In a new 2025 meta-analysis published in Anesthesia & Analgesia by Gu et al., researchers examined a pressing question in critical care medicine: does high arterial oxygen concentration (hyperoxia) during extracorporeal membrane oxygenation (ECMO) influence survival outcomes?
With the use of ECMO expanding significantly in recent years, particularly during the COVID-19 pandemic, understanding how to manage oxygenation in these critically ill patients safely is paramount. This analysis, involving over 17,000 patients, provides vital evidence that could significantly impact clinical practice in intensive care units worldwide.
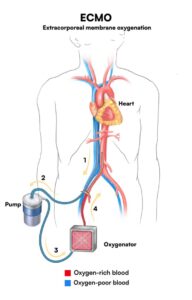
What is ECMO, and why do oxygen levels matter
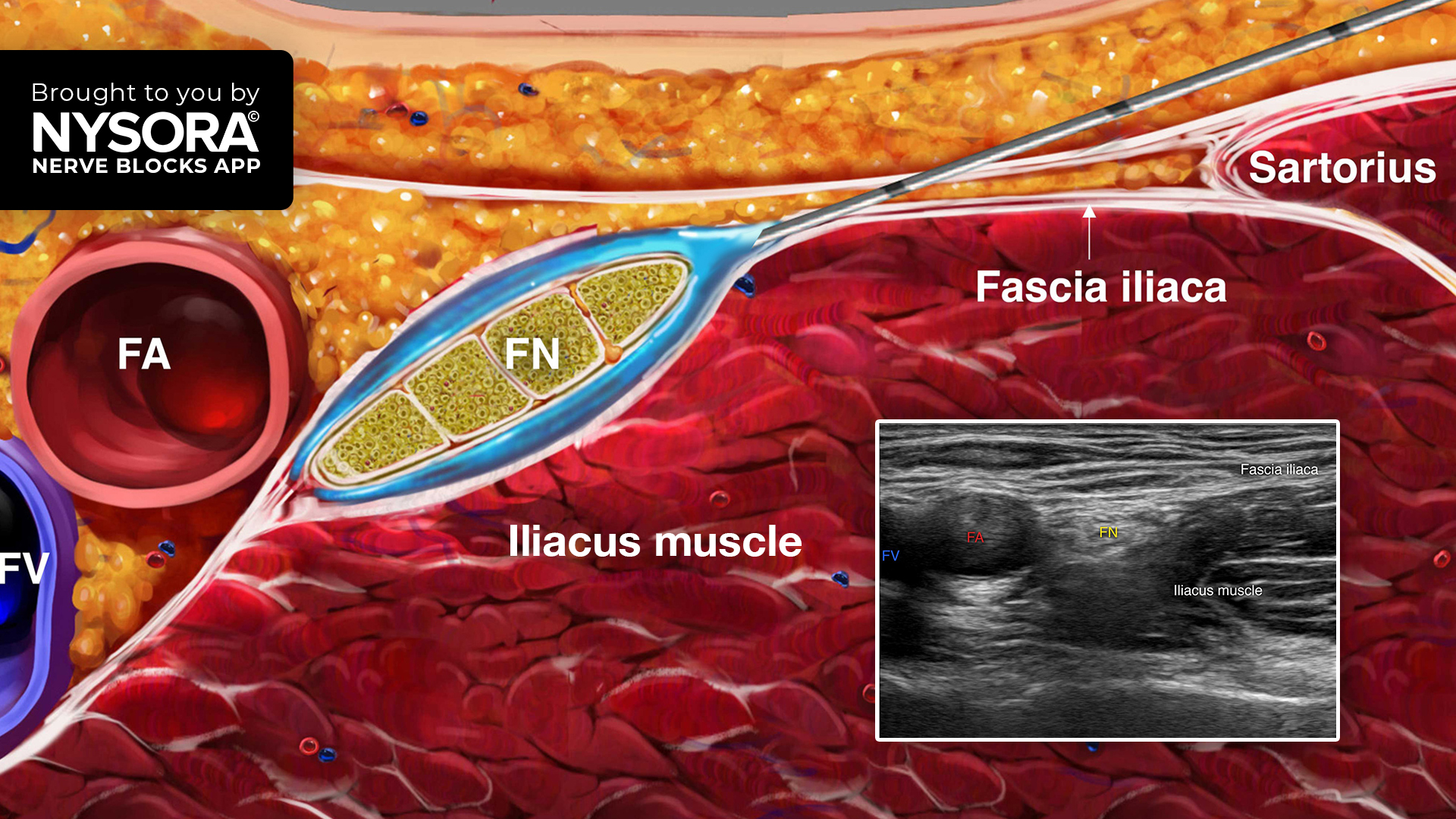
Extracorporeal membrane oxygenation (ECMO) is a form of advanced life support used in patients experiencing severe cardiac or respiratory failure. ECMO works by pumping blood outside the patient’s body to a machine that removes carbon dioxide and adds oxygen, then returning the oxygen-rich blood to the body.
