As healthcare systems globally evolve toward delivering high-value, patient-centered care, each component of perioperative management is being rigorously scrutinized for both clinical efficacy and economic sustainability. One area of active investigation is the optimal route of administration for acetaminophen, a core element of multimodal analgesia strategies employed in modern surgical recovery protocols.
A new prospective, randomized controlled trial (RCT), recently published in Regional Anesthesia & Pain Medicine, addresses this critical issue by comparing intravenous (IV) and oral formulations of acetaminophen in patients undergoing ambulatory spine surgery. This study delivers valuable insights into the utility, limitations, and cost-effectiveness of IV acetaminophen in the outpatient surgical context.
Methods
This parallel-group, single-blinded, randomized controlled trial enrolled 82 adult patients undergoing ambulatory lumbar spine surgery at either a tertiary care academic hospital or a specialized orthopedic hospital. All patients met the inclusion criteria based on American Society of Anesthesiologists (ASA) physical status (I–III), body weight ≥50 kg, and the ability to understand English. Exclusion criteria included pregnancy, revision surgery, known intolerance to acetaminophen, chronic pain unrelated to the surgical indication, and recent high-dose opioid use.
Patients were randomized to receive either:
- 1000 mg oral acetaminophen preoperatively (administered 30 minutes before operating room arrival), or
- 1000 mg intravenous acetaminophen intraoperatively (administered approximately 30 minutes before skin closure)
Importantly, both groups received a standardized multimodal regimen that included general anesthesia, intraoperative ketorolac and dexamethasone (unless contraindicated), and local bupivacaine infiltration when performed by the surgeon. Postoperative analgesia followed institutional protocols with as-needed fentanyl or hydromorphone in the PACU, transitioning to oral opioids once tolerated.
Primary and secondary endpoints
The primary endpoint was total postoperative opioid consumption within the first 24 hours, expressed in intravenous morphine milligram equivalents (MMEs). This timeframe included the PACU period and extended to the 24-hour postoperative phone follow-up.
Secondary endpoints included:
- Postoperative pain scores were assessed at 30 minutes, 60 minutes, and PACU discharge
- Quality of Recovery-15 (QoR-15) scores at baseline and 24 hours postoperatively
- Length of PACU stay
- Incidence of postoperative nausea and vomiting (PONV)
- Correlation analyses involving pain catastrophizing (PCS), opioid consumption, and QoR-15
Results
Opioid consumption
The core hypothesis—that IV acetaminophen would reduce opioid use—was not supported by the data. Median 24-hour MME consumption was statistically indistinguishable between groups:
- IV group: 12.6 mg (IQR: 4.0–27.1)
- Oral group: 12.0 mg (IQR: 4.0–29.5)
- p-value: 0.893
Sensitivity analysis using an “as-treated” model confirmed this lack of difference, even when accounting for crossovers.
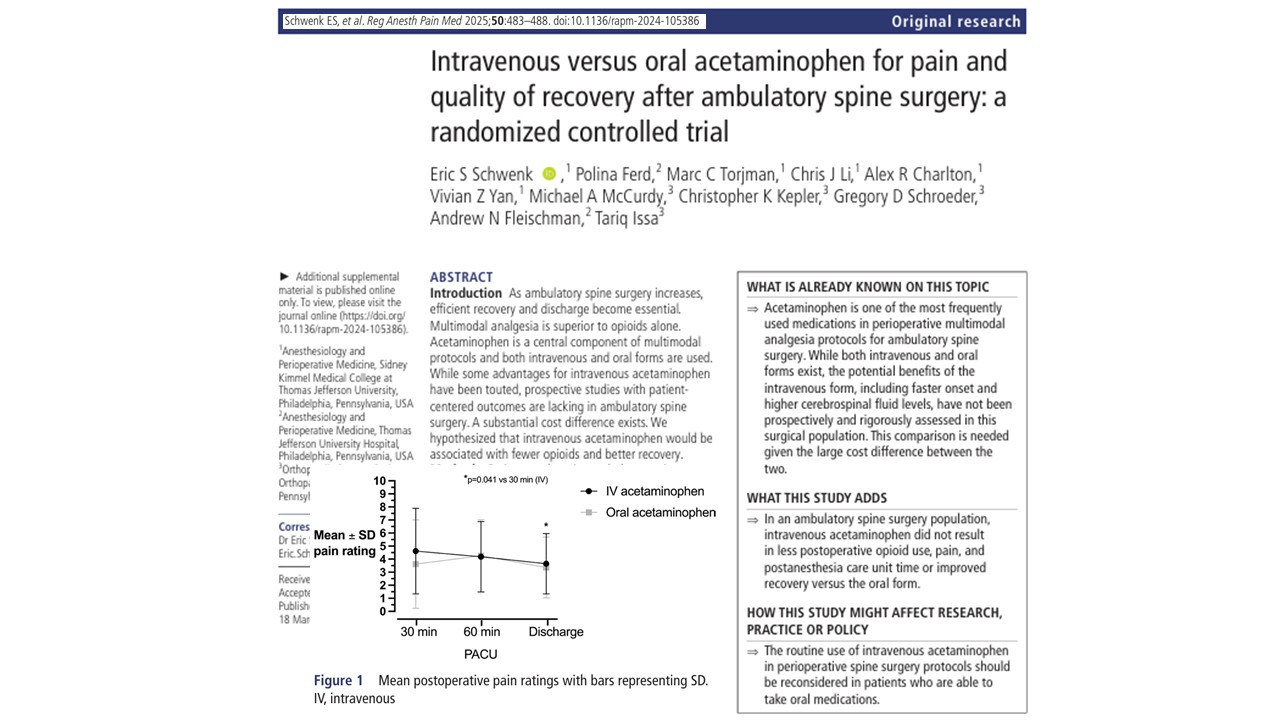
Postoperative pain
Pain intensity measured via Numerical Rating Scale (NRS, 0–10) showed no significant intergroup variation:
- At 30 minutes: IV 5 ± 3 vs. Oral 4 ± 3
- At 60 minutes: Both groups averaged 4 ± 3
- At PACU discharge: IV 4 ± 2 vs. Oral 3 ± 2
Despite the theoretically faster onset of IV administration, this did not translate into enhanced analgesic effect in practice.
