Herve Bouaziz
INTRODUCTION
Selective obturator nerve block was first described by Gaston Labat in 1922. More interest in obturator nerve block emerged a few years later when Victor Pauchet, Sourdat, and Gaston Labat stated, “obturator nerve block combined with blocks of the sciatic and femoral nerves, anesthetized the entire lower limb.” However, a lack of clear anatomic landmarks, the block complexity, and inconsistent results were the reasons why this block had been used infrequently. Historically, Labat’s classic technique remained forgotten until 1967, when it was modified by Parks. In 1993, the interadductor approach was described by Wassef, which was further modified by Pinnock in 1996. In 1973, Alon Winnie introduced the concept of the “3-in-1 block,” an anterior approach to the lumbar plexus using a simple paravascular inguinal injection to anesthetize the femoral, lateral cutaneous and obturator nerves. Since its description however, many studies have refuted the ability of the 3-in-1 block to reliably block the obturator nerve with this technique. With the introduction of modern nerve stimulators, and particularly ultrasound guidance selective block of the obturator nerve has become more reliable.
Indications
Obturator nerve block is used to treat hip joint pain and is also used in the relief of adductor muscle spasm associated with hemiplegia or paraplegia. Muscle spasticity is a relatively common problem among patients suffering from central neurologic problems, such as cerebrovascular pathology, medullar injuries, multiple sclerosis, and cerebral palsy.
Spasticity of the adductor muscle induced via the obturator nerve plays a major role in associated pain problems and makes patient hygiene and mobilization very difficult. Tenotomies, cryotherapy, botulinum toxin infiltration, surgical neurolysis, and muscle interpositions have been suggested to remedy this problem. Common clinical practice is to combine a sciatic nerve block with the femoral nerve block for surgical procedures distal to the proximal third of the thigh. When deemed necessary, addition of a selective obturator nerve block may reduce intraoperative discomfort, improve tourniquet tolerance, and improve the quality of postoperative analgesia in these cases.
Obturator nerve block is also occasionally used in urologic surgery to suppress the obturator reflex during transurethral resection of the lateral bladder wall. Direct stimulation of the obturator nerve by the resector as it passes in close proximity to the bladder wall results in a sudden, violent adductor muscle spasm. This is not only distracting to the surgeon, but may increase the risk of complications such as bladder wall perforation, vessel laceration, incomplete tumor resection, and obturator hematomas. Prevention strategies include muscle relaxation, reduction in the intensity of the resector, the use of laser resectors, shifting to saline irrigation, periprostate infiltrations, and/or endoscopic transparietal blocks. A selective obturator nerve block remains an effective remedy to this problem.
NYSORA Tips
The obturator reflex is not abolished by spinal anesthesia. It can be suppressed only by a selective obturator nerve block.
Neurolytic blocks with alcohol or phenol, performed with the help of a nerve stimulator and/or fluoroscopy, result in a cost-effective and effective reduction of muscle spasms.
The main drawback to neurolytic block is its temporary duration and the need to repeat the block when the previous block wears off. Selective obturator nerve block has also been used in the diagnosis and treatment of chronic pain states secondary to knee arthrosis or pelvic tumors resistant to conventional analgesic approaches.
Contraindications
Patient refusal, inguinal lymphadenopathy, perineal infection, or hematoma at the needle insertion site all are contraindications to obturator nerve block. Preexisting obturator neuropathy, clinically manifested by groin pain, pain of the posteromedial aspect at the thigh, and occasionally paresis of the adductor group of muscles, are relative contraindications to this block. Obturator nerve blocks should be avoided in the presence of a coagulopathy.
Anatomy
The obturator nerve is a mixed nerve, which, in most cases, provides motor function to the adductor muscles and cutaneous sensation to a small area behind the knee. It is derived from the anterior primary rami of L2, L3, and L4 (Figure 1). On its initial course, it runs within the psoas major muscle. Taking a vertical course, it emerges from the inner border of the psoas, staying medial and posterior at the pelvis until it crosses at the level of the sacroiliac joint (L5) under the common iliac artery and vein and runs anterior/lateral to the ureter (Figure 2).
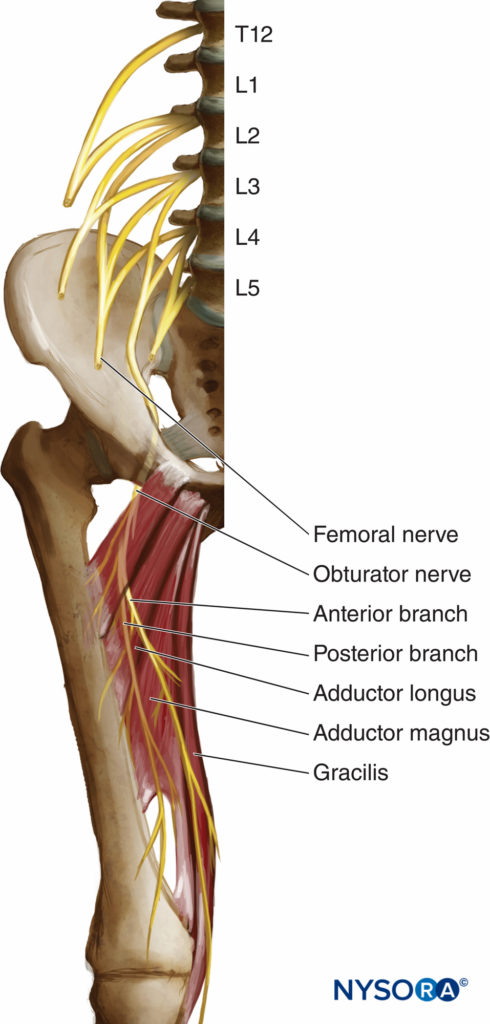
FIGURE 1. Anatomy of the obturator nerve.
