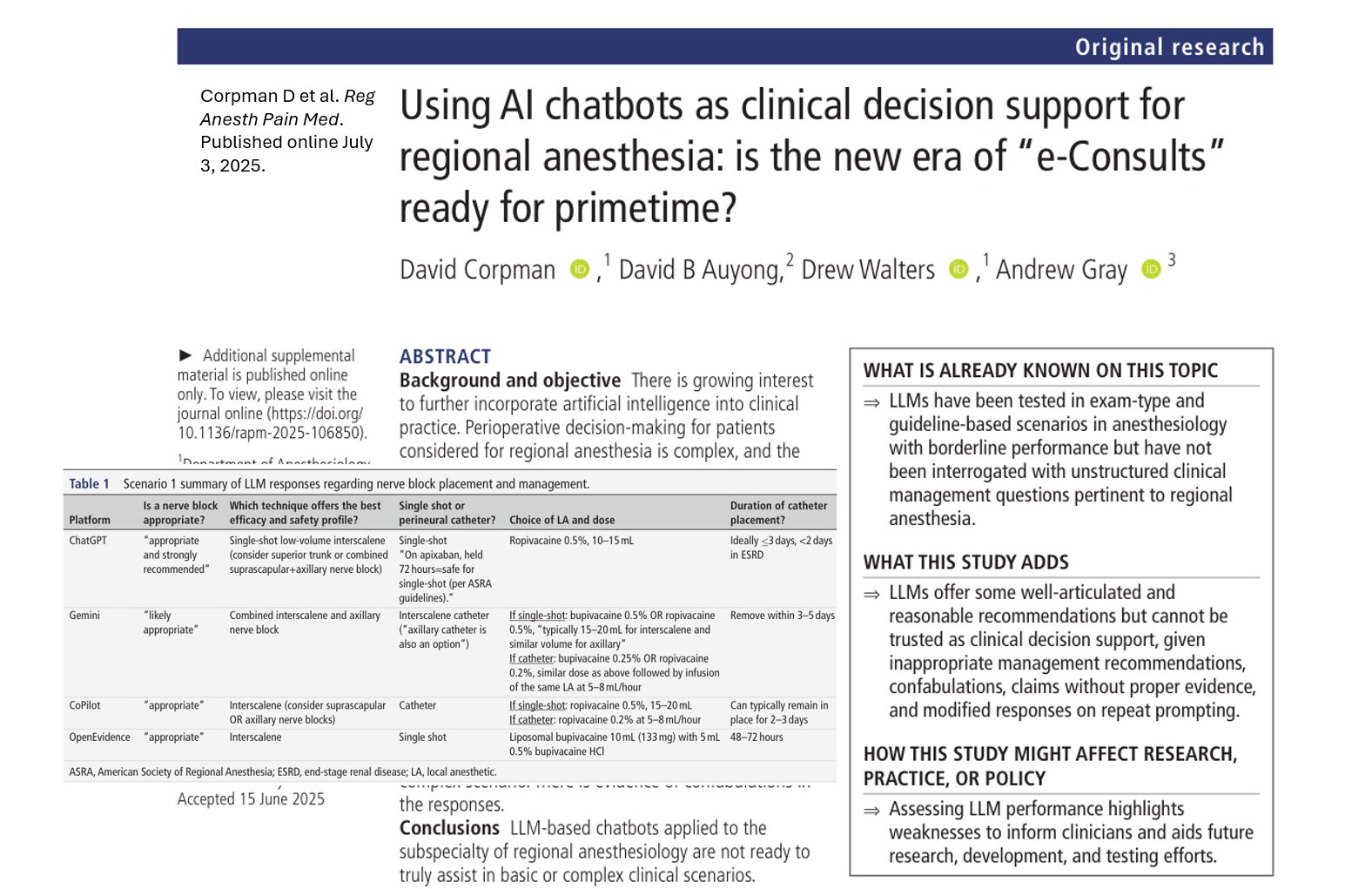
A new study published in Regional Anesthesia & Pain Medicine by Corpman et al. (2025) critically evaluates the potential of AI chatbots, powered by large language models (LLMs), as clinical decision support tools in regional anesthesiology. With AI becoming increasingly embedded in healthcare, this research offers a timely examination of its readiness for real-world perioperative decision-making.
