A landmark study published in the September 2025 issue of Anesthesia & Analgesia by Guglielminotti et al. sheds new light on the mental health risks associated with the use of general anesthesia (GA) for cesarean delivery. Researchers at Columbia University report that women who underwent cesarean delivery under GA faced a significantly increased risk of postpartum depression (PPD) requiring hospitalization and a heightened risk of suicidality compared to those who received neuraxial anesthesia, even after accounting for obstetric complications.
These findings highlight an often-overlooked dimension of maternal health: how the choice of anesthesia at delivery may influence psychological well-being for months after childbirth. The study emphasizes the need to limit GA use when alternatives are available and to implement routine postpartum mental health screening for women exposed to GA.
Cesarean delivery in the U.S.: common and complex
Cesarean delivery is among the most frequently performed surgical procedures in the United States, with roughly 1.2 million operations each year. Over the past few decades, improvements in surgical techniques and anesthesia care have greatly reduced physical risks. However, the procedure remains associated with a wide range of complications—from infection and hemorrhage to thromboembolic events.
The anesthetic approach plays a critical role in both safety and recovery. Neuraxial techniques, such as spinal or epidural anesthesia, are widely considered the gold standard for cesarean delivery. These techniques allow the mother to remain awake and present during the birth, reduce maternal complications, and generally offer better pain control.
By contrast, general anesthesia, which renders the mother unconscious and requires airway management, is used in a minority of cesarean deliveries. The national GA rate for cesarean delivery has steadily declined and now hovers around 5–6%, typically reserved for emergencies (e.g., severe hemorrhage, fetal distress) or when neuraxial anesthesia is contraindicated.
The 2016 American Society of Anesthesiologists (ASA) guidelines strongly recommend neuraxial anesthesia for most cesarean deliveries, citing increased risks of maternal morbidity and mortality with GA. What has been less studied until recently, however, is the mental health impact of GA compared to neuraxial techniques.
Postpartum depression: a hidden epidemic
Postpartum depression (PPD) is one of the most prevalent complications of childbirth, affecting about 13% of new mothers. Characterized by persistent sadness, anxiety, guilt, and difficulty bonding with the newborn, PPD has serious implications for both mother and child.
- PPD is a leading risk factor for maternal self-harm and suicide, which are increasingly recognized as major contributors to preventable maternal deaths in the United States.
- PPD can also negatively impact infant development, particularly if maternal mental health challenges interfere with breastfeeding, bonding, or early caregiving.
- Importantly, the burden of PPD is not equally distributed. Minority women, especially Black and Hispanic mothers, report higher rates of depressive symptoms but are less likely to receive timely diagnosis or treatment due to systemic barriers in healthcare.
Against this backdrop, examining modifiable medical factors that influence PPD risk—such as the mode of anesthesia during delivery—is vital for improving maternal outcomes.
Study design: linking anesthesia to maternal mental health
Using data from the New York State Inpatient Database (SID), State Ambulatory Surgery and Services Database (SASD), and State Emergency Department Database (SEDD), the team conducted a retrospective cohort study spanning nearly a decade (2009–2017).
The researchers included 325,840 women aged 10–44 years who underwent cesarean delivery. They excluded patients lacking key demographic or anesthesia information to ensure accuracy. Each patient was followed for one year after delivery, and outcomes were tracked across hospital readmissions, outpatient visits, and emergency department (ED) encounters.
Outcomes measured
- Primary outcome: Diagnosis of postpartum depression (PPD) within one year of delivery, recorded in hospital or ED databases.
- Secondary outcomes:
- PPD requiring hospitalization (a marker of severity).
- Suicidality, including suicidal ideation, attempts, self-harm, and suicide.
Accounting for confounders
One of the key strengths of this study was its careful attention to obstetric complications that could confound results. For example:
- Preterm birth increases both the likelihood of GA and the risk of PPD.
- Stillbirth, postpartum hemorrhage, and severe maternal morbidity are linked to higher GA rates and poorer maternal mental health outcomes.
