SPINAL OR GENERAL ANESTHESIA FOR HIP FRACTURE
I invite all of my anesthesiology colleagues, particularly those with expertise in regional anesthesia, to act now to atone the conclusion of the studies on Spinal versus General Anesthesia for Patients with Hip Fracture that is, potentially, harmful, both to our patients and to our profession.
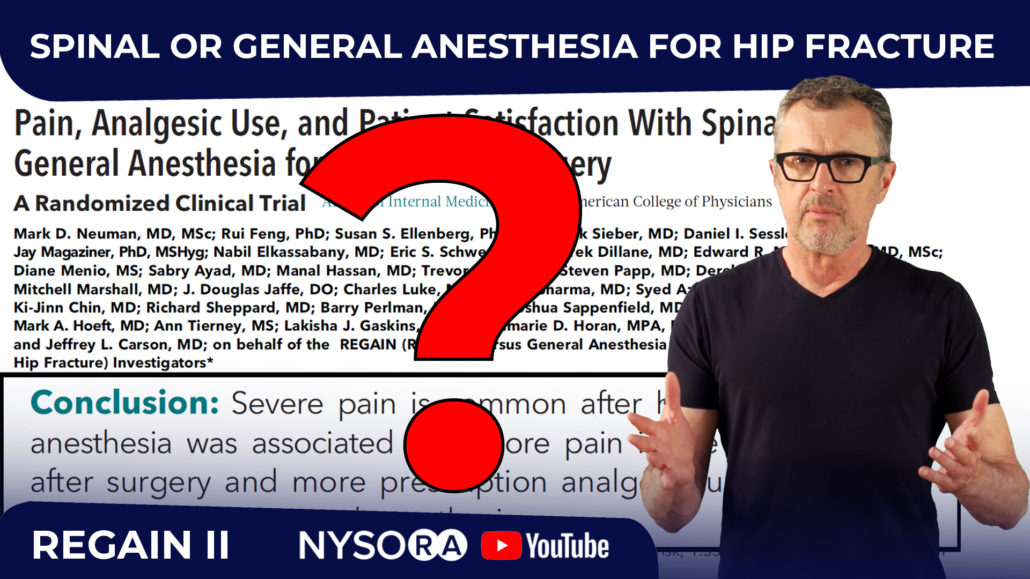
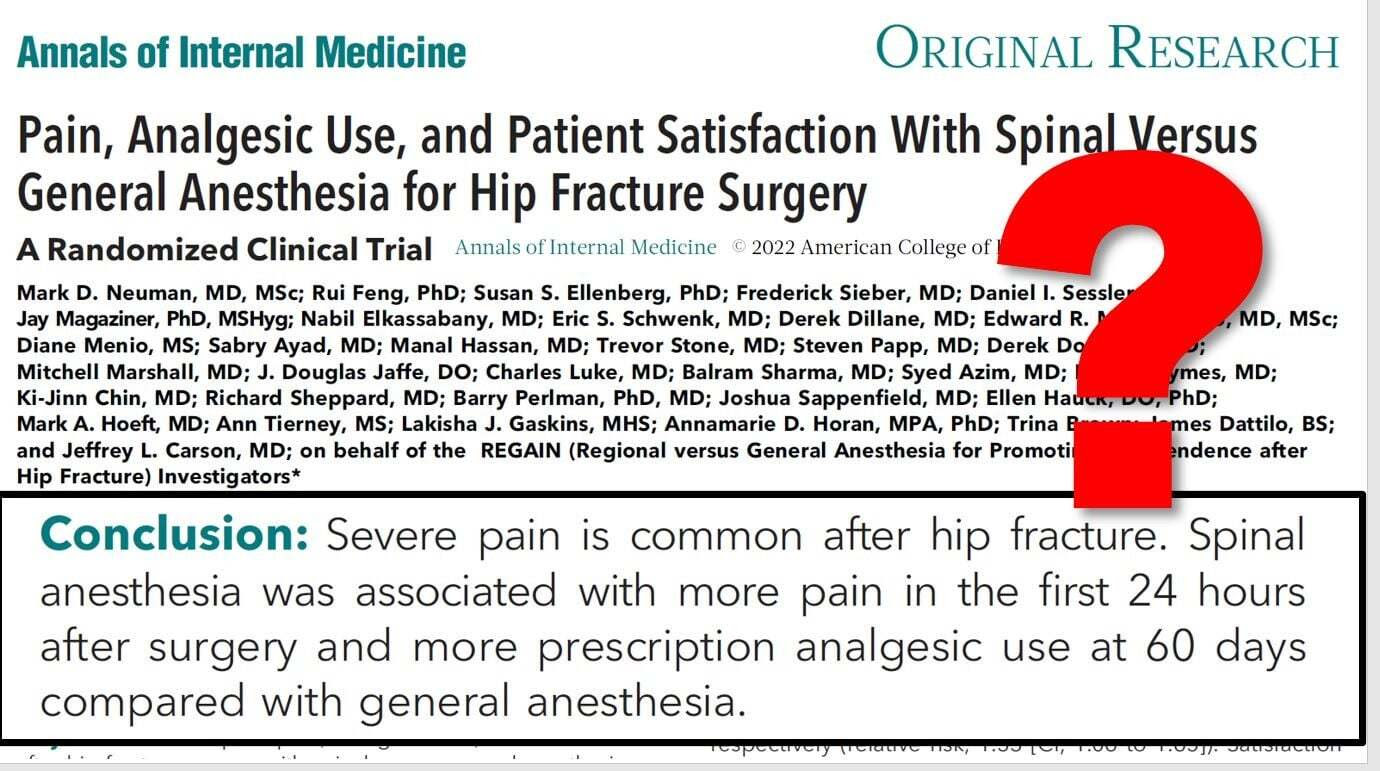
I refer to two articles published by Dr. Neuman and colleagues, in the New England Journal of Medicine (NEJM) (2021)(1) and the Annals of Internal Medicine (2022)(2), respectively, on the relative merits of spinal anesthesia versus general anesthesia conducted on patients with a hip fracture.
