Sugammadex has revolutionized the reversal of aminosteroid neuromuscular blockade in modern anesthesia. As its use becomes widespread due to generic availability and falling costs, attention is turning to rare but serious adverse reactions, chief among them, anaphylaxis.
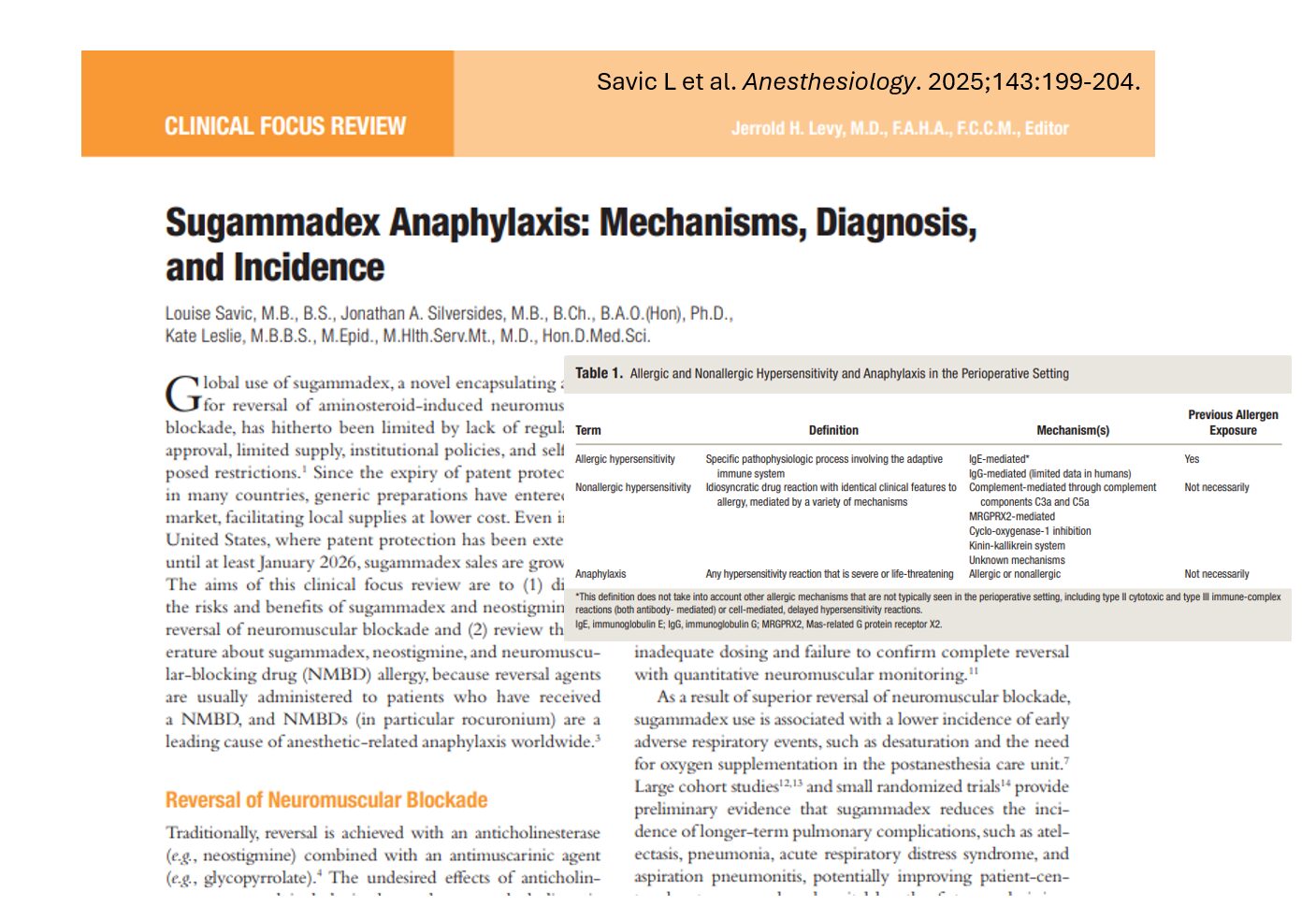
A new article by Savic et al. (2025, Anesthesiology) explores the mechanisms, diagnosis, and incidence of sugammadex-related hypersensitivity reactions, particularly in the context of its use with neuromuscular blocking drugs (NMBDs), such as rocuronium.
What is sugammadex?
Sugammadex is a modified γ-cyclodextrin designed to encapsulate aminosteroid NMBDs, effectively reversing their action. It is particularly used to reverse the effects of rocuronium and vecuronium, providing a faster and more reliable recovery from neuromuscular blockade compared to traditional agents like neostigmine.
Benefits of sugammadex over neostigmine
- Faster reversal: More rapid return of muscle function, especially for moderate and deep blocks.
- Fewer side effects: Avoids cholinergic and antimuscarinic side effects associated with neostigmine/glycopyrrolate combinations.
- Better postoperative outcomes:
- Lower rates of residual blockade
- Reduced respiratory complications like hypoxia, pneumonia, and aspiration
- Shorter hospital stays (potentially)
Key risks associated with sugammadex
While highly effective, sugammadex is not without adverse effects:
- Bradycardia: Typically mild but can be severe and even lead to asystole, especially at higher doses.
- Laryngospasm: Documented in some clinical reports.
- Anaphylaxis: A rare but potentially life-threatening event that often occurs at the end of surgery.