To address this, the researchers used propensity score matching and overlap weighting to balance groups of women who received GA versus neuraxial anesthesia. This approach controlled for 44 patient- and hospital-level variables, including psychiatric history, substance use, partner violence, and delivery hospital characteristics.
Key findings
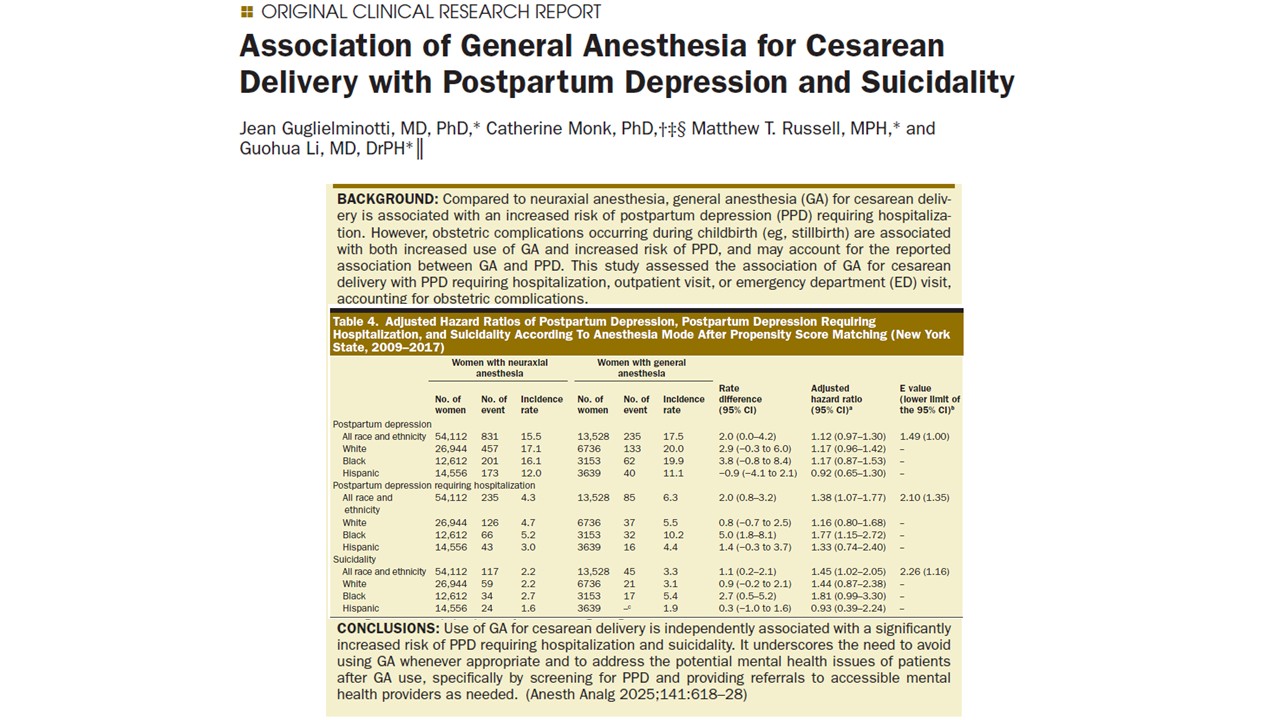
Among the women studied, 19,513 (6%) received GA for cesarean delivery. The results were striking:
- Overall PPD: 4,131 women (12.8 per 1,000 person-years) developed PPD within a year of delivery. After adjustment, GA was not significantly associated with overall PPD incidence.
- PPD requiring hospitalization: GA was associated with a 38% increased risk. This suggests that GA may not raise overall PPD rates but is linked to more severe cases.
- Suicidality: GA was associated with a 45% increased risk.
Racial and ethnic differences
- White women: Highest incidence of diagnosed PPD overall (14.5 per 1,000 person-years).
- Black women: Highest incidence of suicidality (2.3 per 1,000 person-years). GA significantly increased the risk of PPD hospitalization and suicidality in this group.