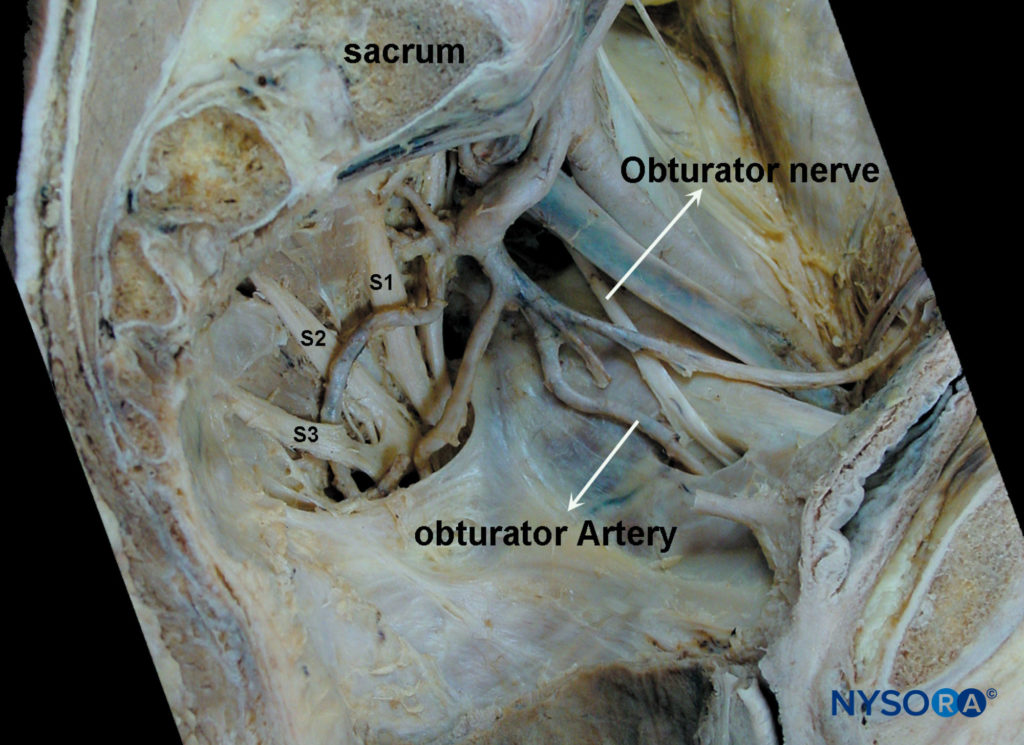
FIGURE 2. Intrapelvic trajectory of the obturator nerve. After crossing under the iliac vessels, the obturator nerve travels toward the obturator foramen via the lateral pelvic wall. During this course, the obturator artery and vein join the nerve, forming the obturator neurovascular bundle.
At this level, it courses close to the wall of the bladder on its inferior/lateral portion and then it takes place anterior to the obturator vessels within the superior part of the obturator foramen, exiting the pelvis below the pubic superior branch. In its intrapelvic course, the obturator nerve is separated from the femoral nerve by the iliopsoas muscle and iliac fascia. It innervates the parietal peritoneum on the lateral pelvic wall and contributes collateral branches to the obturator externus muscle and the hip joint. It leaves the pelvis by passing through the obturator canal before entering the adductor region of the thigh (Figure 3). Here, 2.5–3.5 cm after leaving the obturator foramen, the obturator nerve divides into its two terminal branches, anterior and posterior, providing innervation to the hip adductor compartment (Figure 3).
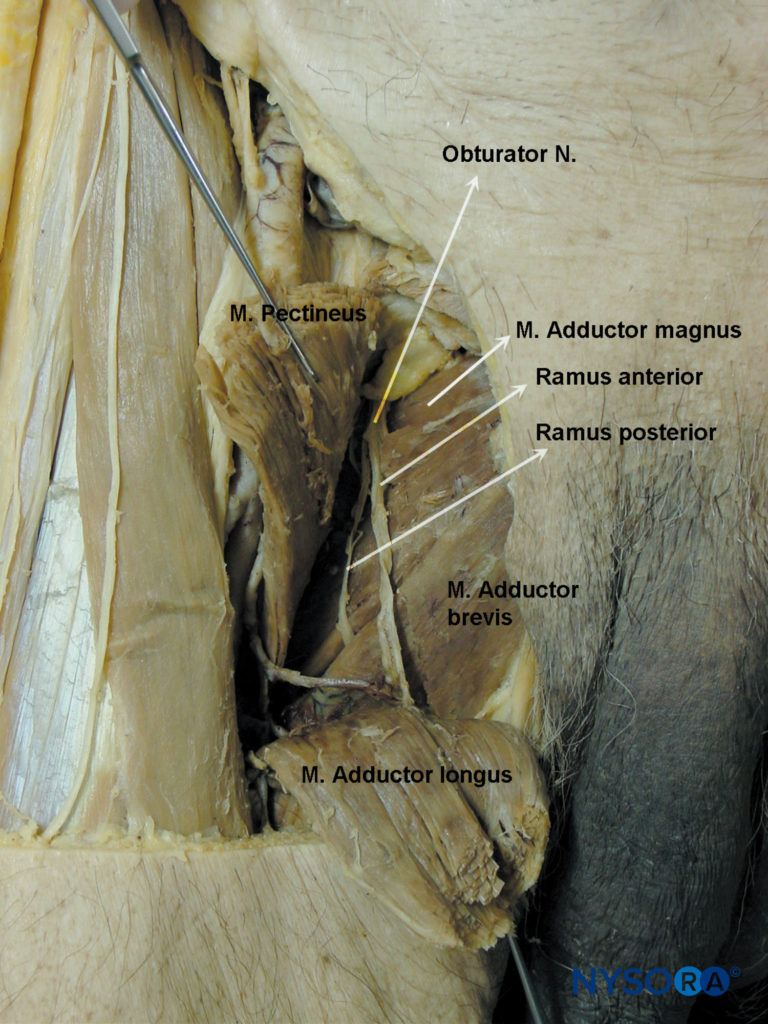
FIGURE 3. Distribution of the anterior and posterior divisions of the obturator nerve after exiting the obturator foramen.
The anterior branch descends behind the pectineus and adductor longus and in front of the obturator externus and adductor brevis. It gives muscular branches to the adductor longus, adductor brevis, gracilis, and occasionally the pectineus, and it terminates as a small nerve that innervates the femoral artery (Figure 4). In 20% of subjects, it contributes a branch, which anastomoses with branches of the femoral nerve and forms the subsartorial plexus, from which sensory branches emerge to supply sensation to posteromedial aspect of the inferior third of the thigh. The anterior branch contributes articular branches to anteromedial aspect of the hip joint capsule (Figure 5) but does not innervate the knee joint. Under ultrasound guidance, selective block of the anterior or posterior branches can be performed. Block of the anterior branch alone may be adequate for preventing the adductor reflex during bladder surgery.
The posterior branch descends between the adductor brevis in front and the adductor magnus behind. It terminates by passing through the adductor hiatus to enter the popliteal fossa, supplying the posterior aspect of the knee joint and the popliteal artery.