Background: AI’s expanding role in anesthesia
AI technologies have already demonstrated utility in ultrasound-based image recognition and block placement in regional anesthesia. However, these tasks represent only a fraction of the broader clinical decision-making required. The study examines whether generative AI can aid anesthesiologists in making complex judgment calls, such as block selection, dosing, and risk-benefit communication.
Study design
- LLMs evaluated: ChatGPT-4o, Gemini 2.0 Flash, Microsoft CoPilot, and OpenEvidence
- Approach: Zero-shot prompting of two scenarios (basic and complex) to simulate real-world clinical decision-making
- Evaluation: Qualitative analysis by experienced regional anesthesiologists using practice guidelines and peer-reviewed literature
Scenario-based testing
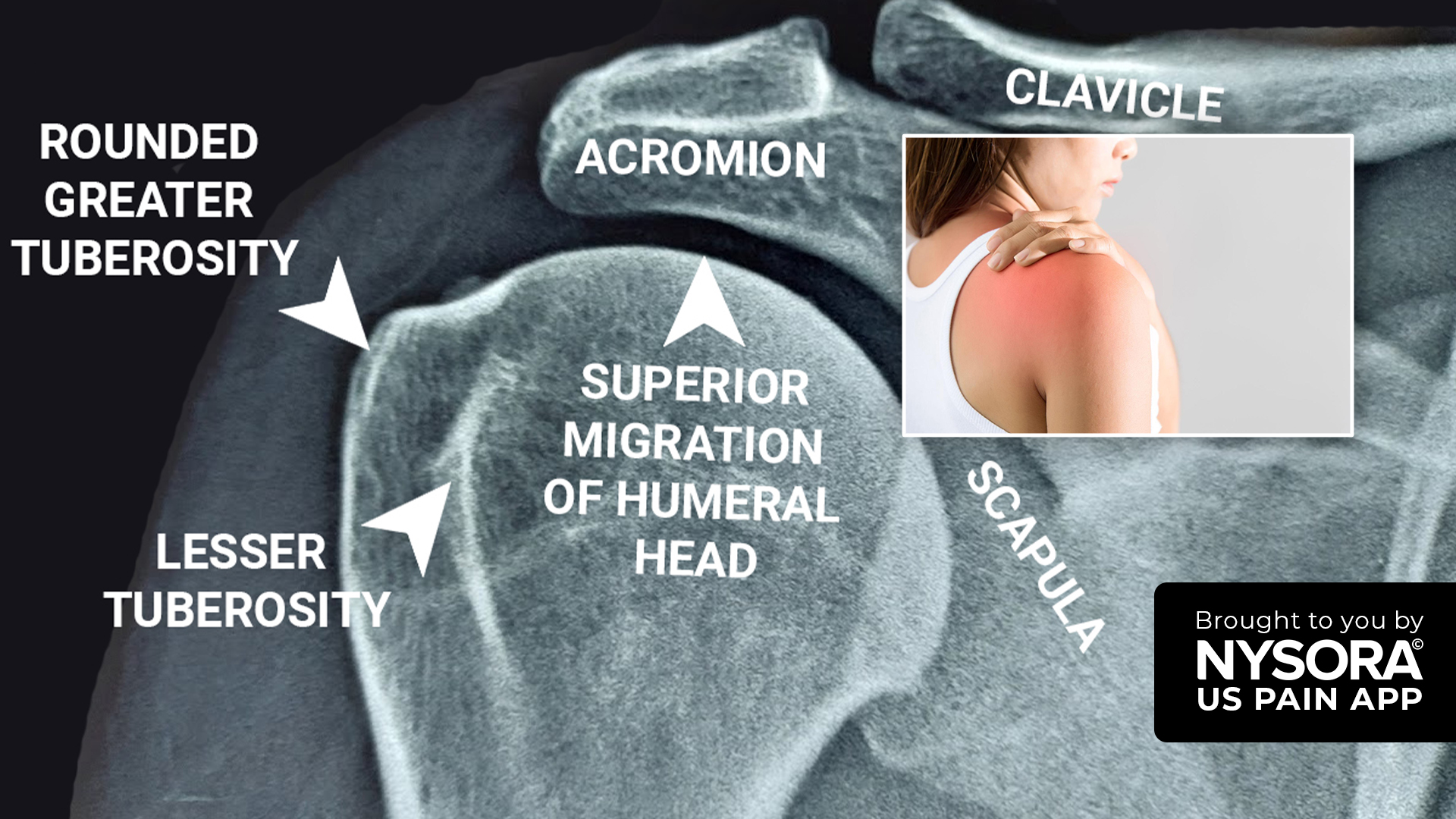
Scenario 1: High-risk patient undergoing total shoulder replacement
- Patient profile: Multiple comorbidities including atrial fibrillation on apixaban, ESRD on hemodialysis, and COPD
- Decision: Is a nerve block safe, and if so, what type, dosing, and duration?