Recovery quality
QoR-15 scores—a validated patient-reported measure assessing comfort, physical and emotional status, and recovery satisfaction—showed comparable outcomes:
- Preoperative: IV 112 vs. Oral 105
- Postoperative: IV 107 vs. Oral 113
- Change in score: Not statistically significant (p = 0.272)
Notably, oral acetaminophen was associated with a slight improvement in QoR-15 from baseline, whereas the IV group experienced a minor decline in quality of recovery. However, these differences were not deemed clinically significant.
PACU length of stay and PONV
No statistically significant differences were observed in either:
- PACU length of stay: IV 127 minutes vs. Oral 143 minutes
- PONV incidence: IV 19.0% vs. Oral 12.5% (p = 0.549)
Adverse events
There were no adverse drug reactions attributed to either formulation, reinforcing the overall safety profile of acetaminophen, irrespective of route.
Cost analysis
One of the most striking observations from the study is the discrepancy in drug acquisition cost:
- IV acetaminophen: $10.85–$28.42 per dose
- Oral acetaminophen: $0.03–$0.07 per dose
Given the absence of clinical superiority, the cost per quality-adjusted outcome for IV acetaminophen is orders of magnitude higher. When multiplied across the volume of surgeries performed annually, this represents a substantial, and arguably unnecessary, expenditure for health systems.
Psychological predictors and recovery outcomes
The study also incorporated validated psychological tools, such as the Pain Catastrophizing Scale (PCS), to assess their influence on pain perception and recovery. Although PCS scores correlated weakly with pain ratings across the entire cohort, a moderate correlation emerged within the IV group only (R=0.571, p<0.001), suggesting a possible psychosocial interaction with perceived analgesic effect.
More notably, there was a moderate negative correlation between postoperative opioid use and QoR-15 scores (R=−0.505, p<0.001), highlighting the relationship between opioid exposure and poorer patient-reported recovery.
These exploratory findings suggest that optimizing analgesia must consider both pharmacologic efficacy and the psychological dimensions of recovery.
Clinical implications
This trial offers strong evidence to support a reevaluation of perioperative analgesia pathways that routinely favor IV acetaminophen over oral forms. For most patients undergoing outpatient spine surgery:
- Oral acetaminophen is clinically equivalent
- IV acetaminophen adds no measurable benefit
- The cost differential is unjustified in the absence of special circumstances
Such findings are directly translatable to practice and can guide hospital formularies, pharmacy and therapeutics (P&T) committees, and perioperative care teams in crafting evidence-based, cost-effective protocols.
When might IV acetaminophen still be useful?
Despite the lack of routine benefit, there are scenarios where IV acetaminophen may retain utility:
- Patients with contraindications to oral intake (e.g., bowel obstruction, vomiting, ileus)
- Immediately postoperatively, when oral access is delayed
- In patients requiring rapid analgesia with no delay in GI absorption
However, such cases should be clearly defined and not serve as justification for routine use.
Study limitations and future directions
While methodologically sound, the study acknowledges several limitations:
- Absence of intravenous placebo: This could have influenced intraoperative opioid administration, although no differences were observed in intraoperative MMEs.
- Site variability: Though patients were recruited from two distinct surgical settings, patient characteristics and treatment protocols were balanced.
- Ketorolac use: While potentially confounding, its inclusion reflects standard care and was equally distributed.
- Data loss: Eight data sets were excluded due to loss before entry, but sensitivity analyses confirmed no impact on final conclusions.
Future studies could explore subpopulations (e.g., patients with high PCS scores) or investigate outcomes over a longer postoperative timeline.
Conclusion
In the context of ambulatory lumbar spine surgery, the use of intravenous acetaminophen does not offer clinical advantages over oral acetaminophen in terms of pain control, opioid sparing, or patient-perceived recovery. With its significantly higher cost, the routine use of the IV formulation is not supported by evidence. This study reinforces the principle that evidence—not assumption or tradition—should guide perioperative pharmacological decisions.
For more information, refer to the full article in Regional Anesthesia & Pain Medicine.
Schwenk ES, Ferd P, Torjman MC, Li CJ, Charlton AR, Yan VZ, McCurdy MA, Kepler CK, Schroeder GD, Fleischman AN, Issa T. Intravenous versus oral acetaminophen for pain and quality of recovery after ambulatory spine surgery: a randomized controlled trial. Reg Anesth Pain Med. 2025 Jun 10;50(6):483-488.
Read more about acetaminophen and spine surgery in our Anesthesiology Manual: Best Practices & Case Management.