- Hispanic women: Lower recorded rates of PPD (9.4 per 1,000 person-years), but likely due to underdiagnosis and reduced access to care.
These findings highlight inequities in diagnosis and treatment, suggesting that Black women not only experience higher rates of severe outcomes but may also carry disproportionate burdens from GA-related risks.
Why general anesthesia may worsen maternal mental health
The researchers discuss several mechanisms that may explain why GA is linked to higher risks of severe PPD and suicidality:
- Delayed maternal-newborn contact: Mothers under GA miss immediate skin-to-skin interaction, which has been shown to protect against PPD and improve breastfeeding success.
- Breastfeeding challenges: GA can delay the first breastfeeding attempt, which has been independently linked to depressive symptoms.
- Postoperative pain: GA has been associated with worse postoperative pain compared to neuraxial anesthesia. Severe acute pain after childbirth triples the risk of developing PPD.
- Psychological impact of expectations: Many women anticipate being awake during birth. Unexpected GA may create feelings of disappointment, disconnection, or guilt.
- Associated emergencies: Situations requiring GA, such as hemorrhage or fetal distress, may themselves increase risk. While this study adjusted for these complications, residual effects cannot be ruled out.
Together, these factors suggest that the experience of GA extends beyond the operating room, potentially shaping maternal well-being long after delivery.
Clinical implications
The findings reinforce the need for anesthesiologists, obstetricians, and perinatal care teams to think beyond the immediate surgical episode.
Implications for practice
- Prefer neuraxial anesthesia: Whenever possible, neuraxial techniques should remain the default approach for cesarean delivery.
- Identify high-risk women: Women who undergo GA should be flagged for enhanced postpartum mental health surveillance.
- Integrate mental health care: Hospitals should create systems for early screening and referral to psychiatric services, particularly for women with known risk factors.
- Address disparities: Given the disproportionate impact on Black women, targeted interventions to improve equity in peripartum care are urgently needed.
Implications for research
Future studies should:
- Explore biological pathways linking anesthesia type to depression.
- Investigate the role of acute and chronic pain as mediators.
- Evaluate whether supportive interventions, such as structured postpartum counseling for GA-exposed women, can mitigate risks.
- Examine outcomes in other states and internationally to confirm generalizability.
Limitations
While the study is robust, certain limitations must be noted:
- Residual confounding: Some unmeasured factors, such as the urgency of cesarean delivery or anesthesiologist experience, could influence results.
- Administrative data: Reliance on ICD codes may underestimate PPD prevalence, particularly before 2015, when no specific PPD code existed.
- Geographic focus: Data were limited to New York State; outcomes may differ across regions.
- No neonatal data: Information on newborn health and bonding was unavailable, limiting insights into mother-infant dynamics.
Despite these challenges, the study provides one of the most comprehensive assessments to date of GA’s impact on maternal mental health.
Conclusion
The study offers compelling evidence that general anesthesia during cesarean delivery is not just a matter of physical risk, but also of long-term mental health. While GA remains an indispensable tool in emergencies, its association with increased risks of severe postpartum depression and suicidality cannot be ignored. These findings should guide clinical practice toward greater caution in GA use, while also prompting proactive efforts to screen, support, and treat women at risk of postpartum mental health disorders.
In an era where maternal mortality and morbidity remain urgent public health concerns—especially in the United States—integrating mental health into obstetric anesthesia decision-making represents a crucial step toward more holistic, equitable, and compassionate maternal care.
For more information, refer to the full article in Anesthesia and Analgesia.
Guglielminotti J, Monk C, Russell MT, Li G. Association of General Anesthesia for Cesarean Delivery with Postpartum Depression and Suicidality. Anesth Analg. 2025 Sep 1;141(3):618-628.
Read more about cesarean delivery in our Anesthesiology Module on NYSORA 360—a complete training resource designed for residents, with practical, up-to-date guidance on perioperative and critical care management.