Intravenous fluid therapy remains one of the most vital interventions in critical care. From trauma and sepsis to post-operative management and neurological emergencies, fluid resuscitation is a mainstay of ICU protocols. Yet, a crucial question has persisted for decades: Should we use balanced crystalloids or normal saline?
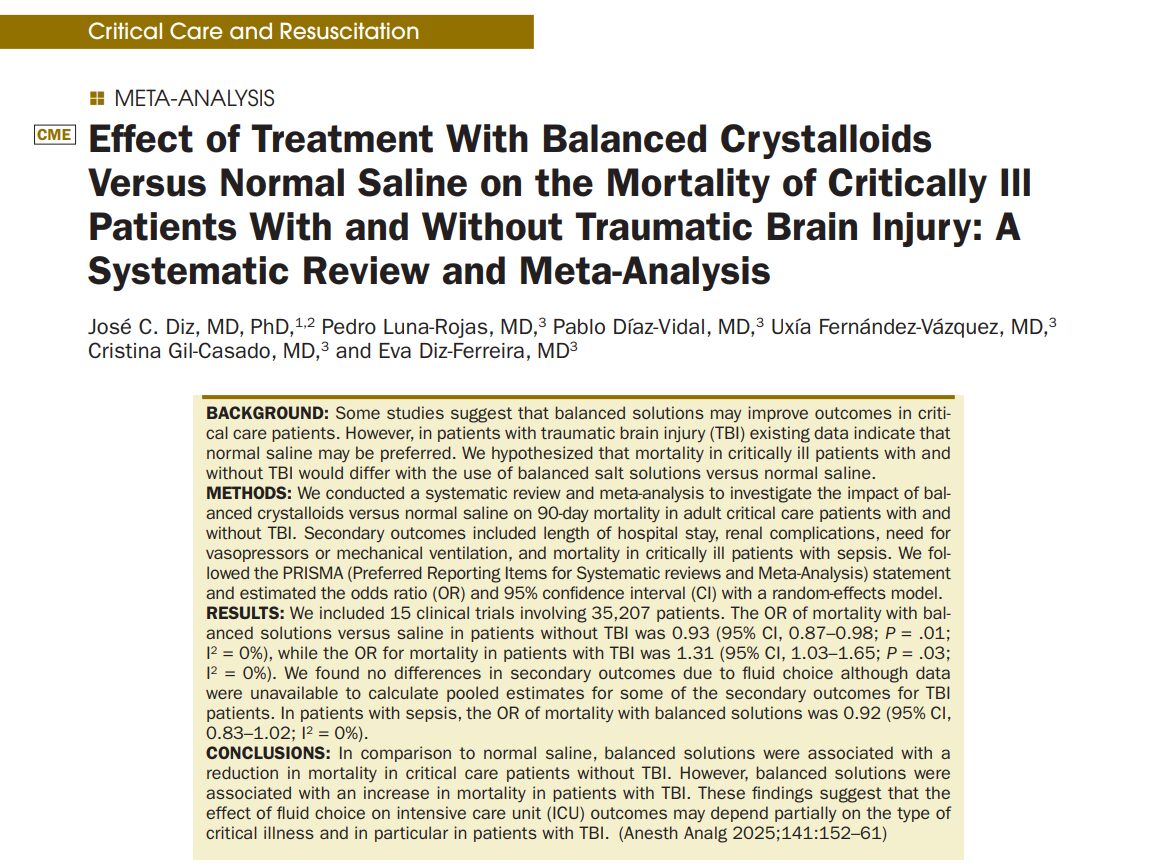
A recent meta-analysis by Diz et al., published in the July 2025 issue of Anesthesia & Analgesia, delivers some of the most comprehensive evidence to date, offering nuanced answers that could reshape fluid therapy strategies, particularly in patients with traumatic brain injury (TBI).
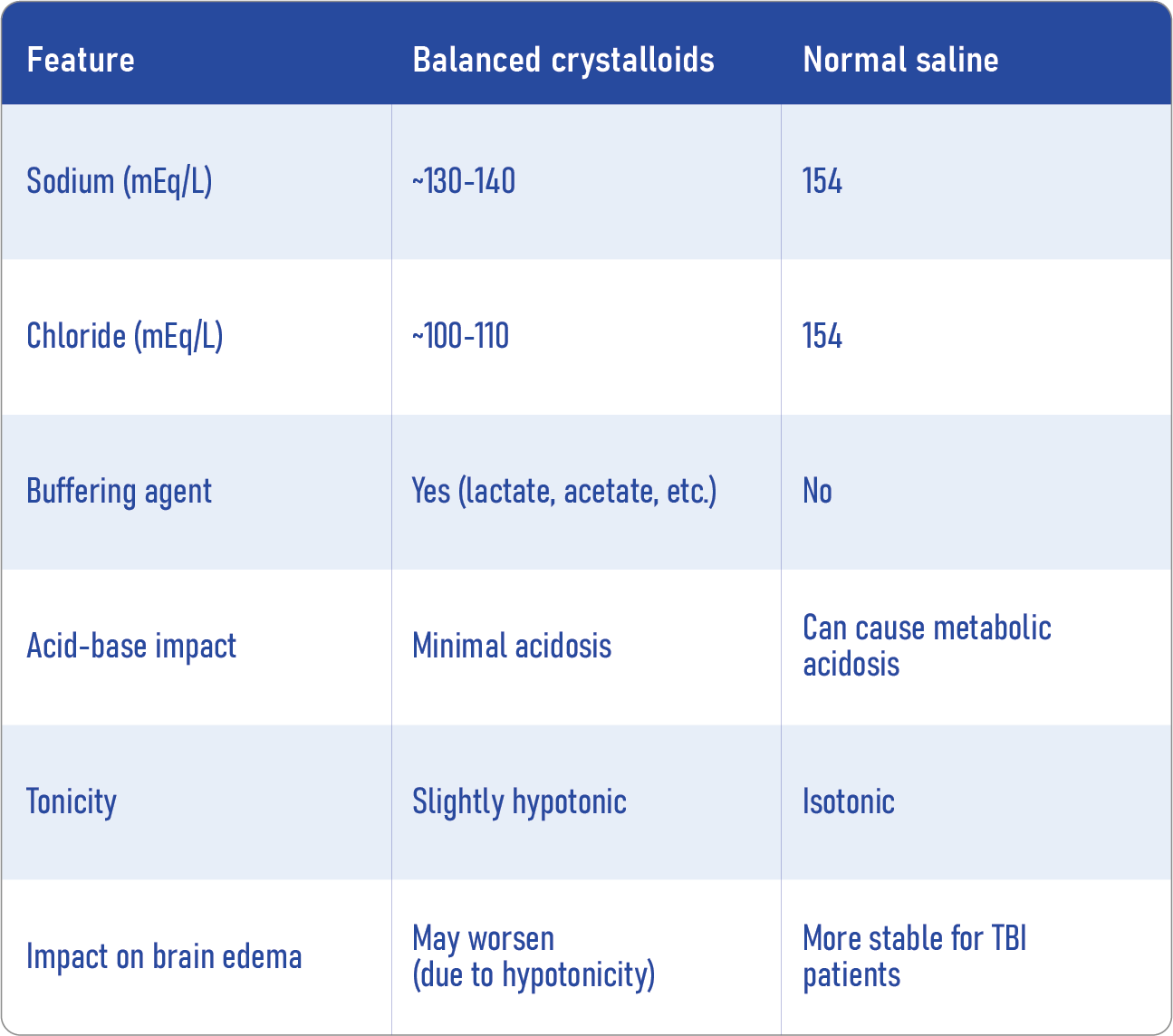
What are balanced crystalloids, and how do they compare with normal saline?
Balanced crystalloids, such as Lactated Ringer’s and Plasma-Lyte, are intravenous fluids formulated to mimic plasma’s electrolyte composition closely. They typically contain:
- Sodium
- Potassium
- Calcium (in some formulations)
- Chloride
- A buffer (lactate, acetate, or gluconate)
Normal saline (0.9% sodium chloride) is a non-balanced solution that contains a high chloride load, which can lead to hyperchloremic metabolic acidosis, particularly when administered in large volumes.
Key differences:
What did the new study investigate?
Study design:
- Systematic review and meta-analysis
- Included 15 randomized clinical trials (RCTs) with a total of 35,388 critically ill adult patients
- Compared balanced crystalloids vs. normal saline
- Primary outcome: 90-day mortality
- Secondary outcomes: renal complications, length of stay (LOS), need for vasopressors/mechanical ventilation, and subgroup mortality in sepsis and TBI
Primary findings:
- In non-TBI patients:
- Balanced crystalloids reduced mortality
- Balanced crystalloids reduced mortality
- In TBI patients:
- Balanced crystalloids increased mortality
- In patients with sepsis:
- No significant mortality difference
These findings underscore the critical importance of tailoring fluid therapy to individual patient conditions.
Subgroup analysis highlights
Non-TBI patients:
- An estimated 3–19 fewer deaths per 1000 patients when using balanced solutions.
