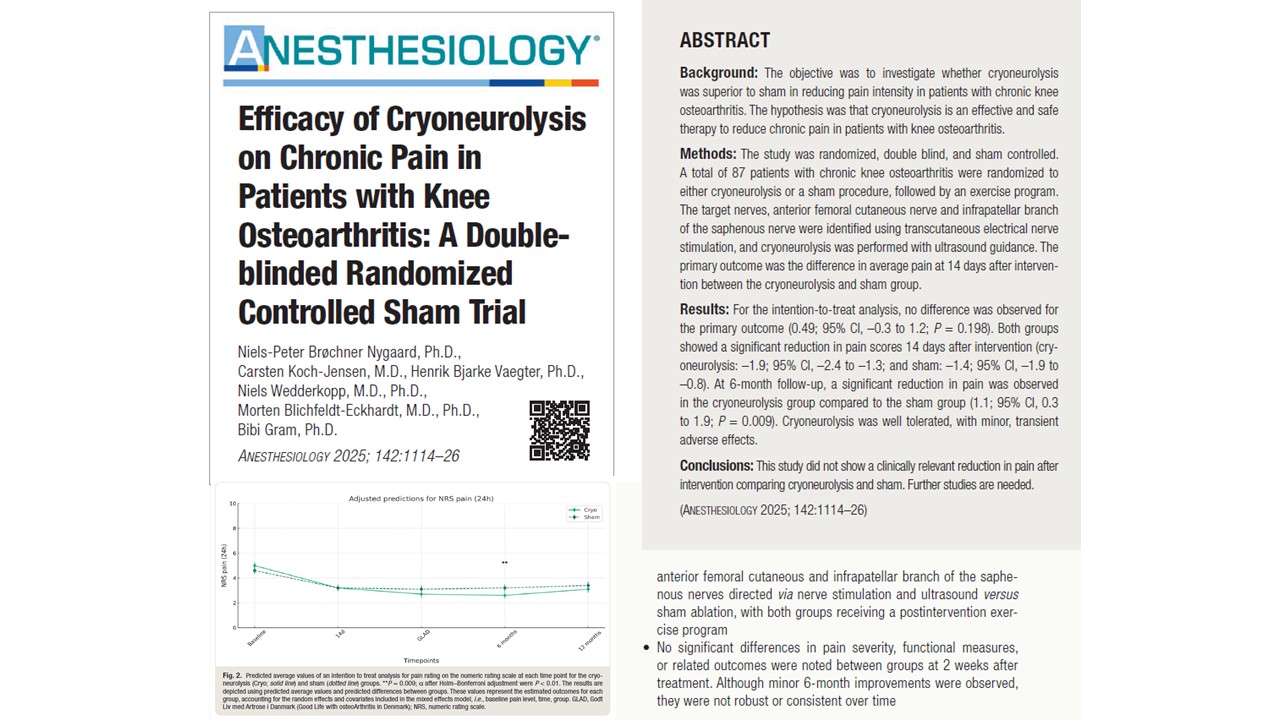
Cryoneurolysis, a technique that destroys peripheral nerve fibers using extreme cold, has seen renewed interest as a potential option for managing chronic non-cancer pain. Although the procedure has been in clinical use for decades, technological advancements and improved guidance methods, such as ultrasound and computed tomography (CT), have allowed for more accurate, controlled applications. Now, a 2025 systematic review and meta-analysis by Nygaard et al. published in Anesthesiology, offers a comprehensive evaluation of this therapy’s efficacy, safety, and clinical utility across a variety of chronic pain conditions.
By aggregating data from multiple studies, this review aims to clarify whether cryoneurolysis is a viable intervention for patients who suffer from persistent pain not related to malignancy. The findings suggest meaningful reductions in pain intensity, with minimal risk of serious complications, positioning cryoneurolysis as a potentially valuable component of modern pain management strategies.
What is cryoneurolysis and how does it work?
Cryoneurolysis, also known as cryoablation or cryoanalgesia, involves applying temperatures ranging from -20°C to -100°C to peripheral nerves. This is achieved using cryoprobes that rapidly freeze the target tissue. The resulting injury causes Wallerian degeneration, a form of selective axonal destruction in which:
- Axons are temporarily disabled.
- The surrounding epineurium and perineurium (connective tissue) remain intact.
- Nerve function typically returns as regeneration occurs over weeks to months.
This mechanism differs from other neurolytic techniques, such as radiofrequency ablation (which uses heat) or chemical neurolysis (using agents like phenol or alcohol), which can cause less predictable or irreversible damage.
Advantages of cryoneurolysis include:
- A minimally invasive technique
- Reversible nerve blockade
- Repeatable treatments without cumulative damage
- Minimal disruption to surrounding structures
These features make cryoneurolysis an appealing choice for patients needing targeted, temporary pain relief.
Systematic review design
The meta-analysis incorporated clinical studies published through 2023, focusing on adult patients treated with cryoneurolysis for chronic non-cancer pain. The authors included randomized controlled trials (RCTs), prospective cohort studies, and case series with appropriate outcome measures.
