patients who cannot tolerate oral medications and who are not appropriate candidates for surgery. These injections have always been performed using a blind technique, with no literature reviewing their accuracy. New research using ultrasound guidance shows a 97% accuracy rate in performing ultrasound-guided supraorbital, infraorbital, and mental nerve injections [7].
1. SCANNING TECHNIQUE
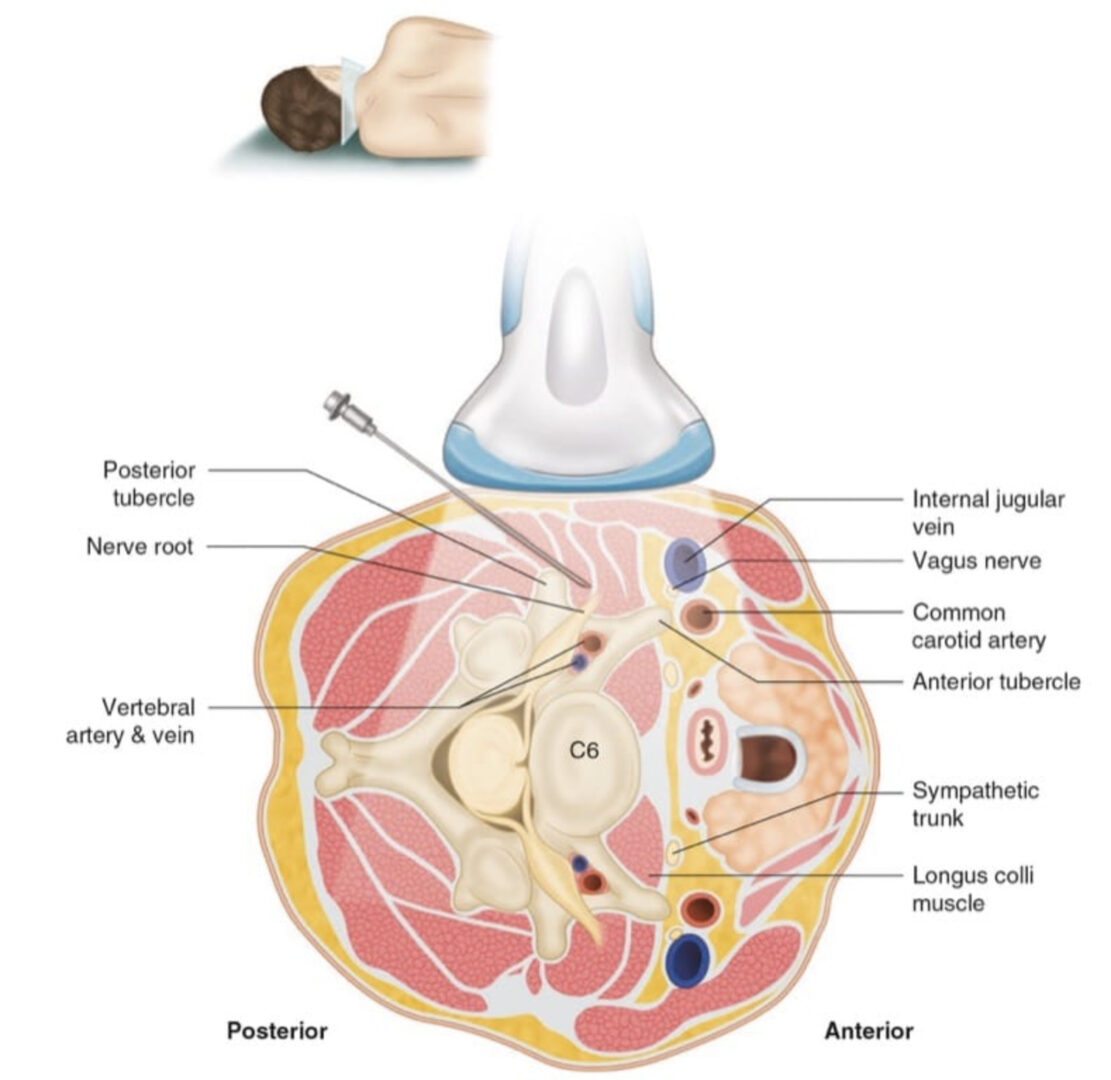
With the patient in the supine position, a pillow can be placed under the neck for comfort. A high-frequency linear transducer (10–15 MHz) is utilized to perform the examination. Scanning occurs over the superficial foramen of the desired nerve, correlating with the pain distribution pattern. The supraorbital foramen is found by placing the probe transversely over the roof of the orbital rim. The bone is scanned until a hypoechoic break identifying the foramen is located (Fig. 1). To identify the infraorbital foramen, the probe is placed in the sagittal