Perioperative pulmonary complications are among the most frequent causes of morbidity and extended hospital stays following surgery. With the advent of point-of-care ultrasound (POCUS), clinicians now have an accessible, noninvasive, and highly sensitive tool to assess lung aeration dynamically.
What is lung ultrasound and why is it important?
Lung ultrasound is a bedside imaging technique used to assess lung aeration and detect pathological changes in the lungs. Unlike static imaging modalities such as chest X-ray or CT scans, lung ultrasound provides real-time visualization of lung dynamics, making it an ideal tool during and after surgical procedures.
Why it’s gaining traction
- Diagnostic accuracy: Detects pneumothorax, pleural effusion, pulmonary edema, and atelectasis more sensitively than X-rays.
- Accessibility: Portable, affordable devices that connect to tablets and smartphones.
- Safety: No radiation exposure.
- Usability: Easy integration into standard perioperative protocols.
During the COVID-19 pandemic, LUS proved vital in the bedside assessment of lung conditions, reinforcing its relevance in routine and emergency care settings.
Ultrasound techniques and transducer types
Transducer orientation
- Longitudinal (sagittal) orientation: Marker faces cephalad; visualizes intercostal muscles and pleura.
- Transverse (axial) orientation: Rotated 90°; enhances detection of subtle atelectasis and extends pleural visibility.
Transducer selection
- Linear (high-frequency): Superior resolution for pleural line and lung sliding.
- Curvilinear or phased-array (low-frequency): Better for deep structures and B-lines; phased array is ideal for intercostal spaces.
Interpreting lung ultrasound: What does normal vs. abnormal look like?
Normal findings
- Lung sliding: A shimmering of the pleural line as visceral and parietal pleura move during respiration.
- A-lines: Horizontal reverberation artifacts; signify well-aerated lung tissue.
- Lung pulse: Rhythmic motion synchronized with the heart; excludes pneumothorax.
Indicators of impaired aeration
- B-lines: Vertical, laser-like artifacts indicating interstitial syndrome or fluid.
- Subpleural consolidations: Small focal areas of collapse beneath the pleural line.
- Dense consolidations: “Lung hepatization” – lung tissue resembling liver in echotexture due to complete air loss.
These abnormal findings help diagnose degrees of atelectasis and fluid overload, aiding intraoperative management.
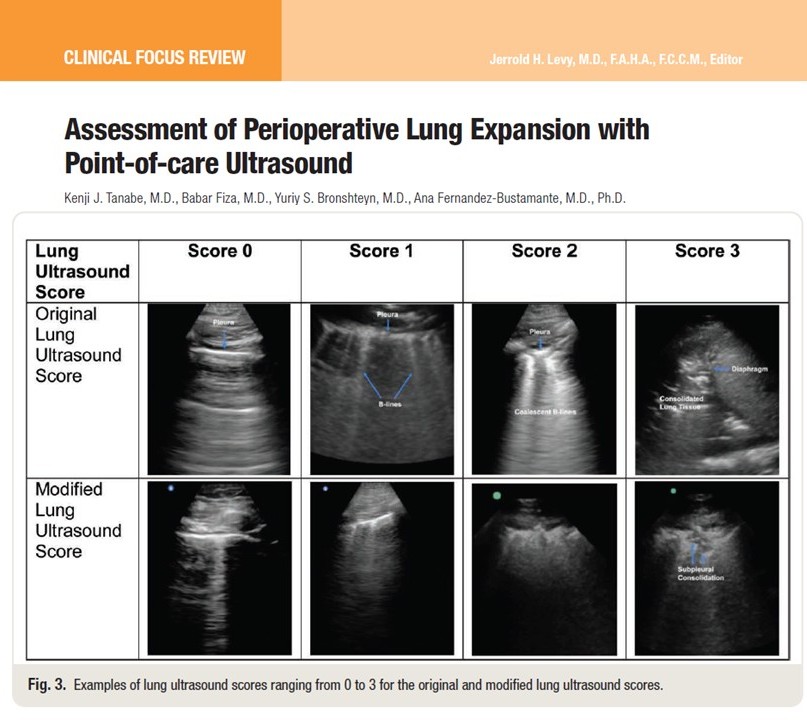
Lung ultrasound scoring systems
To quantify lung aeration, standardized scoring systems are used:
1. Original lung ultrasound score (OLUS)
- Regions scanned: 12 (upper/lower anterior, lateral, and posterior on both sides)
- Scoring:
- 0: Normal aeration
- 1: ≥3 B-lines
- 2: Coalescent B-lines
- 3: Consolidation
- Total score range: 0–36
2. Modified lung ultrasound score (MLUS)
- Enhancements: Includes subpleural consolidations
- Increased sensitivity: More effective in detecting early or partial lung aeration loss
3. Anterolateral protocol
- Regions scanned: 8 (anterior and lateral segments only)
- Score range: 0–24
- Use: Ideal for supine patients or when posterior scanning is impractical
These scores guide interventions such as recruitment maneuvers and PEEP titration.