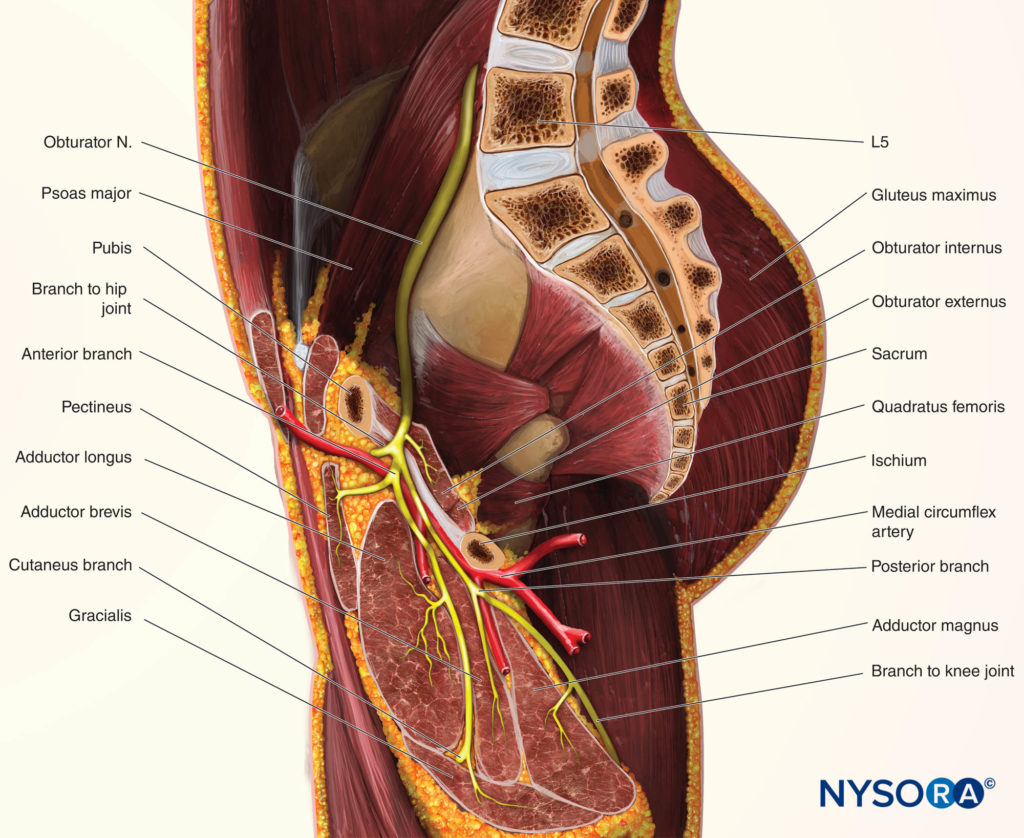
FIGURE 4. Sagittal section demonstrating the relationship of the obturator nerve to the adductor muscles.
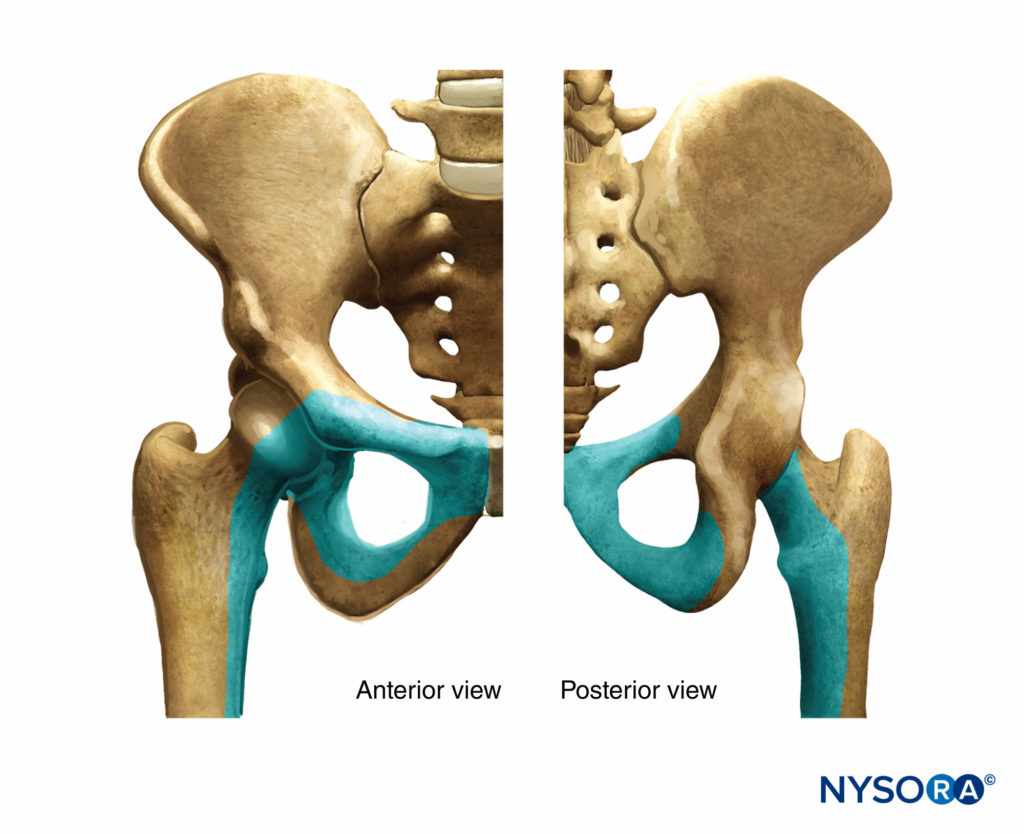
FIGURE 5. The role of the obturator nerve in the sensory innervation of the hip.
During its course, the posterior branch sends muscular branches to the obturator externus, the adductor magnus, and occasionally the adductor brevis muscles (see Figure 4).
Cutaneous innervation by the obturator nerve varies according to the investigators and is illustrated in Figure 6.
The functions of the muscles innervated by the obturator nerve are adduction of the thigh and assistance with hip flexion. The gracilis muscle assists knee flexion, and the obturator externus aids the lateral rotation of the thigh. To request an active adduction of the thigh, therefore, tests the function of the obturator nerve. The patient should be supine with knees extended. The leg is then adducted against resistance while the examiner supports the contralateral leg. The paralysis (or block) of the nerve is characterized by a severe weakening of the adduction, although it is not completely lost as the adductor magnus (the most powerful adductor muscle) receives fibers from the sciatic nerve and eventually from the femoral nerve.
