Learning objectives
- Complications and anesthetic management of carotid endarterectomy
Definition and mechanisms
- A surgical procedure to remove a build-up of fatty deposits (plaque), which cause narrowing of a carotid artery
- The carotid arteries are the main blood vessels that supply blood to the neck, face, and brain
- The carotid artery may become blocked or a clot is formed leading to a stroke or a transient ischemic attack (TIA)
- Carotid endarterectomy significantly reduces the risk of a stroke or TIA
Complications
- Stroke or TIA
- Myocardial infarction
- Cranial nerve injury
- Pooling of blood into the tissue around the incision site causes swelling
- Intracerebral hemorrhage
- Seizures
- Repeated blockage or new blockade of the carotid artery
- Bleeding at the incision site in the neck
- Infection
- High blood pressure
- Irregular heartbeat
- Blocked airway from swelling or from bleeding in the neck
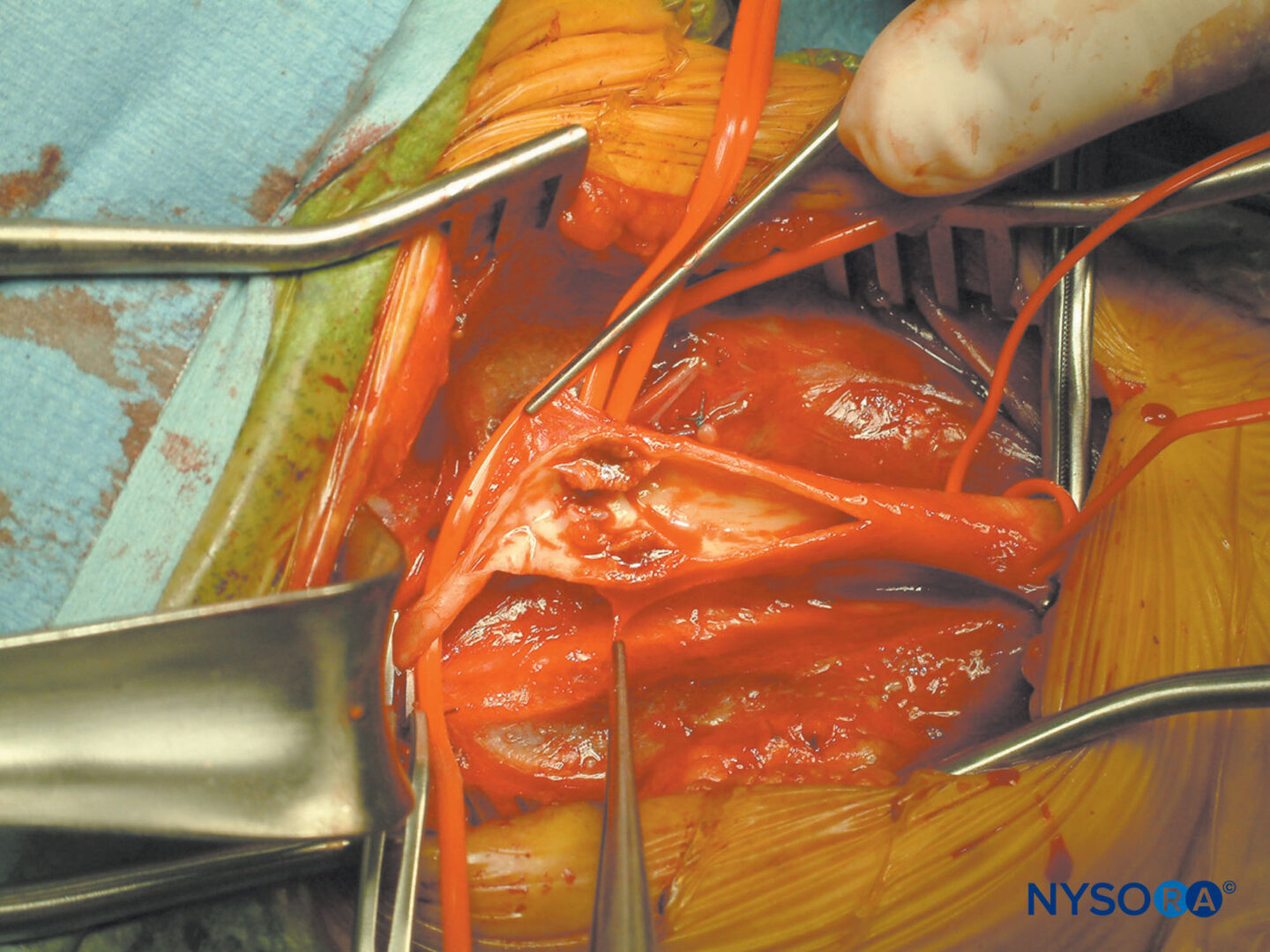
CEA operation
- After careful surgical exposure, the external, internal, and common carotid arteries are cross-clamped
- The carotid bifurcation is isolated from the circulation
- The artery is opened and the plaque will be removed
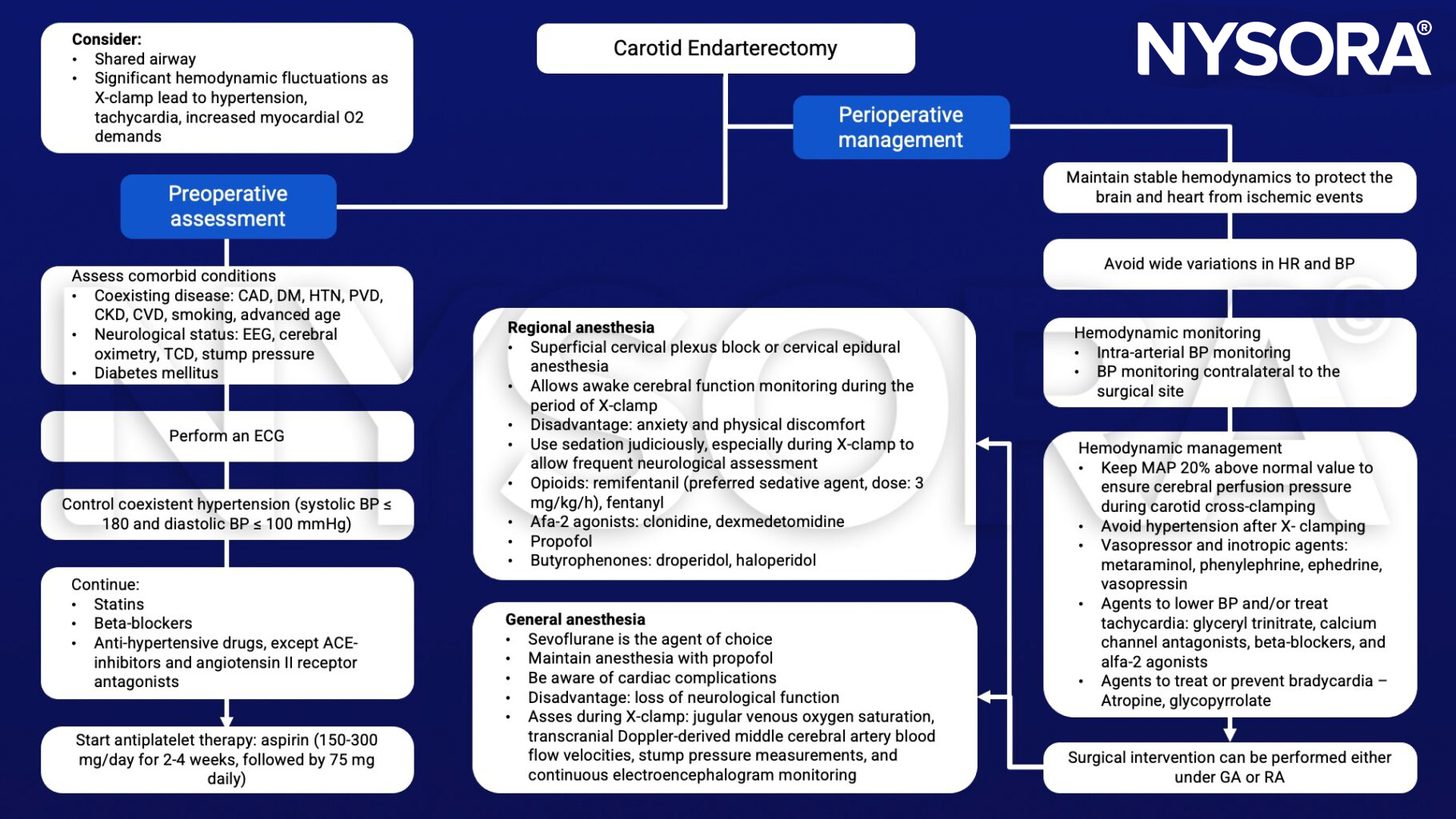
Management
Suggested reading
- Zdrehuş C. Anaesthesia for carotid endarterectomy – general or loco-regional?. Rom J Anaesth Intensive Care. 2015;22(1):17-24.
- Howell SJ. Carotid endarterectomy, BJA: British Journal of Anaesthesia, Volume 99, Issue 1, July 2007, Pages 119–131.
Clinical updates