Practical applications during the perioperative period
-
Intraoperative lung monitoring
LUS is used to assess aeration loss after anesthesia induction, particularly in pediatric and bariatric surgery. Studies show a strong correlation between ultrasound findings and oxygenation parameters or CT imaging.
-
PEEP titration with lung ultrasound
Step-by-step guide:
- Baseline scan: Identify regions with the worst aeration (scores 2 or 3).
- Adjust PEEP: Increase by 2–4 cm H₂O.
- Repeat scan: Wait ~5 minutes and reassess aeration.
- Determine optimal PEEP: Stop when consolidations or B-lines resolve.
PEEP titration using LUS improves oxygenation and compliance, especially in obese or laparoscopic patients.
Ultrasound-guided recruitment maneuvers
These involve stepwise increases in airway pressure, monitored with LUS until collapsed regions re-expand.
Typical parameters:
- Maximum pressure: ~40 cm H₂O
- Incremental steps: 5 cm H₂O every few breaths
Recruitment continues until dense consolidations disappear. Focus on dependent lung zones first.
Limitations to keep in mind
- LUS does not detect alveolar overdistension
- Composite scores may improve without resolving the worst-affected regions
- Operator skill significantly affects image interpretation
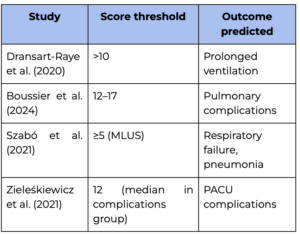
Postoperative risk assessment
Lung ultrasound is a powerful tool to predict respiratory complications post-surgery.
Key findings from clinical trials:
Pediatric applications
Lung ultrasound is equally effective in children, especially neonates and infants undergoing surgery.
Applications include:
- Surfactant need prediction in preterm neonates
- Atelectasis assessment after induction
- Guided recruitment maneuvers reducing hypoxemia
Even with fewer scanning regions, pediatric LUS protocols offer excellent diagnostic accuracy.
Future directions in lung ultrasound
- Clinical trials: Needed to validate POCUS-guided interventions
- Subpopulation protocols: Tailored for cardiac, thoracic, and pediatric surgeries
- Training programs: To reduce variability and standardize interpretation
As research grows, LUS is expected to become a mainstay in personalized ventilatory management.
Conclusion
Lung ultrasound is transforming perioperative care. With its diagnostic precision, real-time feedback, and adaptability across patient populations, LUS provides anesthesiologists with a powerful tool to optimize lung function and reduce complications. Integrating it into routine practice promises better patient outcomes and more individualized care strategies.
For more detailed information, refer to the full article in Anesthesiology.
Tanabe KJ, Fiza B, Bronshteyn YS, Fernandez-Bustamante A. Assessment of Perioperative Lung Expansion with Point-of-care Ultrasound. Anesthesiology. 2025;142(6)
Download NYSORA’s POCUS App HERE for detailed information on lung ultrasound and many more POCUS applications!