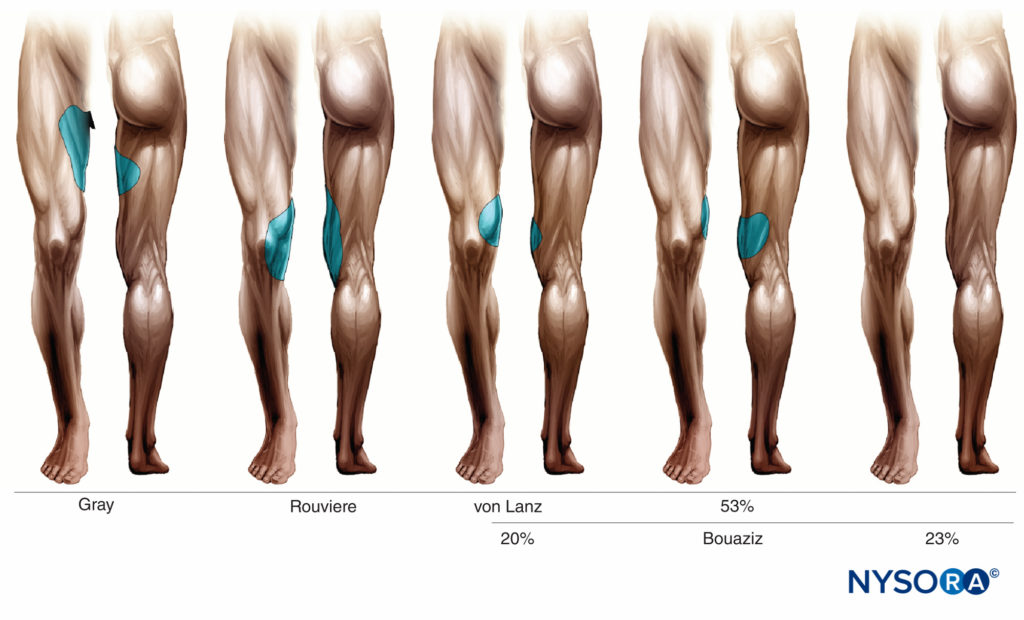
FIGURE 6. Skin innervation by obturator nerve according to different investigators.
Anatomic Variants
Numerous variations to the formation, course, and distribution of the obturator nerve can have clinical implications. For instance, in 75% of cases, the obturator nerve divides into its two terminal branches as it passes through the obturator canal. In 10% of cases, this division occurs before the nerve reaches the obturator canal; in the remaining 15% of cases, after entering the thigh.
Occasionally, the anterior and posterior branches descend through the thigh behind the adductor brevis. Note that the sensory cutaneous branch of the obturator nerve is often absent.
Up to 20% of subjects possess an accessory obturator nerve that can be formed from variable combinations of the anterior rami L2–L4 or emanate directly from the trunk of the obturator nerve. It accompanies the obturator nerve as it emerges from the medial border of the psoas, but unlike the obturator, passes in front of the superior pubic ramus to supply a muscular branch, the pectineus. It contributes articular branches to the hip joint and terminates by anastomosing with the obturator nerve itself.
Equipment
To perform a block, the following equipment is required:
- Nerve stimulator
- Insulated stimulating needle (5–8 cm, depending on the approach chosen)
- Local anesthetic: 1% mepivacaine (onset of motor block 15 min, duration 3–4 h) or 0.75% ropivacaine (on-set of motor block 25 min, block duration 8–10 h)
- Sterile fenestrated drape
- Marking pen
- Ruler
- A 10-mL syringe
- Disinfectant
- Sterile gloves
Learn more about Equipment for Regional Anesthesia.
Landmarks
Anatomic landmarks vary depending on the chosen approach. However, it is useful to identify and outline the following landmarks regardless of the approach chosen (Figure 7):
Bony landmarks: Anterior and superior iliac spine and pubic tubercle, inguinal ligament
Vascular landmarks: Femoral artery, femoral crease
Muscular landmarks: Tendon of the adductor longus muscle
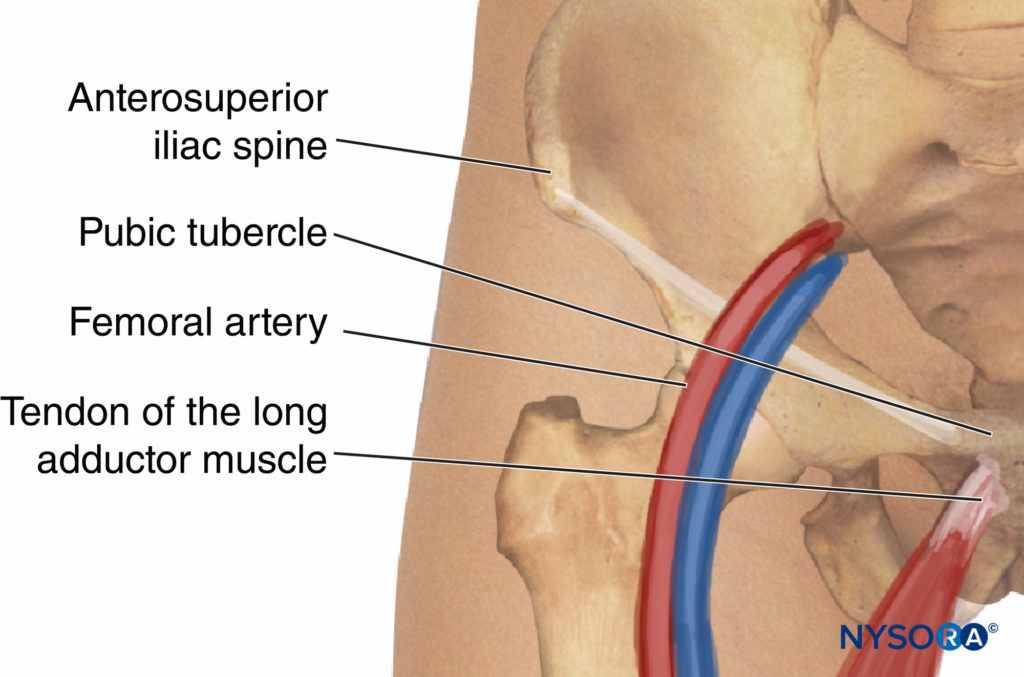
FIGURE 7. Anatomic landmarks for block of the obturator nerve.
Techniques
Several methods can accomplish block of the obturator nerve. These approaches can be grouped into plexus block techniques where the obturator nerve is blocked along with other components of the lumbosacral plexus and specific single-nerve block techniques for the obturator nerve.
3-in-1 Block Technique
Based on the theoretic existence of a suprainguinal compartment, in 1973 Winnie described the lumbar plexus block by an anterior approach or the “3 in 1 block”. According to the 3-in-1 concept, a large volume of local anesthetics is injected over the femoral nerve to spread underneath the fascia iliaca.
When combined with distal compression, the local anesthetic spreads proximally reaching the lumbar plexus. Unfortunately, studies have repeatedly failed to demonstrate the reliability of this technique to obtain a block of the lumbar plexus or the obturator nerve.
In addition, studies in human cadavers have documented the absence of a fluid-conducting compartment that would allow such an extensive proximal spread of the local anesthetic.
