Learning objectives
- Diagnose and management of salicylate toxicity
Diagnosis and mechanisms
- Salicylate toxicity is the result of ingestion of, or (rarely) topical exposure to, chemicals metabolized to salicylate
- Poisoning may occur due to acute or chronic salicylate exposure
- Uncouple oxidative phosphorylation
- Interfere with the Krebs cycle
- Lead to accumulation of lactic acid & ketoacids
- Characterized by acid-base disturbances, electrolyte abnormalities, and central nervous system effects
- Unintentional salicylate toxicity is more common than intentional intoxication
- The most common source of salicylate poisoning is aspirin itself (acetylsalicylic acid) which is rapidly hydrolyzed to salicylate in the gastrointestinal tract, liver, and bloodstream
- Acute toxicity may occur after ingestion of a single dose of aspirin or the equivalent of >150 mg/kg or >6.5 g
- Chronic poisoning tends to occur as a result of repeated exposure to high-dose aspirin or equivalent (150 mg/kg/day), particularly in the setting of renal insufficiency
- Beware that many over-the-counter medications contain salicylates such as Pepto-Bismol, etheric oils, vapors, or analgesic ointments
- Herbs and spices such as ginger or mint also contain salicylates which can add to the drug burden
- Initially, symptoms such as tachypnea, lung crackles, and fever, often mimic a viral infection
- The classic triad of mild toxicity:
- Nausea
- Vomiting
- Tinnitus
Pathophysiology
Therapeutic levels of salicylates
- Irreversibly block COX-1 and modify COX-2 leading to a decrease in inflammation and platelet aggregation
Toxic levels of salicylates
- Stimulate the respiratory center causing hyperpnea
- Shift in metabolism to glycolysis for energy production → ↑ oxygen consumption and heat production → lactic acidosis
Signs and symptoms
| Nervous system | Tinnitus Listlessness Vertigo and incoordination Hallucinations Muscle rigidity Seizures Cerebral edema Coma |
| Gastro-intestinal | Nausea Vomiting |
| Respiratory | Hyperpnea Noncardiogenic pulmonary edema |
| Cardiac | Cardiovascular collapse |
| Metabolic | Fever Respiratory alkalosis Increased anion-gap metabolic acidosis (late sign) Hypernatremia due to fluid deficit Hypokalemia |
Diagnosis
- Arterial blood gases
- Serum electrolyte panel
- Serum salicylate level
- BUN and creatinine
- ECG
- Head CT scan
- EEG
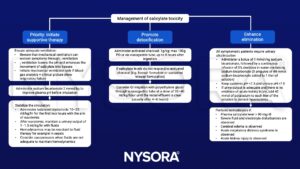
Management
Suggested reading
- Palmer BF, Clegg DJ. Salicylate Toxicity. N Engl J Med. 2020;382(26):2544-2555.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com