Intrathecal opioids in kidney transplantation: A game changer for postoperative pain management
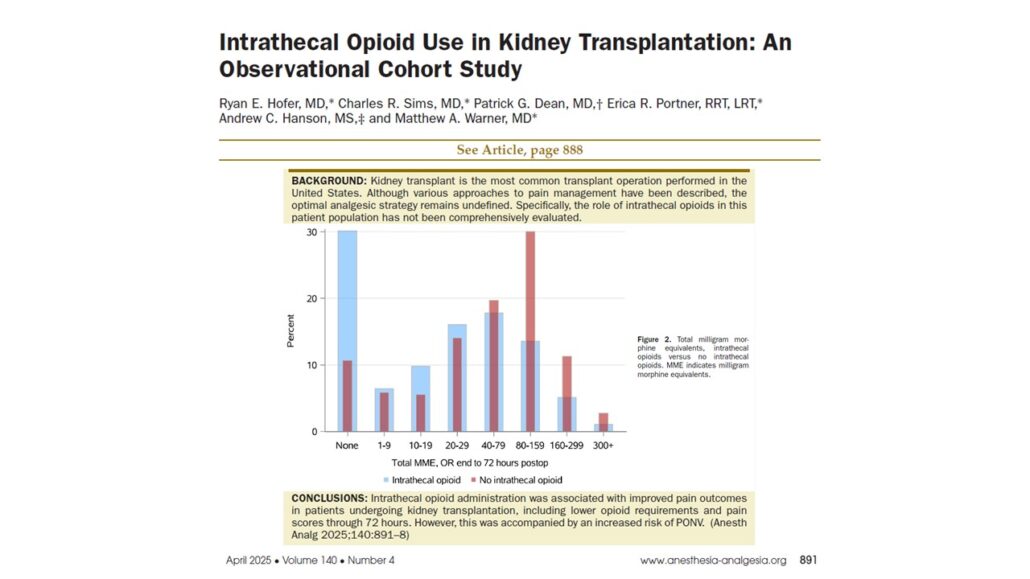
An observational study published in Anesthesia & Analgesia by Hofer et al. 2025 sheds new light on a transformative approach to managing postoperative pain in kidney transplant recipients. This retrospective cohort study found that preoperative administration of intrathecal hydromorphone is associated with significantly reduced postoperative opioid requirements and improved pain control, without increasing serious complications.
As kidney transplant surgery remains the most commonly performed transplant procedure in the United States, enhancing postoperative recovery and comfort is crucial. This new data suggests intrathecal analgesia could be pivotal in evolving perioperative care protocols.
Study summary
- Design: Retrospective observational cohort
- Period: August 1, 2017 – July 31, 2022.
- Location: Mayo Clinic, Rochester, MN.
- Population: 1,014 kidney transplants in 1,012 patients.
- Intervention: Preoperative intrathecal hydromorphone (median dose: 100 µg).
- Primary Outcome: 72-hour postoperative opioid use (measured in MME).
- Secondary Outcomes: Total MME (including intraoperative), pain scores at 24 and 72 hours, incidence of PONV (postoperative nausea and vomiting), pruritus, naloxone administration, and hospital length of stay
Key findings
- Reduced opioid requirements
One of the most notable outcomes of the study was the dramatic reduction in opioid use among patients who received intrathecal opioids.
- 72-hour postoperative MME:
- Intrathecal group: 30 mg (IQR 0–68)
- Non-intrathecal group: 64 mg (IQR 22–120)
- Adjusted reduction: 66%
- Total MME (intraoperative + postoperative):
- 42% lower in the intrathecal group
These findings highlight the potential of neuraxial opioid techniques to drastically reduce systemic opioid burden in a patient population that often presents with comorbidities and renal clearance challenges.
- Improved pain control
Pain scores—measured using the Numeric Rating Scale (NRS)—were consistently lower in the intrathecal group:
- At 24 hours post-op:
- Intrathecal group median: 4/10
- Non-intrathecal group: 7/10
- At 72 hours:
- Intrathecal: 6/10
- Non-intrathecal: 7/10
These differences were both statistically and clinically significant, and more pronounced in opioid-naïve patients.