Of note, increasing the volume of injectate does not increase the spread toward the lumbar plexus; no differences were found when local anesthetic injection volumes of 20 or 40 mL were compared.
Theoretically, catheters inserted by an inguinal approach can ascend toward the psoas compartment, however, only a minor percentage (23%) of catheters can be adequately placed in the therapeutic position.
Iliofascial Block Technique
Dalens first described this approach in 1989 for use in pediatric patients. Following Winnie’s reasoning for the 3-in-1 block, he took a more lateral approach and reported a 100% success rate for femoral and femoral cutaneous nerve block and 88% success rate for the obturator nerve.
However, follow-up studies in adults did not confirm these results.
In adults, the iliofascial approach allows more successful block of the lateral femoral cutaneous nerve when compared with the 3-in-1 technique. However, the obturator nerve remains spared.
Psoas Compartment Block
Since Winnie’s description of the posterior approach to the lumbar plexus in 1974 (psoas compartment block), numerous modifications of the technique have been described. The obvious advantage is the ability to obtain a complete lumbar plexus block with a single injection. Indeed, studies have demonstrated femoral nerve block close to 100% plexus block with this technique, whereas femorocutaneous and obturator nerve blocks are anesthetized 88%–93% of the time.
Parasacral Sciatic Block
Mansour initially described this technique in 1993 with the objective of achieving a more complete sciatic nerve block.
Since this technique is a plexus block, it provides more consistent anesthesia of all branches of the sciatic nerve. It successfully blocks the posterior cutaneous nerve of the thigh, the gluteal superior and inferior nerves, and the pudendal nerve. In addition, the splanchnic nerves, the inferior hypogastric plexus, the proximal portion of sympathetic trunks, and the obturator nerve are located close to the point of injection.
Thus, a block of all these nervous structures would be theoretically achievable with a single injection. However, recent anatomic and clinical studies suggest that the parietal peritoneum and the pelvic fascia surrounding the sacral plexus are anatomically separated from the obturator nerve that runs along the medial border of the psoas. Consequently, although the parasacral approach to sciatic nerve block should result in a complete block of the sacral plexus, it is not reliable for obturator nerve block.
Selective Block Techniques
Labat’s Classic Technique
Labat’s classic approach was a common technique before the development of newer approaches that are easier to perform and less uncomfortable to patients. Originally described as a paresthesia method, the advent of nerve stimulation has increased the effectiveness and reduced patient discomfort, complications, and number of needle insertions. The procedure sequence consists of five phases, depicted in Figure 8.
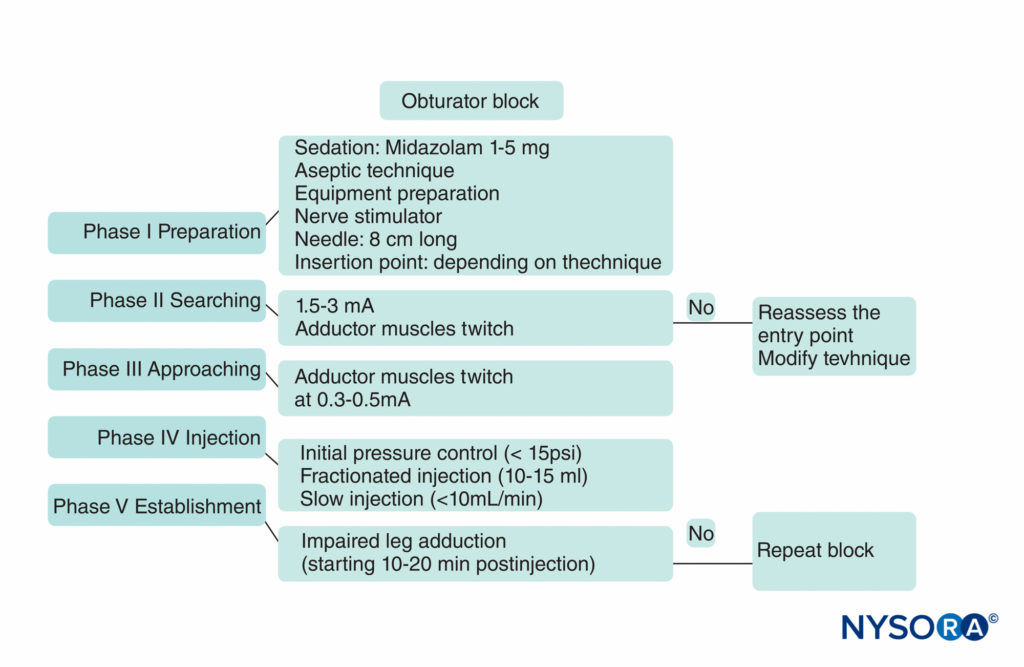
FIGURE 8. A practical algorithm to obturator nerve block.
Nerve stimulation is begun using a current intensity of 2–3 mA (2 Hz, 0.1–0.3 msec) and reduced to 0.3–0.5 mA before injection of local anesthetic. The patient lies supine, with the limb to be blocked at 30 degrees abduction. The pubic tubercle is identified by palpation, and a 1.5-cm long line is drawn laterally and caudally; the injection insertion site is labeled at the tip of the end of the caudal line (Figure 9). The classic approach consists of carrying out three consecutive movements of the needle until the tip of the needle is placed over the top of the obturator foramen, where the nerve runs before splitting into its two terminal branches. With a 22-gauge, 8-cm long needle, the skin is penetrated perpendicularly and the needle is advanced until it makes contact with the inferior border of the superior pubic branch at a depth of 2–4 cm. During the second phase, the needle is cm slightly withdrawn and then slipped along the anterior pubic wall (another 2–4 cm).