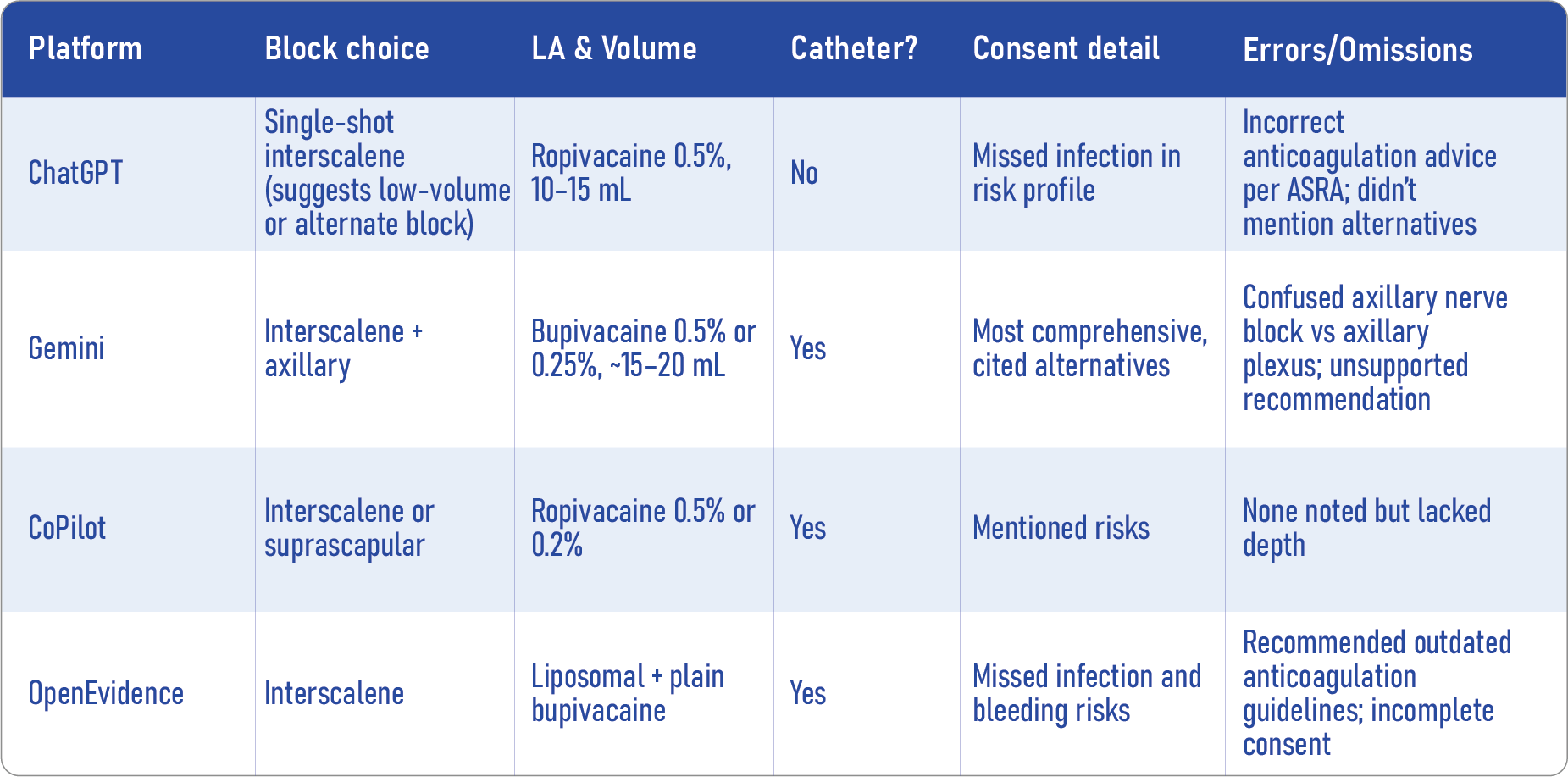
Key findings:
- All LLMs recommended the interscalene block despite known risks like hemidiaphragmatic paralysis.
