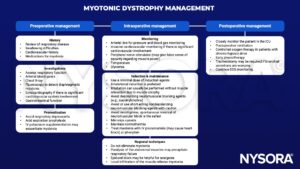
Learning objectives
- Describe the causes and symptoms of myotonic dystrophy
- Diagnose and treat myotonic dystrophy
- Manage myotonic dystrophy patients presenting for surgery
Background
- Myotonic dystrophy (DM) is an autosomal dominant disorder characterized by muscle dystrophy starting in early adulthood
- Myotonic dystrophy type I (DM1, Steinert disease) and type II (DM2, proximal myotonic myopathy, milder form of type I)
- Multisystem disorder affecting somatic and smooth muscle, as well as ophthalmological, cardiovascular, endocrine, and central nervous systems
Etiology
- Genetic disorder caused by an expansion of DNA tandem repeats, resulting in an RNA gain of function mutation
- DM1 is caused by an expansion of a CTG repeat in the 3’-untranslated region of the DM1 protein kinase gene
- DM2 is caused by the expansion of a CCTG repeat in the intron of the CCHC-type zinc finger nucleic aced-binding protein gene
- DM is the most common muscular dystrophy in the European population
- DM1 is more common than DM2
Signs & symptoms
- Can range from potentially lethal in infancy to mild in late adulthood
- DM1 is classified into three types:
- Congenital myotonic dystrophy
- Fetal-onset involvement of muscle and central nervous system
- Reductions in fetal movement and polyhydramnios
- Equinovarus and ventriculomegaly on fetal ultrasound
- Neonatal mortality rate ~18%
- Childhood/adulthood: Characteristic tented appearance of the upper lip that results from facial diplegia, marked dysarthria, expressive aphasia, hypotonia rather dan myotonia
- Frequent respiratory involvement
- Mild myotonic dystrophy
- Mild muscle weakness, myotonia, and cataracts
- Onset between 20-70 years of age (typically after 40)
- Usually normal lifespan
- Classic myotonic dystrophy
- Onset during the second, third, or fourth decade of life
- Myotonia is the primary initial symptom
- Characterized by “warm-up phenomenon”: Symptoms appear more pronounced after rest and improve with muscle activity
- Distal muscle weakness is the main symptom, leading to impairment of fine motor tasks with the hands and impaired gait
- “Myopathic face”: due to weakness and wasting of facial, levator, palpebrae, and masticatory muscles
- Cardiac conduction abnormalities are common
- Reduced lifespan
- Congenital myotonic dystrophy
- DM2:
- Manifests in adulthood (median age 48 years) with a variable presentation
- Early-onset cataract, varying grip myotonia, proximal muscle weakness or stiffness, hearing loss, myofascial pain
- Weakness and/or myalgias are the most common initial symptoms
- Mostly axial and proximal muscle weakness affecting the neck flexors, long finger flexors, hip flexors, and hip extensors
- Abdominal, musculoskeletal, and exercise-related pain
- Sometimes misdiagnosed as fibromyalgia
Diagnosis
- Genetic testing
- Elevations in alkaline phosphatase, gamma-glutamyl transferase, serum aspartate aminotransferase, and serum alanine aminotransferase in 30-50% of patients
- Electrodiagnostic testing:
- Motor nerve conduction studies: Decreased amplitude with normal latency and normal conduction velocity
- Sensory nerve conduction studies: Typically normal
- Electromyography:
- Sustained runs of positive sharp waves
- Trains of negative spikes
- Fluctuating amplitude and frequencies
- Muscle biopsy: Type I fiber atrophy, Type 2 fiber hypertrophy, irregular fiber size, rows of internal nuclei, fibrosis, myofibrils oriented perpendicular to muscle fiber
Differential diagnosis
- Schwartz–Jampel Syndrome
- Duchenne muscular dystrophy
- Hyperkalemic Periodic Paralysis (HPP)
- Paramyotonia Congenita (PC)
- Myotonia Congenita
- Myotubular myopathy
- Acid maltase deficiency
- Debrancher deficiency
- Inflammatory myopathies
- Hypothyroid myopathy
- Chloroquine myopathy
- Statin myopathy
- Cyclosporine myopathy
Treatment
- No curative treatment, therapy is supportive and consists of monitoring and treating the issues associated with DM
| Cardiovascular | Annual ECG monitoring for cardiac conduction disturbances Baseline cardiac imaging every 1 to 5 years |
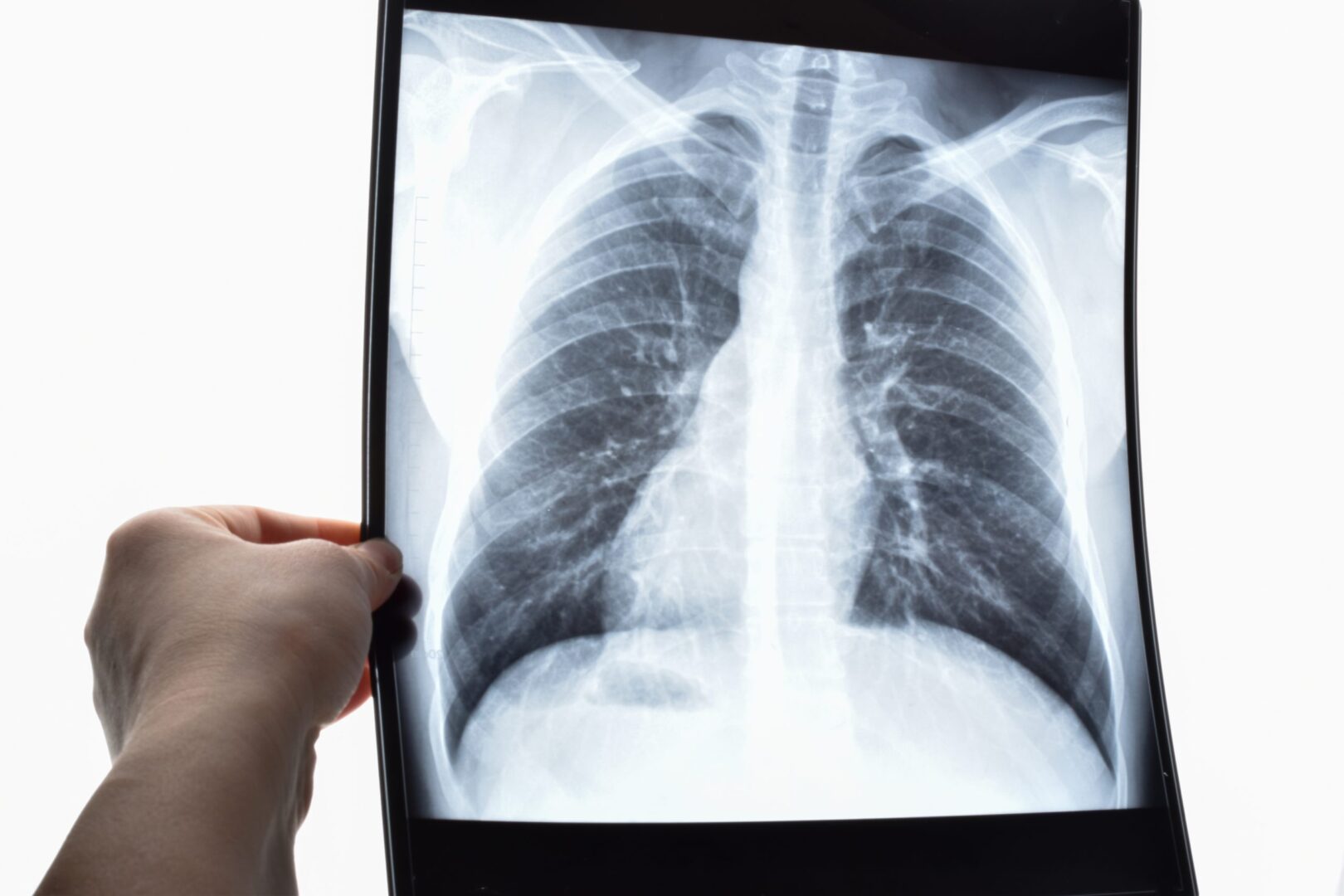
| Pulmonary | Obtaining baseline and serial pulmonary function testing to monitor for neuromuscular respiratory failure |
| Daytime somnolence and obstructive sleep apnea | Evaluate for sleep apnea and treat if necessary Consider neurostimulants (e.g., methylphenidate) for excessive sleepiness |
| Ocular involvement | Annual eye exam Surgical removal of cataracts |
| Obstetrics and gynecology | High-risk obstetrics evaluation for patients who are pregnant or considering pregnancy |
| Endocrine issues | Baseline and annual fasting blood glucose and hemoglobin A1C Screening for hypothyroidism Treat erectile dysfunction if necessary |
| Myotonia | Medications such as mexiletine, tricyclic antidepressants, benzodiazepines, or calcium antagonists reduce sustained myotonia Sodium channel blockers are contraindicated in patients with second and third-degree heart block |
| Muscle weakness | Physical and occupational therapy to strengthen muscles |
Complications
Central nervous system Intellectual disabilities
Cerebrovascular accidents
Anxiety and depression
Hypersomnia and sleep apnea
Ventriculomegaly
Ophtalmologic Cataracts
Hyperopia
Astigmatism
Cardiac Atrial arrhythmias
Conduction system slowing
Ventricular arrhythmias
Cardiomyopathy
Early-onset heart failure
Pulmonary Pneumonia
Increased risk of anesthesia-related pulmonary complications
Gastrointestinal Dysphagia
Gallstones and cholecystitis
Tranaminitis and liver enzyme elevations
Increased risk of post-anesthesia aspiration
Endocrine Insulin insensitivity
Testicular atrophy and male infertility
Increased risk of abortion, miscarriage, pre-term birth, dysmenorrhea
Dermatologic Androgenic alopecia
Increased risk of basal cell carcinoma and pilomatrixomas
Musculoskeletal Progressive loss of motor function
Myalgias
Anesthetic management
Suggested reading
- Vydra DG, Rayi A. Myotonic Dystrophy. [Updated 2022 Jun 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557446/
- Pollard BJ, Kitchen, G. Handbook of Clinical Anaesthesia. Fourth Edition. CRC Press. 2018. 978-1-4987-6289-2.
- Marsh S, Pittard A. Neuromuscular disorders and anaesthesia. Part 2: specific neuromuscular disorders. Continuing Education in Anaesthesia Critical Care & Pain. 2011;11(4):119-23.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com