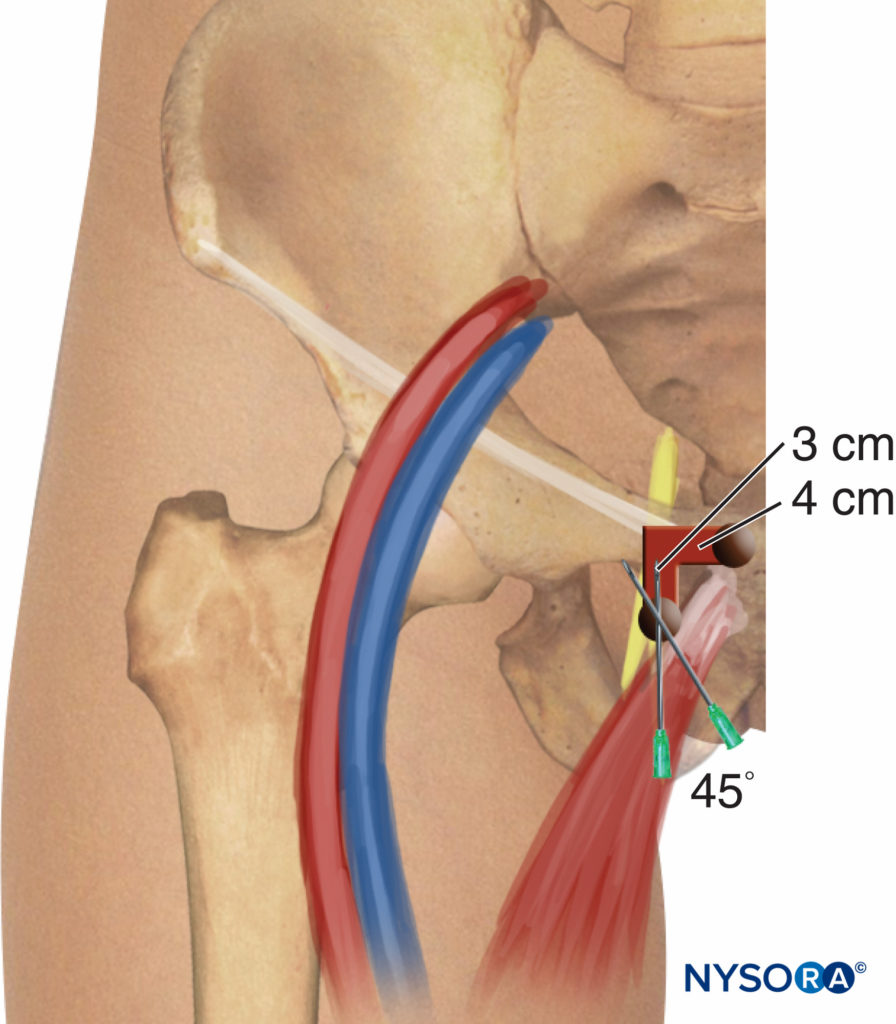
FIGURE 9. Obturator nerve block. Simplified Labat classic technique.
After this, it is redirected anteriorly/posteriorly. Finally, the needle is withdrawn again and slightly redirected (cephalad and laterally) at an angle of 45 degrees for another 2–3 cm until contractions of the thigh adductor muscles are observed.
This technique can be simplified by eliminating the second movement of the needle. Hence, after making contact with the pubic branch, the needle can be redirected 45 degrees laterally to the obturator foramen (see Figure 9).
Paravascular Selective Inguinal Block
This technique consists of a selective block of the two branches of the obturator nerve (anterior and posterior), performed at the inguinal level and slightly more caudad than the previously described techniques. The femoral artery and the tendon of the adductor longus muscle at the pubic tubercle are identified. For tendon identification, extreme leg abduction is required (Figure 10). A line is drawn over the inguinal fold from the pulse of the femoral artery to the tendon of the long adductor muscle. The needle is inserted at the midpoint of this line at an angle of 30 degrees anteriorly/posteriorly and cephalad (Figure 11). By following the needle a few centimeters in depth via the adductor longus muscle, twitches of the adductor longus and gracilis muscles are easily detectable on the posterior and medial aspect of the thigh. Subsequently, the needle is inserted deeper (0.5–1.5 cm) and slightly laterally over the adductor brevis muscle until a response from the adductor magnus muscle is obtained and can be visualized on the posterior-medial aspect of the thigh. After needle insertion, infiltration of 5–7 mL local anesthetic is recommended. Occasionally, a more caudal division of the obturator nerve is found; the two branches are located within the same location at the inguinal fold, and two different motor responses may be observed with a single injection.

FIGURE 10. Leg abduction.
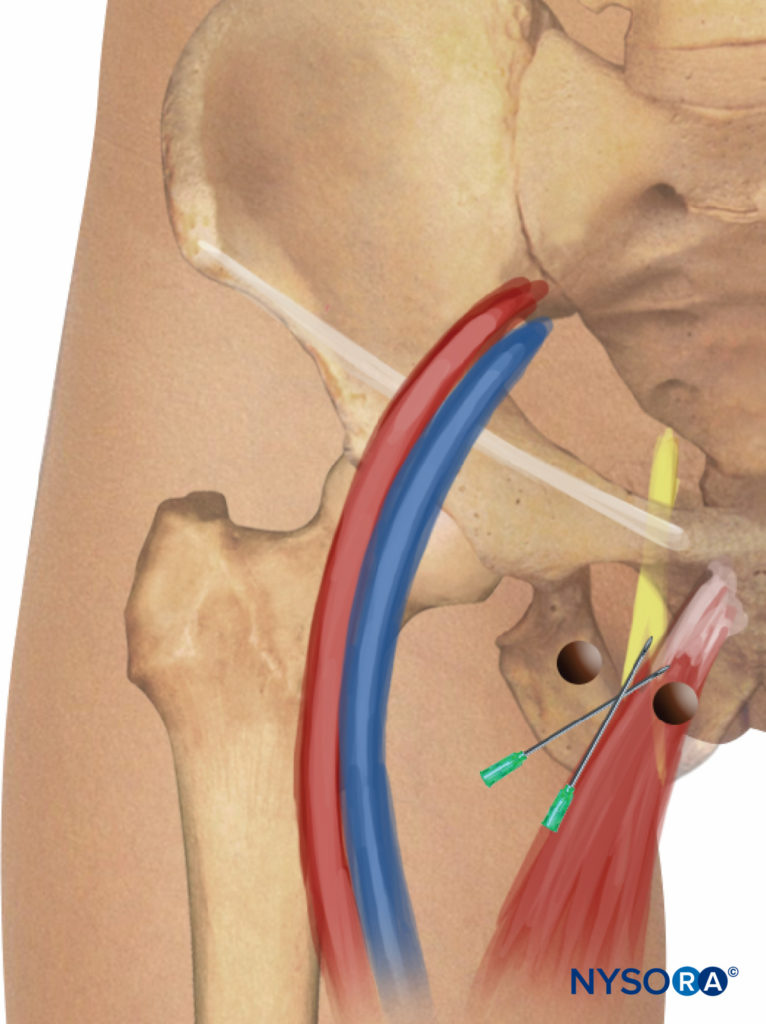
FIGURE 11. Paravascular selective inguinal approach to medial aspect of the knee.Needle insertion and redirection.
NYSORA Tips
• The inguinal approach to the obturator nerve is easier to perform and more comfortable to the patient.
• The needle insertion site with this approach is away from intrapelvic contents, resulting in a lower risk of complications.
• Articular branches to the hip joint are not blocked with this approach.
Choice of Local Anesthetic
Ten milliliters of local anesthetic is adequate. The type and concentration of the local anesthetic depend on the indication for the block. For diagnostic–therapeutic blocks, highly concentrated neurolytic solutions are used to achieve longlasting blocks. In the literature, combinations of phenol, ethanol, bupivacaine, levobupivacaine, and/or steroids are well reported.