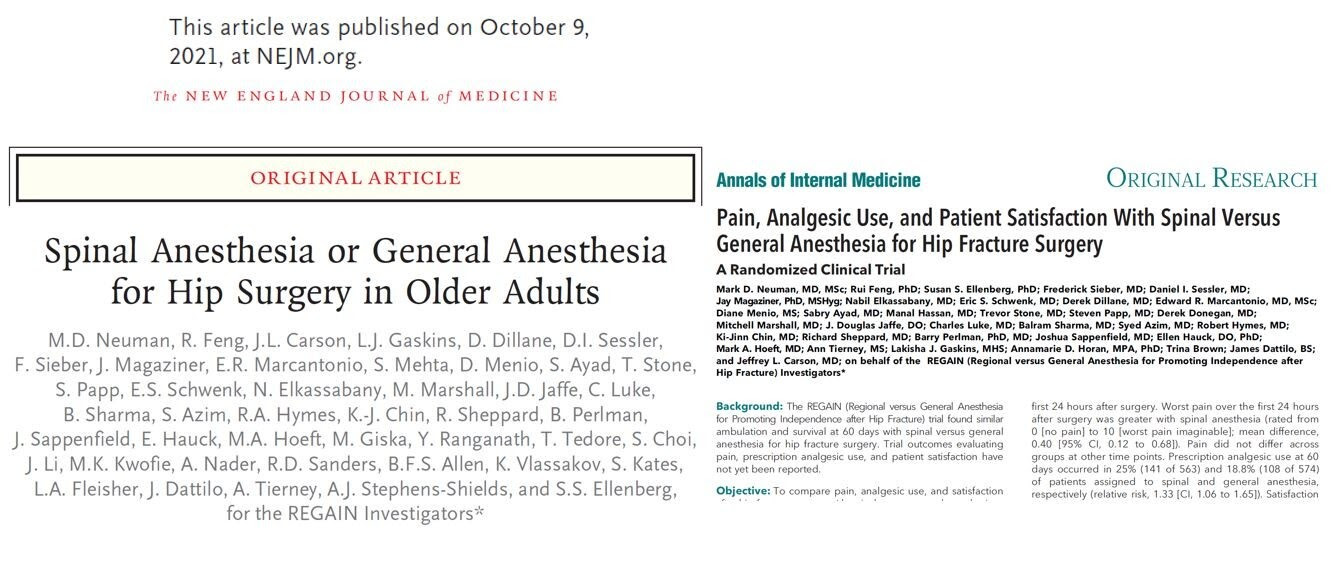
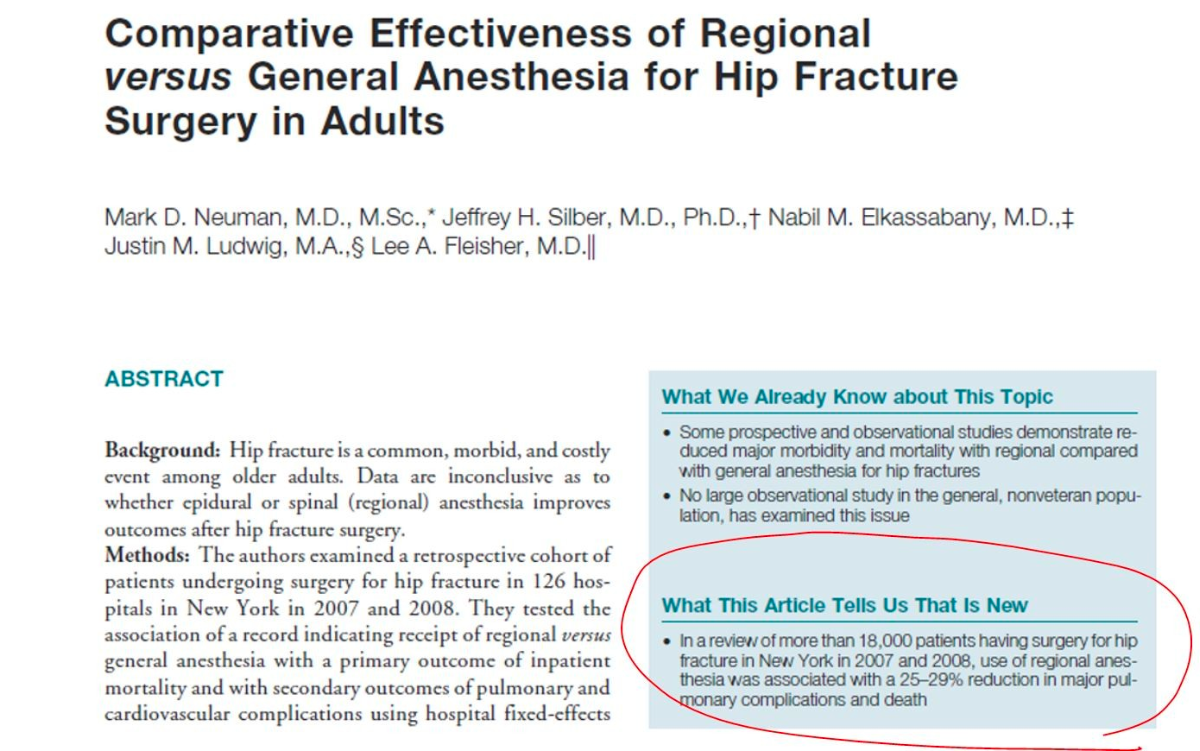
Previous studies(3,4), including those by the same author (Dr. Neuman), on much larger data sets, have clearly documented that spinal anesthesia saves lives and has been shown to decrease the mortality rate, and pulmonary complications by 30%(3).