plane just lateral to the nasal crease and scanned laterally until a hypoechoic break in the bone is identified (Fig. 2). To identify the mental foramen, the probe is placed transversely over the inferior portion of the mandible at the level of the second premolar and scanned in the cephalad direction until a hypoechoic break identifying the foramen is found (Fig. 3). The nerves and associated vessels traverse through the respective foramen. The Doppler function can be used to help identify the vasculature in close proximity to the foramen if it is difficult to find the hypoechoic break.
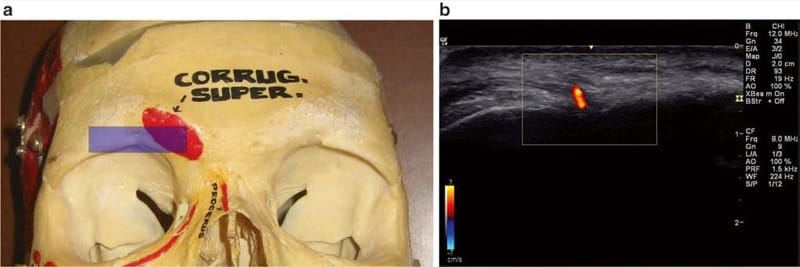
Fig.1 Scanning technique for supraorbital nerve injection (a) Transverse (axial) position of the transducer (semitransparent color rectangle), (b) Doppler mode identifying vessel
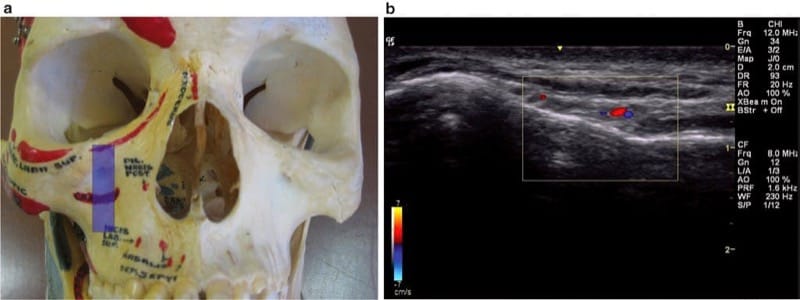
Fig.2 Scanning technique for infraorbital nerve injection (a) Sagittal position of the transducer (semitransparent color rectangle), (b) Doppler mode identifying vessel