- Elevated PONV risk
While analgesia improved, the intrathecal group experienced higher rates of postoperative nausea and vomiting:
- Incidence of PONV:
- Intrathecal group: 55%
- Non-intrathecal group: 38%
- Odds ratio: 2.16
This increase, while substantial, is manageable through targeted antiemetic prophylaxis and patient-specific planning.
- Safety profile
Despite increased PONV, no significant increase in serious adverse events was observed:
- Respiratory depression: None reported
- Naloxone use: Only one patient required administration
- Hospital length of stay: Median of 3 days in both groups
These findings suggest that intrathecal opioid administration, when properly monitored, is a safe technique in this complex surgical population.
Clinical implications
This study carries significant implications for transplant anesthesiology and perioperative care planning.
- For anesthesiologists and surgical teams:
- Lower opioid burden supports faster recovery and reduced risk of opioid-related complications (e.g., ileus, delirium, respiratory depression).
- Improved pain control facilitates early mobilization, potentially reducing other postoperative complications.
- Safety confirmed with no increase in respiratory events or length of stay, reinforcing its feasibility in high-risk populations.
- Patient selection criteria:
- Ideal candidates: Stable coagulation profile (platelets ≥100×10⁹/L, INR ≤1.2), no infection at the puncture site, and no contraindications to neuraxial techniques.
- Best outcomes observed in opioid-naïve patients, with pronounced reductions in pain and opioid use.
How to implement: Step-by-step approach
- Patient screening
- Exclude patients with coagulopathy or thrombocytopenia.
- Confirm absence of spinal infection or increased intracranial pressure.
- Intrathecal procedure
- Administer hydromorphone (typical dose: 100 µg) before induction.
- Use aseptic technique with standard neuraxial equipment.
- Standardized monitoring
- Continuous monitoring post-op: respiratory rate, oxygen saturation, heart rate, and blood pressure.
- Mandatory for the first 24 hours after PACU discharge.
- Antiemetic prophylaxis
- Standardize the use of agents like ondansetron or dexamethasone.
- Consider multi-agent antiemetic therapy in high-risk patients.
- Postoperative pain protocol
- Utilize multimodal analgesia with limited systemic opioids.
- Educate staff on expected lower opioid needs in intrathecal recipients.
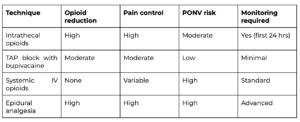
Comparison of analgesic strategies in kidney transplantation
Limitations of the study
- Retrospective design: Relies on EMR data; risk of bias or missing data
- No protocol standardization: Doses and antiemetics varied by provider
- No assessment of patient satisfaction: Pain scores do not capture holistic recovery
- Potential provider bias: Awareness of intrathecal administration may have altered postoperative opioid prescribing behavior
Future research
- Optimal intrathecal dosing protocols specific to renal transplant recipients
- Strategies to mitigate PONV in high-risk patients
- Prospective, randomized controlled trials to validate findings
- Incorporating patient-reported outcomes and long-term follow-up data
Conclusion
This large-scale observational study supports intrathecal opioid administration as a safe and effective strategy to improve postoperative outcomes in kidney transplant recipients. By substantially reducing opioid needs and pain scores, particularly in opioid-naïve patients, while maintaining a favorable safety profile, intrathecal analgesia presents itself as a powerful tool in modern transplant anesthesiology. However, it is not without trade-offs. The increased incidence of PONV must be addressed through careful planning and individualized care. As Enhanced Recovery After Surgery (ERAS) principles gain traction in organ transplantation, intrathecal analgesia emerges as a leading technique for delivering measurable clinical benefit and a better patient experience.
For more information, refer to the full article in Anesthesia & Analgesia.
Hofer, RE, Sims, Charles R, Dean PG, Portner ER, Hanson AC, Warner MA. Intrathecal opioid use in kidney transplantation: an observational cohort study. Anesthesia & Analgesia 140(4):p 891-898, April 2025.
Read more about kidney transplantation in our Anesthesiology Manual: Best Practices & Case Management.