- No model questioned the appropriateness of the block or asked for clarifying details.
- Misinterpretations of anticoagulation guidelines were common.
- Suggested informed consent content varied and often omitted key risks and alternatives.
Scenario 2: Healthy patient undergoing same-day discharge total knee arthroplasty
- Focus: Optimal peripheral nerve block selection to balance analgesia with early mobilization
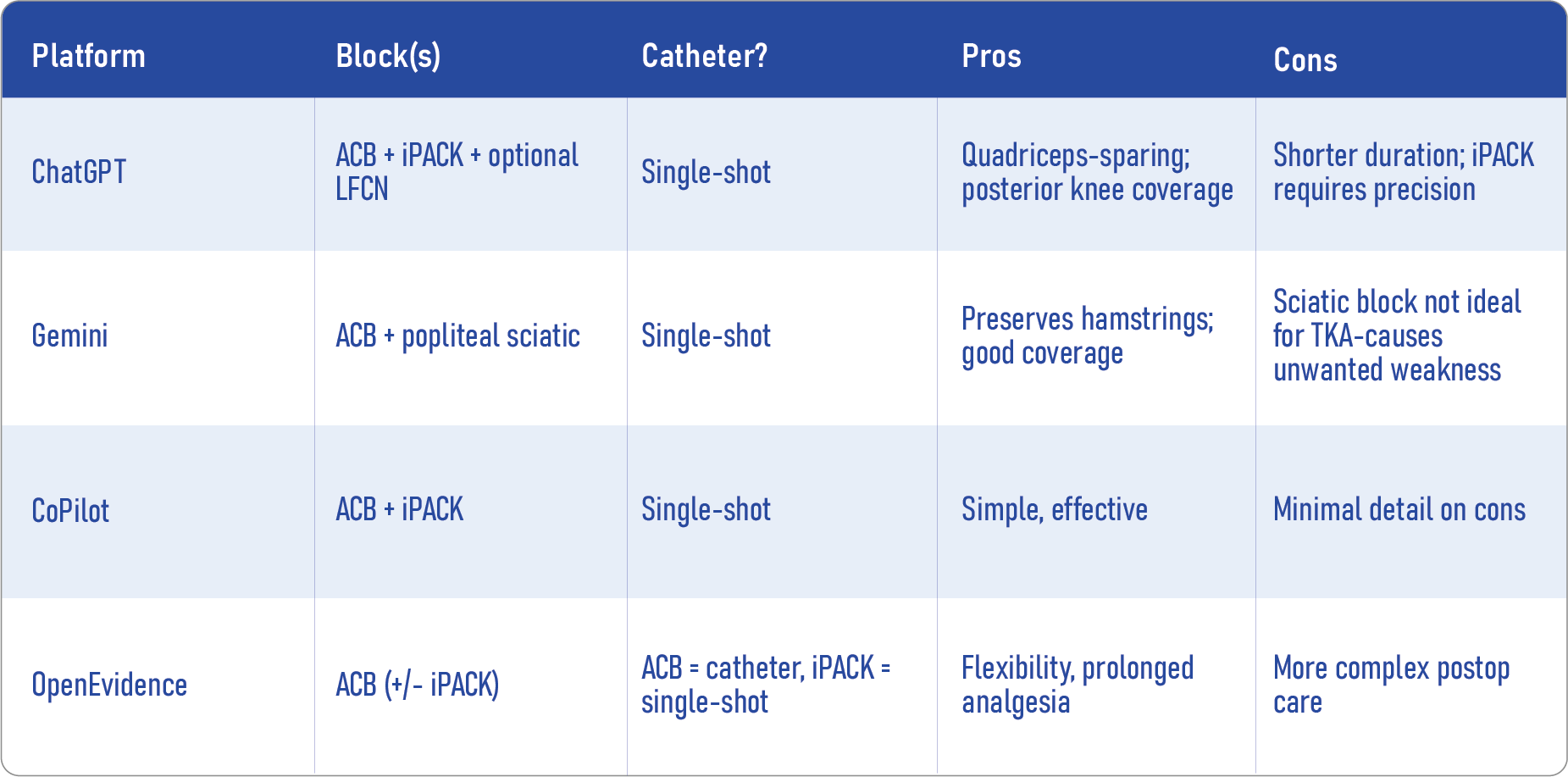
LLM recommendations:
- Common picks: ACB+iPACK or ACB+popliteal sciatic
- Generally sound advice, but with notable exceptions:
- Gemini’s sciatic block could impair ambulation
- Only a few models cited literature, and when they did, it lacked anesthesiology-specific depth
- Gemini’s sciatic block could impair ambulation
Best practices moving forward
How to use LLMs safely in clinical settings
- Always validate LLM recommendations with current guidelines and clinical judgment.