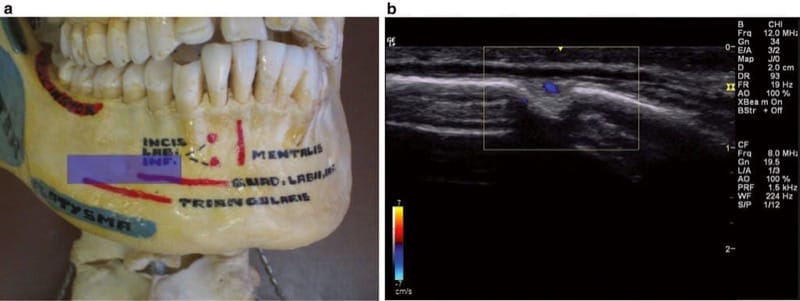
Fig.3 Scanning technique for mental nerve injection (a) Transverse (axial) position of the transducer (semitransparent color rectangle), (b) Doppler mode identifying vessel
2. ULTRASOUND-GUIDED INJECTION TECHNIQUE FOR SUPERFICIAL TRIGEMINAL NERVES
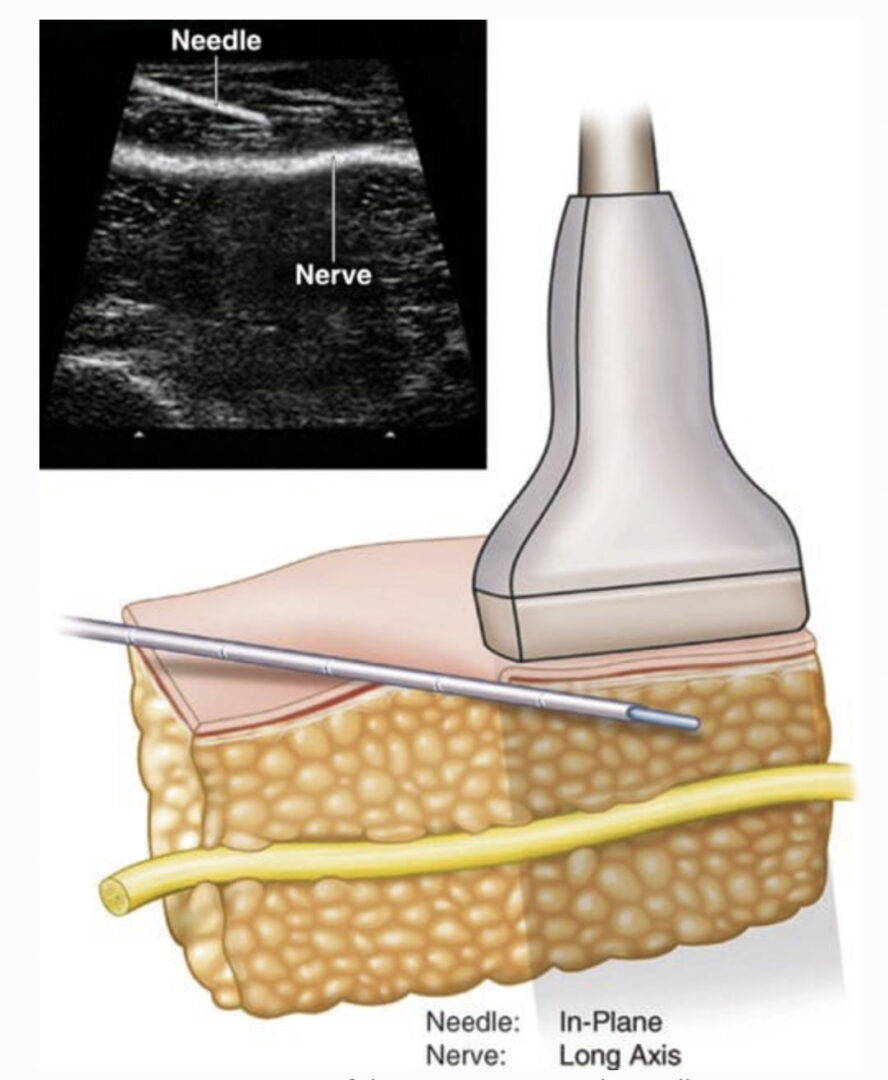
The patient position and setup are the same as for the scanning technique. Once the desired location is identified, mark and disinfect the area with appropriate sterile technique. No monitors or intravenous access is required. Injections in all sites can be performed via an in-plane or out-of-plane technique (Figs. 4, 5 and 6). Color Doppler at all three foramina will help to delineate the foramen and adjacent nerve and help to plan an injection without vessel injury. A 25- or 27-gauge, 1-inch needle with the desired injectate is utilized. A gel standoff technique may be helpful, given the superficial nature of the structures.