For lower limb surgeries, the recommended anesthetic technique consists of the administration of medium- to long-lasting local anesthetics that are associated with adequate postoperative analgesia, such as bupivacaine 0.25%–0.5%; ropivacaine 0.25%, and levobupivacaine 0.25%–0.5%. To avoid adductor muscle spasms during transurethral surgery, the use of mediumto long-acting local anesthetics is not required because the surgery does not last more than 2 hours. Therefore, mepivacaine 1%–2% or lidocaine 1%–2% should be adequate for this purpose.
BLOCK EVALUATION
The onset of motor block is seen approximately 15 minutes after administration of 1% mepivacaine and 25 minutes after injection of 0.5% ropivacaine. Evaluation of an obturator block by sensory testing is unreliable due to the variability in its sensory distribution (see Figure 10). In some cases, the obturator nerve may not contain any sensory branches that can be clinically tested for adequacy of the block. In addition, even when a sensory branch is present, there is considerable overlap of cutaneous innervation from the obturator, femoral, and sciatic nerves. It is often erroneously thought that the skin of the medial aspect of the thigh is innervated by the obturator nerve; in fact, sensory branches of the femoral nerve contribute sensory innervation to this region.
NYSORA Tips
• Evaluation of an obturator block by sensory testing can be challenging because of the variability in its sensory distribution.
• The most common sensory innervation of the obturator nerve is the skin in a small region located on the postero-medial aspect of the knee.
• A considerable overlap of cutaneous innervation exists among the obturator, femoral, and sciatic nerves.
• Reduction in adduction strength is the most reliable means of demonstrating successful obturator nerve block.
The area of skin most commonly regarded as having exclusive obturator nerve supply is a small region located on the posteromedial aspect of the knee. Also, the strength of the lower limb adductors relies 70% on the obturator nerve. Consequently, reduction in the strength of the adductors of the thigh is the most reliable sign of successful obturator nerve block (Figure 10). Adductor muscle strength can be objectively evaluated by comparing the maximal pressure exerted by the patient squeezing a sphygmomanometer that has been preinflated to 40 mm Hg and placed between the legs before and after block performance. Failure to demonstrate a reduction in adductor muscle strength from baseline is synonymous with block failure.
PERIOPERATIVE MANAGEMENT
Patients must be warned that ambulation may be impaired because of the block of the thigh adductors.
COMPLICATIONS
There are no reports of complications associated with obturator nerve block. The lack of reported complications, however, is more likely due to the infrequent use of this block rather than to its inherent safety. Needle orientation for the classic pubic approach of Labat is toward the pelvic cavity. Therefore, if advanced too far in a cephalad direction, the needle can pass over the superior pubic ramus and penetrate the pelvic cavity, perforating the bladder, rectum, and spermatic cord. Accidental puncture of the obturator vessels could result in unintentional intravascular injection and hematoma formation. A retropubic anastamosis between the external iliac and obturator arteries (corona Mortis) is present in up to 10% of patients: bleeding secondary to puncture of the corona Mortis can be difficult to control. Obturator neuropathy, secondary to needle trauma, intraneural injection, nerve ischemia, or local anesthetic toxicity are also possible, as with other peripheral nerve block techniques.
REFERENCES
- Labat G: Regional Anesthesia: Its Technique and Clinical Application. Philadelphia, PA: Saunders, 1922.
- Parks CR, Kennedy WF: Obturator nerve block: a simplified approach. Anesthesiology 1967;28:775–778.
- Wassef M: Interadductor approach to obturator nerve block for spastic conditions of adductor thigh muscles. Reg Anesth 1993;18:13–17.
- Pinnock CA, Fischer HBJ, Jones RP: Peripheral Nerve block. London, UK: Churchill Livingstone, 1996.
- Winnie AP, Ramamurthy S, Durrani Z: The inguinal paravascular technic of lumbar plexus anaesthesia: the “3-in-1” block. Anesth Analg 1973;52:989–996.
- Kim PS, Ferrante FM: Cryoanalgesia: A novel treatment for hip adductor spasticity and obturator neuralgia. Anesthesiology 1998;89:534–536.
- Wheeler ME, Weinstein SL: Adductor tenotomy-obturator neurotomy. J Pediatr Orthop 1984;4:48–51.
- Benzel EC, Barolat-Romana G, Larson SJ: Femoral obturator and sciatic neurectomy with iliacus and psoas muscle section for spasticity following spinal cord injury. Spine 1988;13:905–908.
- Pelissier J: Chemical neurolysis using alcohol in the treatment of spasticity in the hemiplegic. Cah Anesthesiol 1993;41;139–143.
- Akat T, Murakami J, Yoshinaga A: Life-threatening haemorrhage following obturator artery injury during transurethral bladder surgery: sequel of an unsuccessful obturator nerve block. Acta Anaesthesiol Scand 1999;
43:784–788. - Shulm MS: Simultaneous bilateral obturator nerve stimulation during transurethral electrovaporizacion of the prostate. J Clin Anesth 1998;10:518–521.
- Prentiss RJ: Massive adductor muscle contraction in transurethral surgery: cause and prevention; development of new electrical circuit. Trans Am Assoc Genitourin Surg 1964;56:64–72.
- Shiozawa H: A new transurethral resection system: operating in saline environment precludes obturator nerve reflex. J Urol 2002;168:2665–2657.
- Biserte J: Treatment of superficial bladder tumors using the argon laser. Acta Urol Belg 1989;57:697–701.
- Brunken C, Qiu H, Tauber R: Transurethral resection of bladder tumours in physiological saline. Urologe 2004;43:1101–1105.
- Hobika JH, Clarke BG: Use of neuromuscular blocking drugs to counteract thigh-adductor spasm induced by electrical shocks of obturator nerve during transurethral resection of bladder tumors. J Urol 1961;
85:295–296. - Atanassoff PG, Weiss BM, Brull SJ: Lidocaine plasma levels following two techniques of obturator nerve block. J Clin Anesth 1996;8:535–539.
- Kakinohana M: Interadductor approach to obturator nerve block for transurethral resection procedure: comparison with traditional approach. J Anesth 2002;16:123–126.
- Deliveliotis C, Alexopoulou K, Picramenos D, et al: The contribution of the obturator nerve block in the transurethral resection of bladder tumor. Acta Urol Belg 1995;63:51–54.
- Schwilick R, Wingartner K, Kissler GV, et al: Elimination of the obturator reflex as a specific indication for dilute solution of etidocaine. A study of the suitability of a local anesthetic for reflex elimination in the 3-in-1 block technic. Reg Anesth 1990;13–610.