- No significant differences in:
- ICU or hospital length of stay
- Mechanical ventilation duration
- Need for vasopressors
- Renal replacement therapy (RRT)
- ICU or hospital length of stay
TBI patients:
- An estimated 4–83 more deaths per 1000 when treated with balanced solutions.
- Increased intracranial pressure and cerebral edema are likely contributors.
Renal outcomes, ICU stay, and ventilation needs showed no significant benefit with either fluid type.
Step-by-step: How to choose the right IV fluid
- Identify the primary diagnosis: Is the patient suffering from TBI, sepsis, or general critical illness?
- Evaluate comorbid conditions: Especially renal disease, electrolyte imbalances, and acid-base disturbances.
- Review current guidelines and evidence, such as sepsis protocols or neurocritical care guidelines.
- Select the fluid:
- TBI: Prefer normal saline
- Non-TBI critically ill: Choose balanced crystalloids
- Sepsis: Either fluid is acceptable, but consider balanced solutions for acid-base stability
- TBI: Prefer normal saline
Monitor closely: Adjust based on response, laboratory values, and clinical status.
Final thoughts
This comprehensive review challenges the “one-size-fits-all” approach to IV fluid resuscitation. Instead, it emphasizes the importance of context, diagnosis, and patient-specific physiology. While balanced crystalloids may be safer and more effective for most critically ill patients, they can be detrimental in TBI, where isotonic fluids like normal saline are preferable.
Reference: Diz JC et al. Anesth Analg. 2025;141:152-161.
For more information on IV fluids and their impact on perioperative care, check out Anesthesia Updates on the NYSORA Anesthesia Manual App.
Get access to step-by-step management algorithms, the latest research, and peer-reviewed insights—all in one place. Download the app today and experience the future of anesthesia education and decision-making.
Here’s what Anesthesia Assistant recommends:
A 58-year-old man with multiple rib fractures and moderate traumatic brain injury (GCS 9) is admitted to the ICU.
He requires resuscitation and ongoing fluid support.
What IV fluid should you reach for?