There are two main types:
- Venoarterial ECMO (VA-ECMO): supports both heart and lung function.
- Venovenous ECMO (VV-ECMO): supports only lung function.
Hyperoxia refers to excessively high levels of oxygen in the blood. While oxygen is essential for survival, supraphysiological oxygen levels can be harmful. On ECMO, hyperoxia often occurs because oxygenation is aggressively managed, particularly in life-threatening conditions.
Key findings from the study
This systematic review and meta-analysis included 13 observational studies published between 2017 and 2023. These studies collectively involved 17,766 patients, making this one of the most comprehensive evaluations to date on this topic.
Important results:
-
Consistent link between hyperoxia and increased mortality:
- Pao₂ ≥ 300 mm Hg: 56% higher odds of death
- Pao₂ ≥ 200 mm Hg: 43% higher odds
- Pao₂ ≥ 150 mm Hg: 51% higher odds
- Pao₂ ≥ 100 mm Hg: 44% higher odds
- Pao₂ ≥ 300 mm Hg: 56% higher odds of death
-
Findings were robust across age groups:
- Adults: significant mortality risk at all thresholds
- Pediatrics: particularly strong association at ≥ 200 mm Hg
- Adults: significant mortality risk at all thresholds
-
The type of ECMO mattered:
- VA-ECMO and ECPR: high oxygen strongly linked with mortality
- VV-ECMO: no statistically significant association, possibly due to limited data
- VA-ECMO and ECPR: high oxygen strongly linked with mortality
How hyperoxia causes harm
Physiological mechanisms:
- Oxidative stress: Over-oxygenation leads to the excessive production of reactive oxygen species (ROS), which damage cellular components such as DNA, proteins, and lipids.
- Inflammation: Hyperoxia triggers the release of proinflammatory cytokines, contributing to systemic inflammation.
- Mitochondrial damage: Prolonged exposure to toxins damages mitochondrial function, thereby affecting cellular energy production.
- Neurological injury: High Pao₂ has been linked with increased rates of acute brain injury in ECMO patients.
- Pulmonary effects: It may exacerbate atelectasis, alveolar-capillary leakage, and lung fibrosis in patients with ARDS.
Clinical implications and best practices
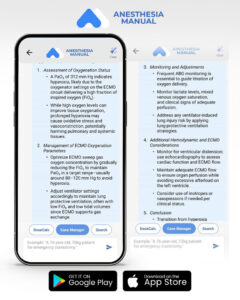
Given the association between hyperoxia and poor outcomes, clinicians are urged to reconsider current oxygenation strategies in ECMO patients.
Clinical recommendations:
- Avoid targeting supraphysiological Pao₂ levels.
- Use conservative oxygen strategies, titrating to the lowest level needed to maintain adequate tissue oxygenation.
- Monitor oxygen levels closely with frequent arterial blood gas analyses.
- Adopt individualized oxygen targets based on patient condition, type of ECMO, and response to therapy.
- Educate critical care teams about the potential harms of hyperoxia and the importance of targeted oxygen management.
These approaches align with the ELSO Interim Guidelines, which recommend avoiding both hypoxia and hyperoxia in ECMO-supported cardiac patients.
Conclusion
This landmark meta-analysis highlights the importance of cautious oxygen management in patients supported by ECMO. Arterial hyperoxia is associated with higher mortality, particularly at levels above 200 mm Hg, and affects both adults and children. While more rigorous studies are needed to establish causality, the evidence is sufficient to inform practice today.
In critical care, sometimes less is more; even when it comes to oxygen.
Reference: Gu W. et al. Association Between Arterial Hyperoxia and Mortality in Pediatric and Adult Patients Undergoing Extracorporeal Membrane Oxygenation: A Systematic Review and Meta-Analysis. Anesthesia & Analgesia. 2025;140:1367-1376.
For more information on ECMO and new guidelines, check out Anesthesia Updates on the NYSORA Anesthesia Manual App.
Get access to step-by-step management algorithms, the latest research, and peer-reviewed insights—all in one place. Download the app today and experience the future of anesthesia education and decision-making.
AI on call: Case of the week
A 58-year-old man is placed on VA-ECMO after cardiac arrest from a massive MI. His initial ABG shows a Pao₂ of 312 mm Hg.