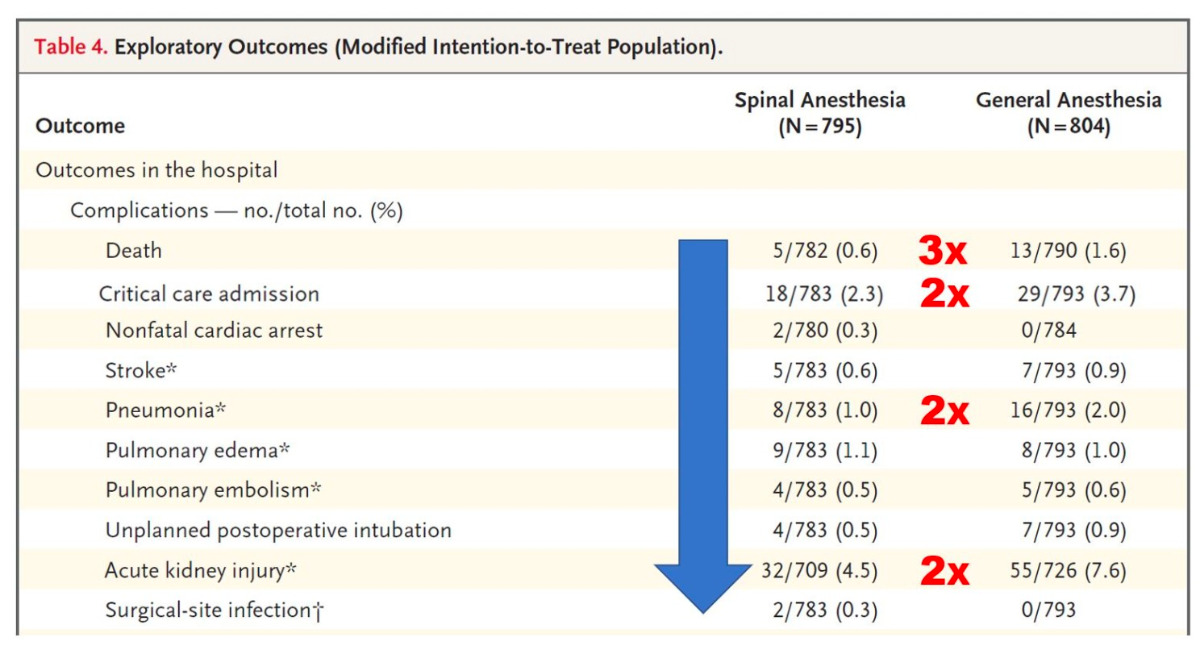
However, the current study(1) conducted in 30 institutions and involving 1,600 patients – has reported that there is no difference in outcome and that spinal anesthesia results in more postoperative pain and use of prescription analgesics.
Unfortunately, these findings, which are crafted too definitively, are misleading and have the potential to instil a negative perception of spinal anesthesia in surgeons, internal medicine specialists, and patients alike.