- Rubial M, Molins N, Rubio P, et al: Obturator nerve block in transurethral surgery. Actas Urol Esp 1989;13:79–81.
- Gasparich JP, Mason JT, Berger RE: Use of nerve stimulator for simple and accurate obturator nerve block before transurethral resection. J Urol 1984;132:291–293.
- Viel E, Pelissier J, Pellas F, et al: Alcohol neurolytic blocks for pain and muscle spasticity. Neurochirurgie 2003;49:256–262.
- Viel E.J, Peennou D, Ripart J, et al: Neurolytic block of the obturator nerve for intractable spasticity of adductor thigh muscle. Eur J Pain 2002;6:97–104.498
- Kirazli Y, On AY, Kismali B, et al: Comparison of phenol block and botulinus toxin type A in the treatment of spastic foot aster stroke. A randomized double-blind trial. Am J Phys Med Rehabil 1998;77:510–515.
- Loubser PG: Neurolytic interventions for upper extremity spasticity associated with head injury. Reg Anesth 1997;22:386–387.
- Heywang-Kobrunner SH, Amaya B, Okoniewski M, et al: CT-guided obturator nerve block for diagnosis and treatment of painful conditions of the hip. Eur Radiol 2001;11:1047–1053.
- Hong Y, O’Grady T, Lopresti D, et al: Diagnostic obturator nerve block for inguinal and back pain: a recovered opinion. Pain 1996;67:507–509.
- Edmonds-Seal J, Turner A, Khodadadeh S, et al: Regional hip block in osteoarthrosis. Effects on pain perception. Anaesthesia 1982;37:147–151.
- James CDT, Little TF: Regional hip block. A simplified technique for the relief of intractable osteoarthritic pain. Anaesthesia 1976;31:1060–1070.
- Sunderland S: Obturator nerve. In Sunderland S (ed): Nerves and Nerve Injuries. Edinburgh, Scotland: Livingstone, 1968, pp 1096–1109.
- Whiteside JL, Walters MD: Anatomy of the obturator region: Relations to a trans-obturatorsling. Int Urogynecol J Pelvic Floor Dys- funct 2004;15:223–226.
- Sinha SK, Abrams JH, Houle TT, Weller RS: Ultrasound-guided obturator nerve block: an interfascial injection approach without nerve stimulation. Reg Anesth Pain Med 2009;34:261–264.
- Taha AM: Brief reports: ultrasound-guided obturator nerve block: a proximal interfascial technique.. Anesth Analg 2012;114:236–239.
- Manassero A, Bossolasco M, Ugues S: Ultrasound-guided obturator nerve block: interfascial injection versus a neurostimulation-assisted technique. Reg Anesth Pain Med. 2012;37:67–71.
- Falsenthal G: Nerve blocks in the lower extremities: anatomic considerations. Arch Phys Med Rehabil 1974;55:504–507.
- Parkinson SK, Mueller JB, Little WL, et al: Extend of block with various approaches to the lumbar plexus. Anesth Analg 1989;68:243–248.
- Brindenbaugh PO, Wedel DJ. The lower extremity. Somatic block. In Cousins MJ, Brindenbaugh PO (eds): Neural Blockage in Clinical Anesthesia and Management of Pain. Philadelphia, PA: Lippincott-Raven, 1998, pp 373–394.
- Atanassoff PG, Weiss BM, Brull SJ, et al: Electromyographic comparison of obturator nerve block to three-in-one block. Anesth Analg 1995;81:529–533.
- Ritter JW: Femoral nerve “sheath” form inguinal paravascular plexus block is not found in human cadavers. J Clin Anesth 1995;7:470–473.
- Seeberger MD, Urwyler A: Paravascular lumbar plexus extension after femoral nerve stimulation and injection of 20 vs 40 ml mepivacaine 10 mg/kg. Acta Anesthesia Scand 1995;39:769–813.
- Singelyn FJ, Gouverneur JM, Gribomont BF: A high position of the catheter increases the success rate of continuous 3-in-1 block. Anesthesiology 1996;85:A723.
- Capdevila X, Biboulet P, Morau D, et al: Continuous 3-in-1 block for postoperative pain after lower limb orthopedic surgery: where did the catheter go? Anesth Analg 2002;94:1001–1006.
- Dalens B, Vanneuville G, Tanguy A: Comparison of the fascia iliac block with the 3-in-1 block in children. Anesth Analg 1989;69:705–713.
- Morau D, Lopez S, Biboulet P, et al: Comparison of continuous 3-in-1 and fascia iliaca compartment blocks for postoperative analgesia: feasibility, catheter migration, distribution of sensory block, and analgesic efficacy. Reg Anesth Pain Med 2003;28:309–314.
- Capdevila X, Biboulet P, Bouregba M, et al: Compartment of the 3-in-1 and fascia iliaca compartment block in adults: clinical and radiographic analysis. Anesth Analg 1998;86:1039–1044.
- Winnie AP, Ramamurthy S, Durrani Z, et al: Plexus blocks for lower extremity surgery. Anesthesiol Rev 1974;1:1–6.
- Chayen D, Nathan H, Chayen M: The posterior compartment block. Anesthesiology 1976;45:95–99.
- Hanna MH, Peat SJ, D’Costa F: Lumbar pexus block: an anatomical study. Anaesthesia 1993;48:675–678.
- Chupfer G, Jöhr M: Psoas compartment block in children: Part I—Description of the technique. Pediatric Anesth 2005;15:461–464.
- Pandin PC, Vandesteen A, d’Hollander AA: Lumbar plexus posterior approach: a catheter placement description using electrical nerve stimulation. Anesth Analg 2002;95:1428–1431.
- Awad IT, Duggan EM: Posterior lumbar plexus block: anatomy, approaches, and techniques. Reg Anesth Pain Med 2005;30:143–149.
- Mansour NY: Reevaluating the sciatic nerve block: Another landmark for consideration. Reg Anesth 1993;18:322–323.
- Morris GF, Lang SA, Dust WN, et al: The parasacral sciatic nerve block. Reg Anesth 1997;22:223–228.
- Jochum D, Iohom G, Choquet, et al: Adding a selective obturator nerve block to the parasacral sciatic nerve block: an evaluation. Anesth Analg 2004;99:1544–1549.
- Choquet O, Nazarian S, Manelli H: Bloc obturateur au pli in- guinal: étude anatomique. Ann Fr Anesth Réanim 2001;20:131s.
- Fujita Y, Kimura K, Furukawa Y, et al: Plasma concentrations of lignocaine alter obturator nerve block combined with spinal anaesthesia in patient undergoing transurethral resection procedures. Br J Anaesth
1992;68:596–598.