Understanding gastric emptying in pregnancy is critical for anesthesia providers, particularly for obstetric procedures. A recent narrative review published in the British Journal of Anaesthesia by Lawson et al. (2025) explores how pregnancy affects gastric emptying and its implications for anesthetic practice.
Why This Topic Deserves Your Focus
Pulmonary aspiration remains a serious risk during anesthesia for Caesarean delivery and labor, often due to delayed gastric emptying. Traditional fasting guidelines are based on assumptions about delayed gastric emptying in pregnancy, but how accurate are these assumptions? This review analyzed 55 studies, including 32 observational studies and 22 randomized controlled trials, to clarify gastric emptying patterns in pregnancy and labor.
How the Authors Did the Study
The review assessed gastric emptying of solids and liquids across different trimesters, during labor, before Caesarean delivery, and postpartum. Methods of evaluating gastric emptying included:
- Gastric ultrasound (most common)
- Paracetamol absorption tests
- Scintigraphy (gold standard but less frequently used)
- Breath hydrogen analysis
The authors also examined the effects of analgesia (epidural vs. opioids), fasting durations, and pharmacological interventions (prokinetics like metoclopramide and antiemetics like granisetron).
What the Authors Found
- First trimester: Gastric emptying is delayed compared to nonpregnant women.
- Second and third trimesters: Gastric emptying returns to normal and is comparable to nonpregnant individuals.
- Labor: Gastric emptying slows significantly, especially if opioids are used.
- Epidural analgesia: Partially improves gastric emptying but does not restore it to baseline.
- Intrathecal opioids: Delay gastric emptying more than epidurals alone.
- Elective Caesarean section:
- Carbohydrate drinks or tea with milk 2 hours before surgery do not increase gastric volumes compared to fasting.
- Some patients still have “high-risk” gastric contents despite standard fasting.
Postpartum period: Conflicting evidence exists, but most studies suggest a gradual return to normal gastric function.
Breaking It Down
The study confirms that gastric emptying is unpredictable in pregnancy, especially in labor. The longstanding assumption that all pregnant women have delayed gastric emptying is only true in labor and early pregnancy. This means some fasting guidelines may need reassessment.
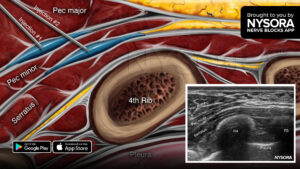
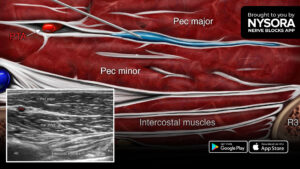
Notably, gastric ultrasound can be a valuable bedside tool for individualizing fasting and aspiration risk assessments.
The findings also support the use of carbohydrate-rich fluids before elective Caesarean delivery, challenging traditional prolonged fasting practices.
The Takeaway
- Gastric emptying is not universally delayed in pregnancy—the first trimester and labor are the most affected.
- Systemic opioids slow gastric emptying; epidural analgesia helps but does not restore it completely.
- Gastric ultrasound could be a useful tool to assess individual aspiration risk.
- The Sip-Til-Send approach (allowing sips of water up to surgery) appears safe in elective cases.
Carbohydrate drinks and tea with milk do not significantly increase gastric volume, suggesting potentially more liberal preoperative fluid intake could be safe.
Practical Recommendations for Clinicians
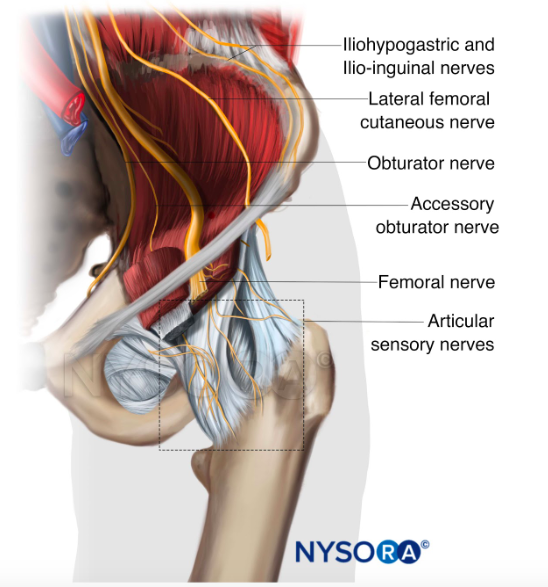
- Consider gastric ultrasound to assess individual aspiration risk rather than relying on universal fasting guidelines.
- Encourage epidural analgesia over systemic opioids in labor to reduce gastric stasis.
- Avoid prolonged fasting before elective Caesarean delivery—carbohydrate drinks or tea with milk may be safe alternatives.
- For emergency cases, assume delayed gastric emptying and manage accordingly with rapid-sequence induction.
- Monitor postpartum patients individually, as gastric function recovery is variable.
Final Thoughts
This review challenges traditional assumptions about gastric emptying in pregnancy and suggests a more individualized approach to fasting and aspiration risk. Incorporating gastric ultrasound and updated fasting practices could improve patient safety and comfort during obstetric anesthesia.
Join NYSORA’s newsletter for anesthesiology updates, case studies, and expert insights—delivered first, straight to your inbox!
Reference:
Lawson J, Howle R, Popivanov P, et al. Gastric emptying in pregnancy and its clinical implications: a narrative review. Br J Anaesth. 2025;134(1):124-167.