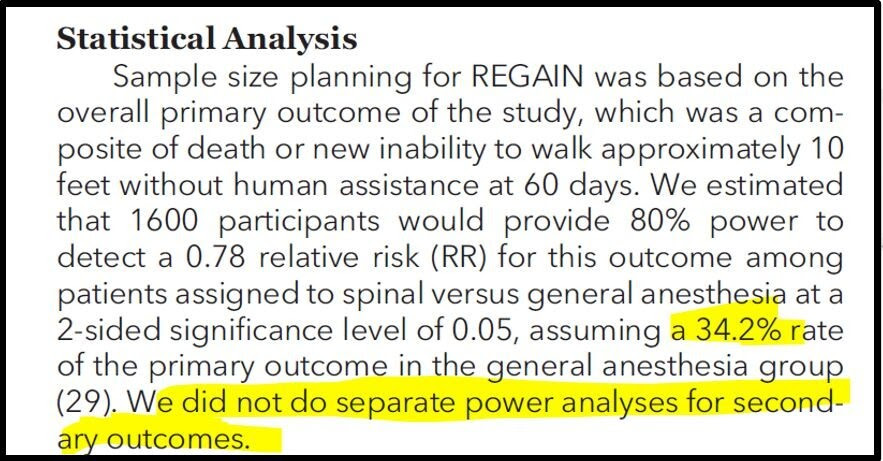
The first study(1), in the NEJM, concludes that there was no difference in outcome between spinal and general patients with a hip fracture. However, the study was powered based on the composite outcome (death at 60 days), assuming that the outcome would be 34%. Since death at 60 days in the study was only 18%, it is clear that the population in this study was much healthier than that typically encountered in typical clinical practice. Moreover, 15% of patients randomized for spinal had to cross to general anesthesia due to the inability or failure of spinal anesthesia. These data indicate that the practitioners who performed spinal anesthesia in this study were experts in general, and not in regional, anesthesia.
The benefits of spinal anesthesia in very ill patients are obvious to anyone who practices clinical anesthesiology. Spinal anesthesia requires less invasive monitoring and hemodynamic interventions. While this may not be reflected in composite death as an outcome at 60 days, spinal anesthesia results in a much more stable postoperative course and a lower burden of care. Since the study by Dr. Neuman based its findings solely on the comparison of composite death rates and the ability to walk independently at 60 days, these outcomes are simply too crude to distinguish the myriad of obvious differences between spinal and general anesthesia that are not a matter of life and death. Dr. Neuman’s previous studies in a much larger population clearly documented the advantages of spinal anesthesia over general(3,4).
|
|
In this study, general anesthesia was performed according to the protocol, whereas spinal anesthesia was conducted without any protocol. As an example, we do not know what premedication was used for positioning the patients for the spinal anesthesia, the level of neuraxial block achieved, or what doses were administered. Also, there remains the possibility that patients were just put to sleep in order to perform the spinal anesthesia. Likewise, intraoperative sedation was mandates for patients receiving spinal anesthesia, which may have contributed to biased information concerning the incidence of delirium postoperatively.
