Trigeminal neuralgia (TN), often described as one of the most agonizing pain syndromes, can severely impact quality of life. Known colloquially as the “suicide disease,” TN causes debilitating, electric-shock-like facial pain, often refractory to standard medical treatment. When conservative options fail, interventional therapies become necessary. Among these, pulsed radiofrequency (PRF) of the Gasserian ganglion has emerged as a promising, minimally invasive treatment with a favorable safety profile.
What is trigeminal neuralgia?
Trigeminal neuralgia is a chronic neuropathic pain disorder affecting the trigeminal nerve (cranial nerve V), which supplies sensation to the face. TN typically presents with:
- Sudden, severe, lancinating facial pain
- Pain episodes lasting seconds to minutes
- Unilateral involvement
- Triggering by light touch, talking, or chewing
Subtypes of TN
The International Headache Society classifies TN into:
- Classic TN: Often caused by vascular compression of the nerve root.
- Secondary TN: Related to multiple sclerosis or space-occupying lesions.
- Atypical TN: Includes persistent background pain with paroxysms.
Conventional treatment approaches and their drawbacks
Pharmacologic therapy, usually with carbamazepine or oxcarbazepine, is first-line but may fail due to insufficient pain control or side effects. Surgical options include:
- Microvascular decompression (MVD): Invasive but effective for younger patients.
- Radiofrequency (RF) thermocoagulation: Destroys nerve fibers but carries risks like facial numbness and dysesthesia.
- Balloon compression and glycerol rhizotomy: Effective but neurodestructive.
While effective, these invasive procedures can produce serious adverse effects, especially in elderly or medically fragile patients.
Pulsed radiofrequency: a safer alternative
Pulsed radiofrequency (PRF) delivers short bursts of high-frequency current with long intervals between pulses, allowing tissue to cool. Unlike conventional RF, PRF does not destroy nerve tissue, making it a neuromodulatory rather than neurodestructive approach.
Key benefits
- Reduces the risk of permanent sensory loss
- Minimizes motor dysfunction
- Can be repeated if necessary
- Suitable for patients with multiple sclerosis or other conditions involving nerve sensitivity
The PROGRESS trial
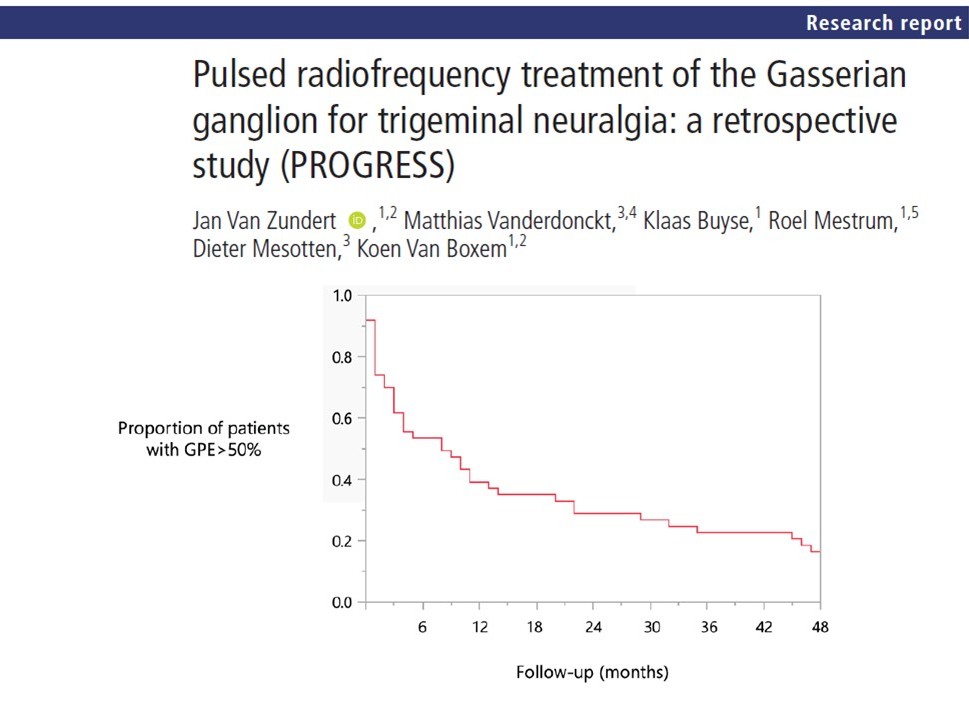
A 2025 retrospective study titled “Pulsed Radiofrequency Treatment of the Gasserian Ganglion for Trigeminal Neuralgia: a retrospective study (PROGRESS)” offers valuable insights into PRF’s effectiveness and safety.