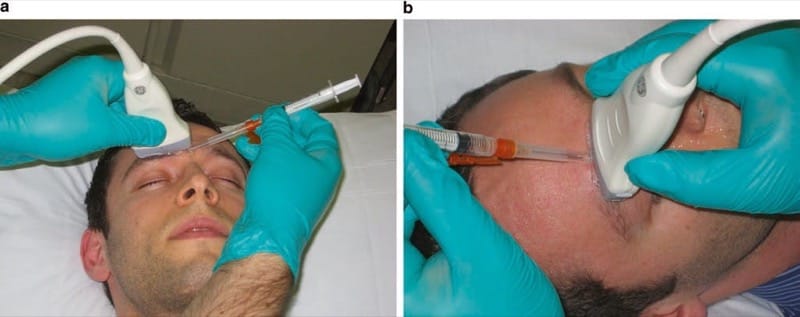
Fig.4 Ultrasound-guided supraorbital nerve injection technique (a) Example of in-plane needle position, (b) example of out-of-plane needle position
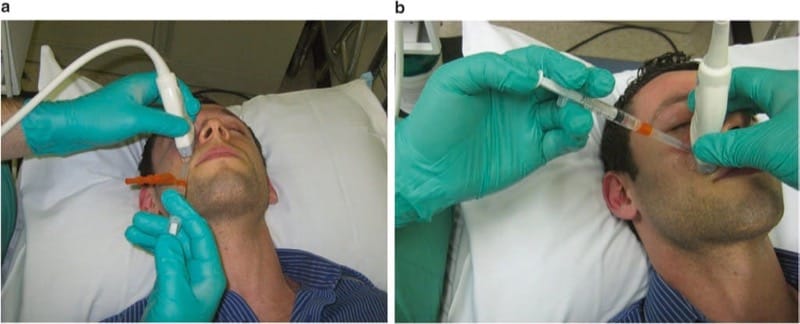
Fig.5 Ultrasound-guided infraorbital nerve injection technique (a) Example of in-plane needle position, (b) example of out-of-plane needle position
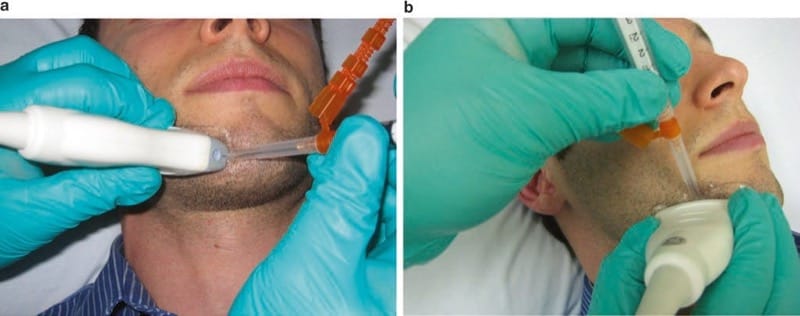
Fig.6 Ultrasound-guided mental nerve injection technique (a) Example of in-plane needle position, (b) example of out-of-plane needle position
3. CONCLUSIONS
A person affected by TN going through a painful crisis can find it nearly impossible to eat, drink, sleep, or work. His or her overall quality of life and daily functioning are significantly reduced. Though oral medications and surgery do provide relief for many patients, neurosurgical intervention is not suitable for some. For these patients, peripheral nerve injections become an important part of disease management.
Patient satisfaction with peripheral alcohol injections is high, with most patients reporting that they would be willing to undergo further injections when the pain returns [8]. There is literature supporting successful peripheral alcohol injection, but it is unclear why a percentage of patients find these injections ineffective [3]. Shah et al. give as probable reasons for ineffectiveness anatomical variations in the nerve, uncooperative behavior of patients, and faulty technique [3]. Reported complications of blind injections include soreness, infection, swelling, dysesthesia, and headache [3]. A recent study by Spinner and Kirschner shows accuracy rates of 97% for superficial supraorbital, infraorbital, and mental nerve injections; the result may be increased effectiveness of injections and decreased complications [7].