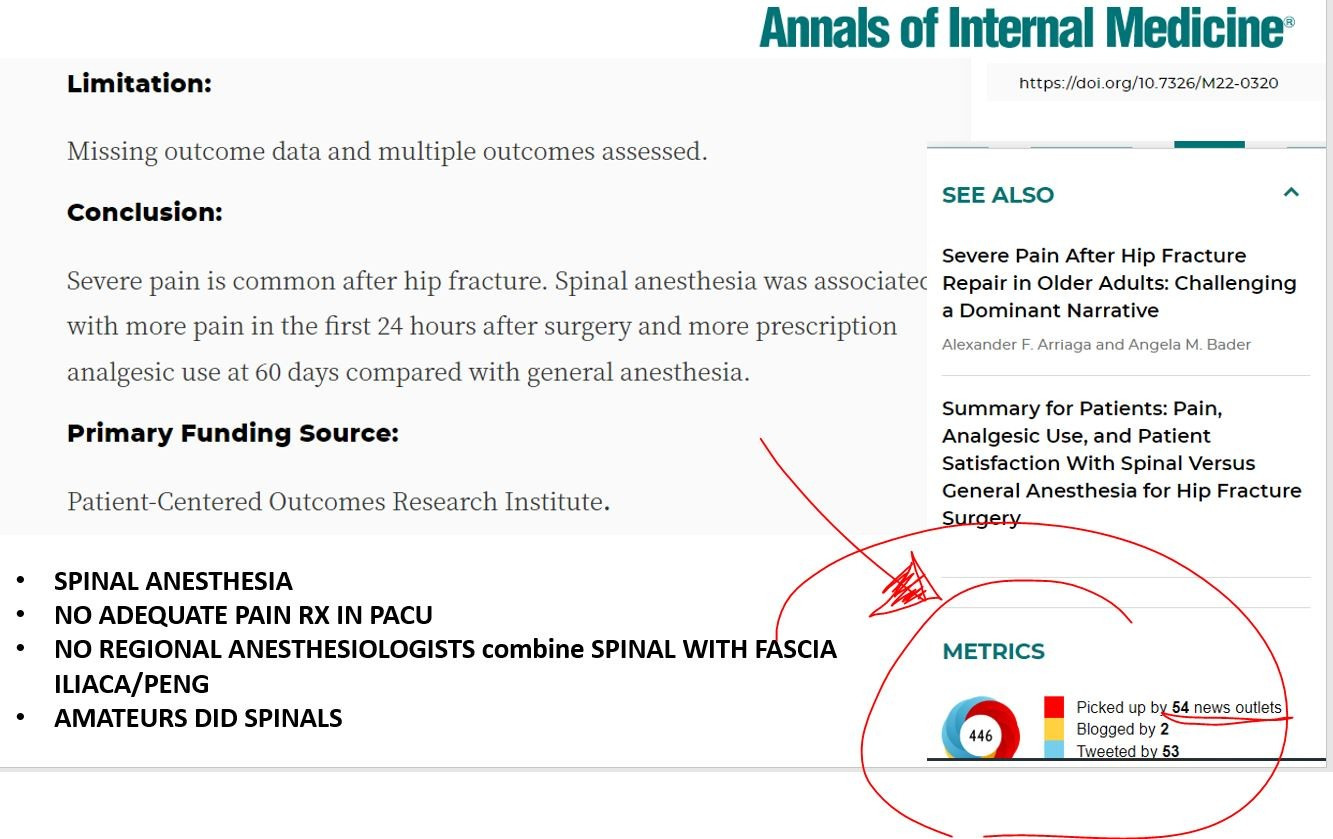
Our concern is that the widespread dissemination of this data, published in some of the most prestigious journals of medicine, has the potential to mislead our colleagues, internists, surgeons, and, perhaps, patients, in its inference that spinal anesthesia does not make a difference. The consequences may even deprive very ill patients of, what are sometimes, life-saving anesthesia techniques. Some of the very co-authors of these articles who have seen my video rebuffing the NEJM article on YouTube have asked me for another video to atone for unjust conclusions from the Neuman et al. Annals of Internal Medicine (2022) article.
With these considerations, it is imperative that we draw attention to the shortcomings of the conclusions of these two published studies, based as they were on a healthy population, which did not include very sick patients. It is vital that we do not allow such potentially harmful conclusions, based on flawed premises, to permeate our profession unchallenged. So, I invite you, colleagues, and fellow professionals, to have your say and be vocal about this and educate your colleagues surgeons, internists and patients that spinal anesthesia can be life-saving in severely ill patients, and that spinal anesthesia does not result in more postoperative pain than general anesthesia.
References
- Mark D. Neuman et al. Spinal Anesthesia or General Anesthesia for Hip Surgery in Older Adults. N Engl J Med 2021; 385:2025-2035.
- Mark D Neuman et al. Pain, Analgesic Use, and Patient Satisfaction With Spinal Versus General Anesthesia for Hip Fracture Surgery: A Randomized Clinical Trial. Ann Intern Med 2022.
- Mark D Neuman et al. Comparative Effectiveness of Regional Versus General Anesthesia for Hip Fracture Surgery in Adults. Anesthesiology 2012; 117(1):72-92.
- Jiabin Liu et al. Neuraxial Anesthesia Decreases Postoperative Systemic Infection Risk Compared with General Anesthesia in Knee Arthroplasty. Anesth Analg 2013; 117(4):1010-1016.