Study design
- Setting: Tertiary referral pain center in Belgium
- Duration: 2014–2021
- Participants: 81 patients with medication-resistant TN
- Procedure: Single PRF session targeting the Gasserian ganglion
Procedure protocol
- Patient preparation: Supine positioning under sedation.
- Fluoroscopic guidance: C-arm rotated to visualize the foramen ovale.
- Needle insertion: A 10-cm thermocouple electrode is advanced into Meckel’s cavity.
- Localization: Stimulation at the V1, V2, or V3 branches to confirm correct positioning.
- PRF application: 240 seconds of pulsed current delivered.
The method ensures precise targeting and minimizes damage to surrounding structures.
Study findings: Is PRF effective?
Pain relief outcomes
- Clinical success rate: 61% of patients achieved ≥50% pain reduction at 6 weeks.
- Average pain reduction: NRS score dropped from 8.51 to 4.38.
- Duration of relief: Average 8 months, with some lasting up to 4 years.
- Long-term success: 14% maintained meaningful pain relief at 4 years.
Patient demographics
- Mean age: 64.8 years
- Gender: 58% female
- Side affected: 59% right, 41% left
- Most affected nerve branch: V2 (77%)
Prior interventions
- 22% had undergone previous MVD
- 14% had multiple sclerosis
- Some received cryotherapy or topical capsaicin
- Safety and adverse events
One patient experienced transient dysesthesia that resolved within three months. No serious complications, such as anesthesia dolorosa or corneal damage, were reported. This supports PRF’s superior safety profile compared to conventional RF.
Comparison with other studies
PRF efficacy in other research
- Zipu et al. (2021): 75% initial efficacy; sustained results over years.
- Chua et al. (2012): >80% pain relief in 73% of patients at 2 months.
Conventional RF (CRF) outcomes
- Kanpolat et al.: 97.6% initial relief, but 42.3% recurrence over 5 years.
- CRF was associated with higher rates of sensory deficits: up to 40% numbness at 3 months, declining to 18.7% at one year.
Head-to-head comparisons
- Erdine et al.: CRF more effective than PRF, but 5% of CRF patients developed anesthesia dolorosa.
- Agarwal et al.: CRF provided stronger pain control, but 25% experienced hypoesthesia vs. none in PRF group.
Special considerations for MS patients
Patients with multiple sclerosis are at higher risk of nerve injury. In this study:
- PRF was selected over CRF to avoid worsening demyelination.
- MS patients responded similarly to the general cohort.
- No increase in adverse effects was observed.
This makes PRF particularly suited for neurologically vulnerable populations.
Clinical implications: When to consider PRF
Ideal candidates
- Patients unresponsive to medication
- Patients unsuitable for surgery
Those with comorbid conditions like MS - Individuals concerned about sensory side effects
Benefits over surgery
- Outpatient procedure
- Lower complication rates
- Repeatable with minimal risk
- Rapid recovery and symptom improvement
Practical guide: steps to implement PRF in your clinic
- Patient selection: Identify TN patients refractory to medication.
- Pre-procedure imaging: Consider MRI to rule out secondary causes.
- Informed consent: Discuss benefits and potential risks.
- Procedure setup: Use fluoroscopy for needle guidance.
- Post-procedure care: Schedule follow-up at 6 weeks and 6 months.
Limitations and research gaps
- Retrospective design limits causality inference.
- Incomplete analgesic data post-procedure.
- No standardized post-treatment analgesic weaning protocol.
- Future randomized controlled trials are needed to compare PRF with CRF and surgical options in diverse populations.
Conclusion: a forward step in trigeminal neuralgia care
The PROGRESS study confirms that pulsed radiofrequency of the Gasserian ganglion is a safe, effective, and repeatable treatment for trigeminal neuralgia. Especially valuable in high-risk or elderly patients, PRF bridges the gap between conservative and invasive therapies.
With minimal risk and respectable long-term outcomes, PRF deserves a central role in the interventional management of TN.
For more information, refer to the full article in RAPM
Van Zundert J, Vanderdonckt M, Buyse K, Mestrum R, Mesotten D, Van Boxem K. Pulsed radiofrequency treatment of the Gasserian ganglion for trigeminal neuralgia: a retrospective study (PROGRESS). Regional Anesthesia & Pain Medicine. 2025;50(5):449.
Read more about the latest impactful research in pain medicine in Pain Medicine Updates 2025!