Allergic vs. nonallergic reactions: what’s the difference?

Immune pathways involved
- IgE-mediated allergy: Requires prior sensitization.
- Non-IgE pathways: These may involve direct mast cell activation via MRGPRX2 or complement activation, explaining reactions that occur on first exposure.
Why do patients react on first exposure?
One theory, the pholcodine hypothesis, suggests prior exposure to compounds with ammonium ions (like pholcodine in cough syrups) may sensitize individuals to NMBDs. However, such cross-reactivity is not fully understood.
For sugammadex, some hypothesize that environmental sensitization to cyclodextrins in food might play a role, though this remains unproven.
Diagnosing sugammadex allergy
In vivo testing
- Skin prick and intradermal tests:
- Helpful when pthe retest probability is high.
- Variable sensitivity/specificity.
- Can test sugammadex alone or in complex with rocuronium.
In vitro testing
- Specific IgE assays:
- Indicate sensitization, but not necessarily clinical allergy.
- Not widely available for sugammadex or NMBDs.
- Basophil and mast cell activation tests:
- Provide functional response to allergens.
- Currently experimental and not in routine clinical use.
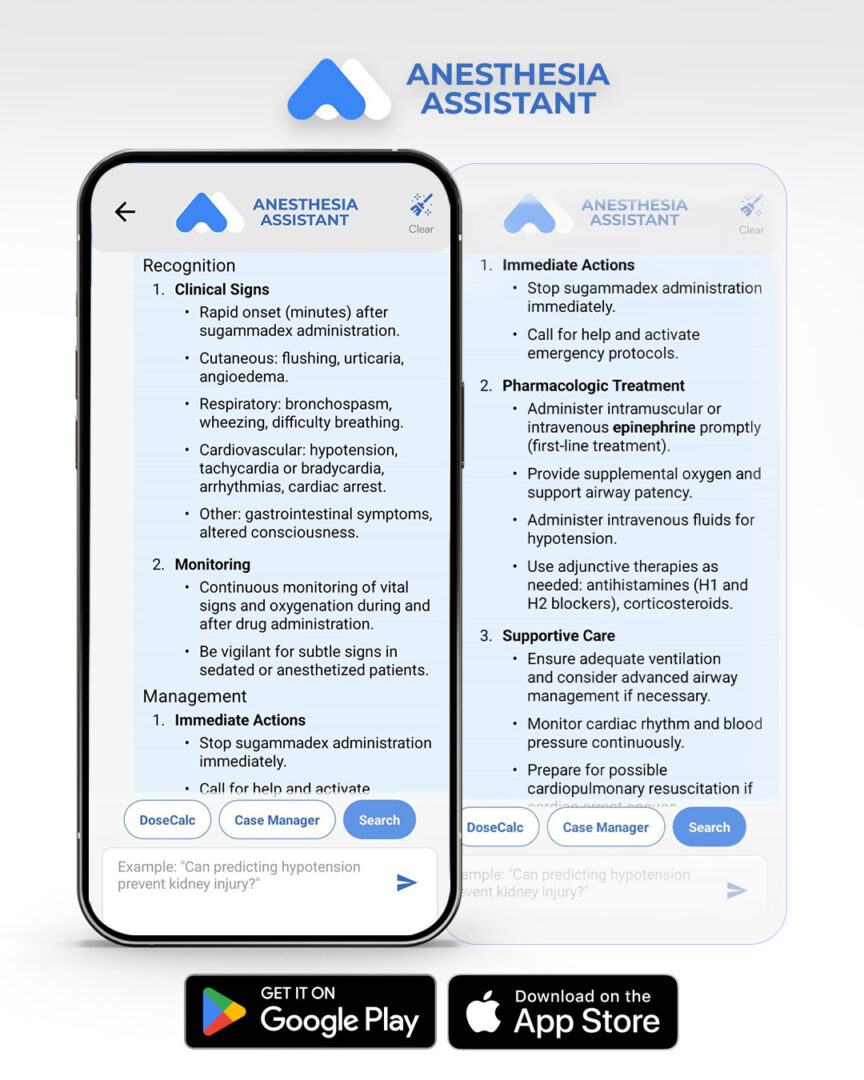
Steps to manage suspected sugammadex hypersensitivity
- Recognize symptoms: Hypotension, bronchospasm, rash, or cardiovascular collapse at the end of anesthesia.
- Administer treatment: Immediate use of epinephrine, oxygen, fluids, and antihistamines.
- Monitor: Continuous observation in a high-dependency setting.
- Refer for testing: Skin and in vitro testing as soon as the patient recovers.
- Document and report: Ensure local pharmacovigilance systems are notified.
Conclusion
Sugammadex represents a major advancement in anesthesia safety, offering faster recovery and fewer complications than older reversal agents. Though rare, the risk of hypersensitivity, particularly anaphylaxis, demands ongoing vigilance. Clinicians should be aware of diagnostic limitations, report suspected cases, and continue to support research into safer anesthesia practices.
Reference: Savic L et al. Anesthesiology. 2025;143:199-204.
For more information on sugammadex, check out Anesthesia Updates on the NYSORA Anesthesia Assistance App.
Get access to step-by-step management algorithms, the latest research, and peer-reviewed insights—all in one place. Download the app today and experience the future of anesthesia education and decision-making.
Here’s what Anesthesia Assistant recommends:
How can anaphylaxis due to sugammadex be recognized and managed?