- Use AI as a brainstorming tool, not a source of definitive advice.
- Apply prompt engineering to refine queries and test understanding.
- Incorporate AI outputs into team discussions, never as a standalone directive.
- Report AI errors to developers or researchers to contribute to safety improvements.
Future directions and final thoughts
The future of AI in anesthesiology holds promise. Agentic AI, which is goal-driven and context-aware, may reduce reliance on manual precision. Integration with EMR data, personalized learning, and real-time risk assessments could revolutionize patient care.
Reference: Corpman D et al. Reg Anesth Pain Med. Published online July 3, 2025.
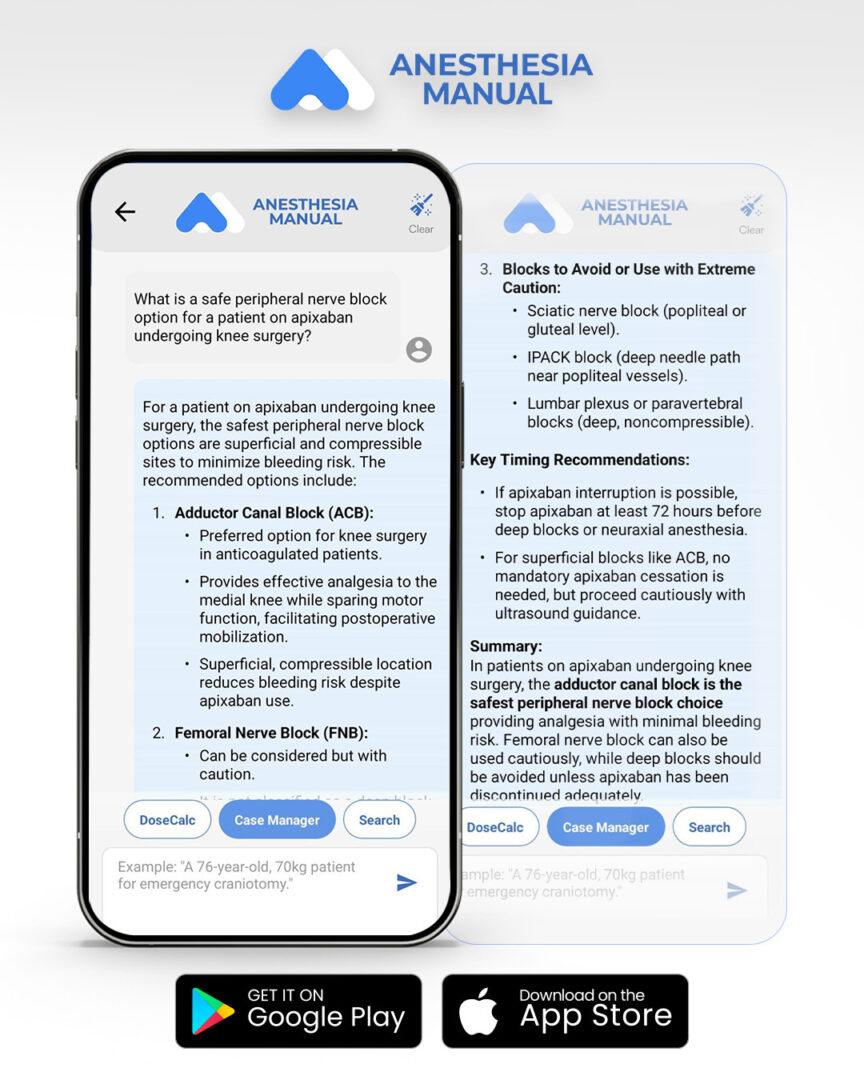
For more information on AI in a medical context, check out Anesthesia Updates on the NYSORA Anesthesia Manual App.
Get access to step-by-step management algorithms, the latest research, and peer-reviewed insights—all in one place. Download the app today and experience the future of anesthesia education and decision-making.
Let’s test MAIA
What is a safe peripheral nerve block option for a patient on apixaban undergoing knee surgery?