Chronic widespread pain (CWP), a hallmark of conditions like fibromyalgia and long COVID, has now been linked to significant increases in dementia and cognitive decline. A groundbreaking longitudinal study reveals that individuals with CWP have more than double the risk of mild cognitive impairment (MCI) and a 50% higher risk of all-cause dementia.
Key takeaways from the study
- CWP is linked to 2.5x higher odds of MCI
- 50% increase in risk for all-cause dementia
- Poorer performance in multiple cognitive domains
- Brain structural changes and inflammation partially mediate the relationship
- No strong evidence yet of a direct causal link, but compelling associations
What is chronic widespread pain?
Chronic widespread pain refers to pain that:
- Persists for more than three months
- Affects multiple areas of the body
- Is often accompanied by fatigue, psychological distress, and cognitive dysfunction
Common conditions involving CWP:
- Fibromyalgia
- Long COVID
- Rheumatoid arthritis
- Chronic fatigue syndrome
- Postsurgical and postcancer pain syndromes
Study design: a closer look
The study analyzed data from 188,594 participants from the UK Biobank over a 13-year follow-up period. Key components included:
- Pain reports categorized as: no pain, short-term pain, chronic localized pain (CLP), and CWP
- Cognitive assessments using 8 standardized tests
- Brain imaging data (MRI)
- Inflammatory biomarkers from blood samples
- Diagnosis of dementia and MCI based on ICD codes from hospital records
Major findings
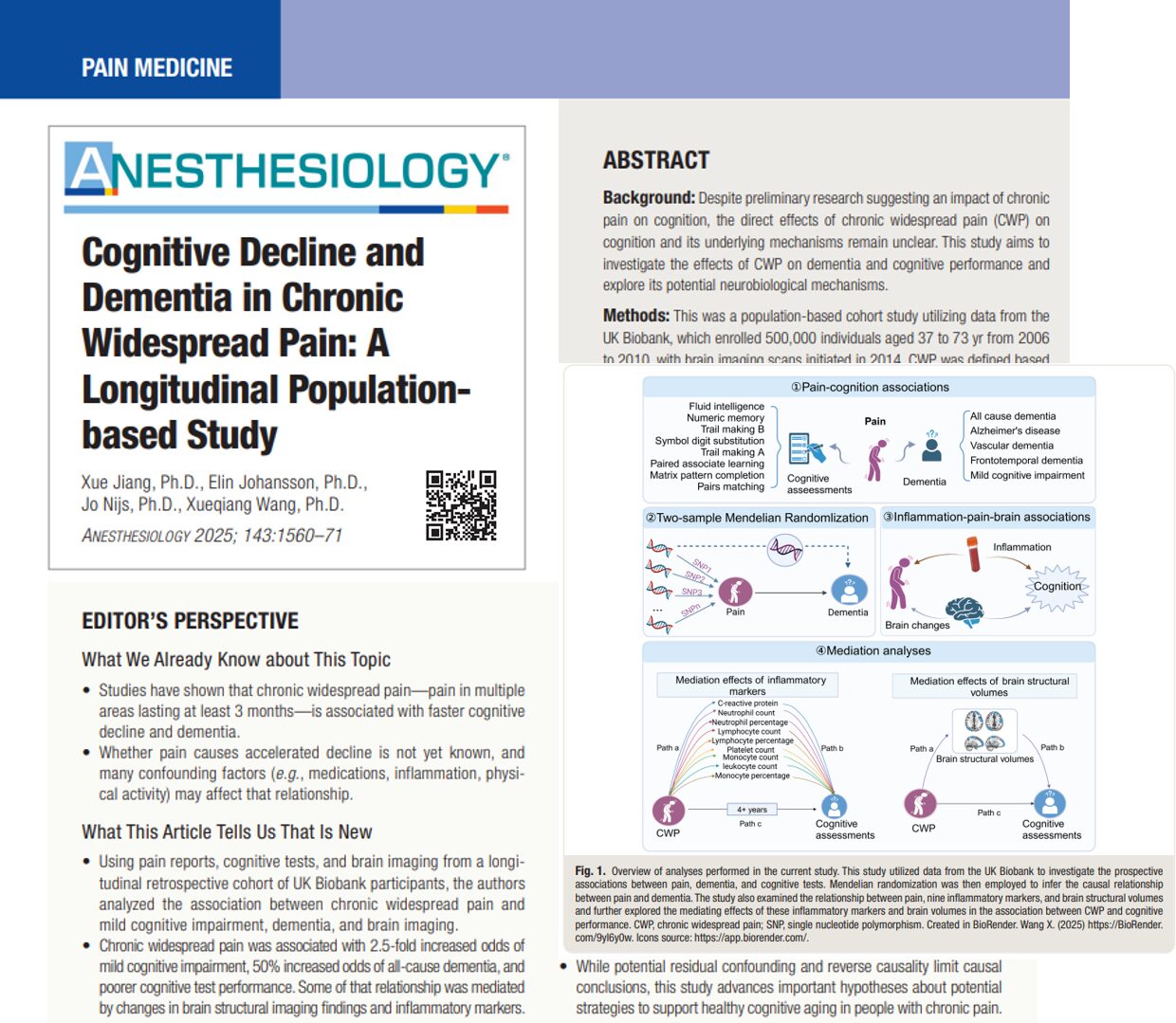
1. Risk of dementia and cognitive decline
- CWP was significantly associated with:
- 2.55x higher risk of mild cognitive impairment (MCI)
- 1.53x higher risk of all-cause dementia
- 2.55x higher risk of mild cognitive impairment (MCI)
- Risk was notably higher in men and individuals under 60 years old
- No statistically significant associations with Alzheimer’s, vascular, or frontotemporal dementia individually
2. Impaired cognitive performance
Participants with CWP showed deficits in:
- Fluid intelligence
- Trail making tests A & B (executive function, processing speed)
- Symbol digit substitution (attention, motor speed)
- Matrix pattern completion
- Pairs matching (visual memory)
Cognitive decline worsened with increasing pain duration and distribution
What brain changes are involved?
According to the MRI analysis:
- Individuals with CWP had reduced gray matter volume
- Mediation analysis revealed significant changes in:
- Prefrontal cortex
- Insular cortex
- Thalamus
- Amygdala
- Precentral/postcentral gyri
- Prefrontal cortex
Overall, gray matter volume mediated over 10% of the association between CWP and cognitive impairment.
How does inflammation factor in?
Systemic inflammation appears to play a modest but significant mediating role:
- Leukocyte and neutrophil counts were associated with poorer cognitive outcomes
- Platelet and lymphocyte levels also showed mediation effects
- These markers suggest chronic low-grade inflammation could impact brain health
However, these systemic markers accounted for only a small proportion of the effect. Future studies should consider central nervous system markers like microglial activation using PET imaging or cerebrospinal fluid analysis.
Final thoughts
This large-scale study adds to a growing body of evidence linking chronic pain and cognitive decline. It urges a paradigm shift: treating pain may not just be about comfort, but preserving brain health. Though causality remains unconfirmed, the findings support a multidisciplinary approach to managing chronic pain, including neurologic, psychiatric, and rehabilitation perspectives.
“Early identification and management of CWP may not only alleviate pain but also reduce the risk of cognitive decline and its progression to dementia.” – Jiang et al., 2025
Reference: Jiang X et al. Cognitive Decline and Dementia in Chronic Widespread Pain: A Longitudinal Population-based Study. Anesthesiology. Published online October 16, 2025.
For more information about chronic pain and dementia, get the NYSORA Anesthesia Assistant App!