Key characteristics:
- 17 studies involving 599 patients
- Pain conditions: occipital neuralgia, chronic shoulder pain, post-thoracotomy pain, lumbar facet joint pain, and others
- Techniques: Ultrasound- and CT-guided cryoneurolysis using commercial cryoprobes
- Outcome measures: Pain reduction (VAS, NRS), functional improvement, quality of life, adverse events
- Follow-up: 1 week to 6 months post-treatment
The primary outcome of interest was a reduction in pain intensity. Secondary outcomes included functional improvement and incidence of adverse events.
Efficacy of cryoneurolysis
The pooled analysis revealed that cryoneurolysis consistently resulted in significant reductions in pain intensity across various patient groups and anatomical targets.
Pain reduction
- The pooled mean reduction in pain scores was -3.38 points, with a 95% confidence interval of -4.14 to -2.61.
- Statistically significant improvements were evident as early as 1 week after the procedure.
- In some studies, pain relief persisted up to 3–6 months, although durability varied by condition and nerve treated.
Notably, conditions such as occipital neuralgia and chronic post-surgical shoulder pain showed the most robust and sustained responses.
Functional improvement
Several studies reported secondary benefits in:
- Mobility and joint function, particularly in cases of shoulder pain.
- Sleep quality and daily activity levels, particularly where pain had significantly disrupted quality of life.
However, measures of functional improvement were inconsistently reported, limiting definitive conclusions.
Safety profile
- Adverse events were rare and mild:
- Transient numbness
- Local bruising
- Mild injection site discomfort
- No reports of neuroma formation, infection, or permanent sensory loss
- Imaging guidance appeared to enhance both safety and accuracy
Overall, the favorable safety profile supports its use in outpatient and ambulatory care settings.
Limitations
Despite encouraging findings, the review highlights several limitations that temper the strength of recommendations for widespread adoption:
- Heterogeneity in study design: Differences in cryoprobe temperature, nerve target, patient diagnosis, and outcome metrics complicated direct comparisons.
- Small sample sizes: Many studies enrolled fewer than 50 participants, which limited their statistical power.
- Short follow-up durations: Few studies evaluated outcomes beyond 3 months, leaving long-term durability unclear.
- Lack of control groups: Many included studies were observational, and only a few were randomized or included sham controls.
These limitations indicate a need for more rigorous clinical trials with consistent protocols and standardized reporting.
Practical applications in chronic pain care
Given its attributes and demonstrated efficacy, cryoneurolysis may be a valuable intervention for patients who:
- Have not responded to pharmacologic treatments (e.g., opioids, NSAIDs, antidepressants).
- They are not candidates for invasive procedures or surgery.
- Require non-permanent nerve blockade to facilitate rehabilitation or recovery.
- Need repeatable treatments with minimal risk.
Important considerations for clinical use:
- Precise anatomical knowledge and imaging support (ultrasound or CT) are critical for accurate targeting.
- Patient counseling should emphasize the temporary nature of relief and the possible need for repeat procedures.
- Integration with multimodal care (physical therapy, psychological support) can improve overall outcomes.
Conditions most responsive to cryoneurolysis
The review highlights three clinical scenarios where cryoneurolysis may offer the most benefit:
- Occipital neuralgia:
- Consistent pain relief
- Quick onset of benefit
- Favorable safety with ultrasound-guided greater occipital nerve targeting
- Chronic shoulder pain (e.g., post-surgical, rotator cuff-related):
- Improved range of motion
- Reduction in nocturnal pain and dependence on medications
- Post-thoracotomy pain syndrome:
- Effective intercostal nerve blockade
- Reduction in opioid use
- Better respiratory function by alleviating pain-related splinting
Other potential areas include ilioinguinal neuralgia, lumbar facet pain, and anterior femoral cutaneous nerve entrapment, though more data are needed.
Future research
To clarify the role of cryoneurolysis in chronic pain management, future studies should aim to:
- Conduct randomized controlled trials with adequate power and blinded comparators.
- Include long-term follow-up (6–12 months) to assess recurrence and regeneration.
- Compare cryoneurolysis to other interventional techniques, such as pulsed radiofrequency or perineural corticosteroid injections.
- Evaluate cost-effectiveness and healthcare utilization, particularly for outpatient applications.
Standardized reporting frameworks for cryoneurolysis protocols, pain scales, and functional outcomes would further strengthen the evidence base.
Conclusion
Cryoneurolysis represents a promising, minimally invasive intervention for selected patients with chronic non-cancer pain. The current evidence suggests that it can provide significant, albeit temporary, pain relief with a low incidence of adverse events. While limitations in the data prevent strong clinical recommendations across all indications, the technique shows particular utility in occipital neuralgia, chronic shoulder pain, and post-thoracotomy neuralgia. As interventional pain management continues to evolve, cryoneurolysis may increasingly serve as a bridge between conservative therapy and more invasive procedures, offering patients a low-risk path to improved function and quality of life. However, broader adoption will depend on ongoing research to address knowledge gaps and validate long-term benefits in diverse populations.
For more information, refer to the full article in Anesthesiology.
Nygaard NB, Koch-Jensen C, Vaegter HB, Wedderkopp N, Blichfeldt-Eckhardt M, Gram B. Efficacy of Cryoneurolysis on Chronic Pain in Patients with Knee Osteoarthritis: A Double-blinded Randomized Controlled Sham Trial. Anesthesiology. 2025 Jun 1;142(6):1114-1126.
Read more about cryoneurolysis in the e Regional Anesthesia Module on the NYSORA360!