Ryalino C et al. (British Journal of Anaesthesia, 2024) emphasize the growing role of multimodal intraoperative neuromonitoring during carotid endarterectomy to detect cerebral ischemia during carotid cross-clamping. The review highlights raw EEG for early ischemic changes, NIRS thresholds (absolute ScO₂ < 55% or ≥ 20% decrease from baseline), and transcranial Doppler detection of > 90% MCA flow reduction as indicators of inadequate cerebral perfusion and potential need for shunting.
- Read more about this study HERE.
Ratnayake A et al. (BMC Anesthesiology, 2024) report that combined superficial and intermediate cervical plexus block (SCPB + ICPB) provided adequate anesthesia for carotid endarterectomy (CEA) in 4 of 5 patients, with only one requiring supplemental local infiltration and no major complications. Compared with deep cervical plexus block (DCPB), the intermediate approach required fewer injections and avoided serious risks such as intravascular injection, epidural spread, and phrenic nerve palsy, while allowing continuous real-time neurologic monitoring during carotid cross-clamping.
- Read more about this case study HERE.
Vetter C et al. (European Journal of Anaesthesiology, 2025) report in a prospective randomized trial that co-administration of dexmedetomidine during total intravenous anesthesia (TIVA) for carotid endarterectomy reduced the propofol effect-site concentration required for burst suppression by 33% and decreased norepinephrine requirements by 50% compared with standard TIVA. Importantly, dexmedetomidine did not impair intraoperative somatosensory or motor-evoked potential monitoring and was not associated with increased postoperative delirium.
- Read more about this study HERE.