Ambulatory surgery continues to expand across specialties as health systems push procedures out of the inpatient setting and into high-efficiency outpatient centers. This shift is driven by both economic pressure, such as hybrid DRG reimbursement models that decouple payment from hospital stay duration, and by growing evidence that well-organized outpatient programs can deliver safe, patient-centered care even for medically complex populations. Within this landscape, regional anesthesia has emerged as a critical enabler of high-quality ambulatory surgery, providing superior analgesia, lower opioid use, reduced PONV, and faster mobilization compared with general anesthesia alone.
Despite these advantages, regional anesthesia remains underutilized in many outpatient centers because of perceived workflow challenges, variability in block performance, concerns about urinary retention or transient neurological symptoms, and fear of rare complications. Limited training, especially in catheter techniques, further restricts integration. Yet modern ultrasound guidance, short-acting spinal agents, and structured recovery pathways have shown that regional anesthesia can enhance rather than slow throughput. This narrative review synthesizes experience from high-volume academic ambulatory centers in Germany and at Stanford University (collectively performing > 4000–5000 regional anesthesia cases annually), describing practical strategies to streamline workflow, optimize patient selection, integrate walking spinal and peripheral nerve block techniques, and critically assess emerging “novel” local anesthetics. The goal is clear: regional anesthesia can become a cornerstone of efficient outpatient care when embedded in a well-organized, patient-focused system.
Study objective and methods
The review aims to provide a practical, experience-based framework for implementing regional anesthesia in ambulatory surgery, with a focus on efficiency, safety, and patient satisfaction.
Design: Narrative expert review integrating published evidence, clinical guidelines, and institutional experience from two high-volume academic ambulatory centers.
Scope:
- Organizational strategies for high-throughput block workflows.
- Preoperative screening, psychological preparation, and procedure selection.
- Use of short-acting intrathecal agents, walking spinals, and peripheral nerve blocks.
- Risk mitigation strategies for PDPH, TNS, POUR, and rebound pain.
- Discharge protocols and multimodal analgesia.
- Role of continuous catheters in outpatient surgery.
- Evaluation of emerging and “novel” local anesthetics, including extended-release formulations.
Primary focus: How regional anesthesia can support, rather than impede, ambulatory surgery efficiency through deliberate workflow design, evidence-based drug selection, and standardized pathways.
Key findings
-
Efficiency depends more on organization than on anesthetic technique
A central theme of the review is that regional anesthesia does not slow ambulatory workflow when block placement is integrated into a coordinated system. Dedicated block rooms, experienced staff, standardized drug protocols, and clear communication between surgeons and anesthesiologists enable regional anesthesia to accelerate throughput by reducing PONV, improving PACU flow, and simplifying postoperative pain management. When applied systematically, regional anesthesia improves, not compromises, operating room efficiency.
-
Preoperative evaluation and psychological preparation determine block acceptance and success
The review emphasizes that successful ambulatory regional anesthesia begins before the day of surgery. Comprehensive preoperative evaluation identifies high-risk patients (OSA, cardiovascular disease, coagulopathies) and ensures outpatient eligibility. Equally important is addressing patient anxiety and misconceptions: explaining the procedure from the patient’s perspective, offering optional anxiolysis, and clarifying the level of sedation available significantly improve acceptance rates. Centers performing thousands of spinal and peripheral blocks annually report that patient-focused counseling increases acceptance to > 90%, demonstrating the substantial impact of psychological preparation on recovery and satisfaction.
-
Short-acting spinal agents make spinal anesthesia ideal for outpatient surgery
Spinal anesthesia remains a core technique in high-volume ambulatory centers. Ultra-short-acting agents such as chloroprocaine, prilocaine, and mepivacaine allow rapid onset with early recovery of motor function, facilitating same-day discharge. Chloroprocaine offers a fast onset and a 60–80-minute duration with low TNS and urinary retention risk. Prilocaine and mepivacaine allow a slightly longer duration but with predictable resolution that supports early ambulation. These agents permit spinal anesthesia even for procedures previously reserved for general anesthesia, including same-day hip and knee arthroplasty in specialized centers.
-
Walking spinal and unilateral spinal techniques can preserve mobility and reduce urinary retention
The “walking spinal” (saddle block) technique limits anesthetic spread to sacral dermatomes by administering a reduced volume of hyperbaric local anesthetic in a seated position, thereby preserving lumbar function and enabling rapid mobilization. Hypotension is rare, and discharge within 2 hours is common. Unilateral spinal anesthesia may reduce motor block and urinary retention but requires strict lateral positioning and has variable success rates. These techniques are best reserved for experienced providers who understand their nuanced dosing and positional requirements.
-
Risks such as PDPH, TNS, or POUR are low with modern needles and optimized dosing
With 27G atraumatic spinal needles, PDPH rates now fall around 2%. TNS is uncommon with bupivacaine, prilocaine, or ropivacaine and, although somewhat more frequent with mepivacaine, is generally mild and does not compromise outpatient recovery. Urinary retention—particularly problematic with long-acting hyperbaric bupivacaine—can be markedly reduced by using short-acting agents and modest doses. This allows the safe use of spinal anesthesia even in procedures historically avoided in ambulatory settings.
-
Safe same-day discharge requires structured assessment and patient education
The review underscores that discharge readiness depends on functional recovery and patient understanding, not arbitrary time thresholds. Patients must receive clear guidance on limb protection, fall prevention, and recognizing complications. Residual sensory block is acceptable if the patient demonstrates safe ambulation and has reliable home support. Written instructions and 24-hour availability of clinical support are essential for patient safety.
-
Rebound pain after single-shot blocks is predictable and must be addressed proactively
Single-injection peripheral nerve blocks provide excellent early analgesia but carry a well-documented rebound pain risk when they wear off—typically 6–12 hours postoperatively. Without proactive planning, rebound pain can undermine patient experience. The review reinforces that multimodal oral analgesia must begin before block regression, using preoperative loading, scheduled postoperative regimens, and tailored protocols for high-risk patients. Benchmarking tools like QUIPS can guide pain-management quality improvement.
-
Continuous peripheral nerve catheters provide extended analgesia but require organizational readiness
For surgeries with high pain burden (e.g., shoulder reconstruction, ACL repair), continuous nerve catheters offer superior, sustained analgesia in the outpatient environment. With portable pumps and secure catheter designs, complications are low and patient satisfaction is high. However, outpatient catheter programs require structured patient education, daily follow-up, and 24/7 support. Reimbursement and staffing remain key barriers to broader adoption.
-
Regional anesthesia expands outpatient eligibility for high-risk and complex patients
Regional techniques offer clear advantages for obese patients, those with OSA, cardiopulmonary disease, or anticoagulant therapy. Compared with general anesthesia, regional approaches minimize respiratory depression, avoid airway manipulation, and allow continuation of important medications. This makes regional anesthesia a strategic tool for expanding the safe boundaries of outpatient surgical care.
-
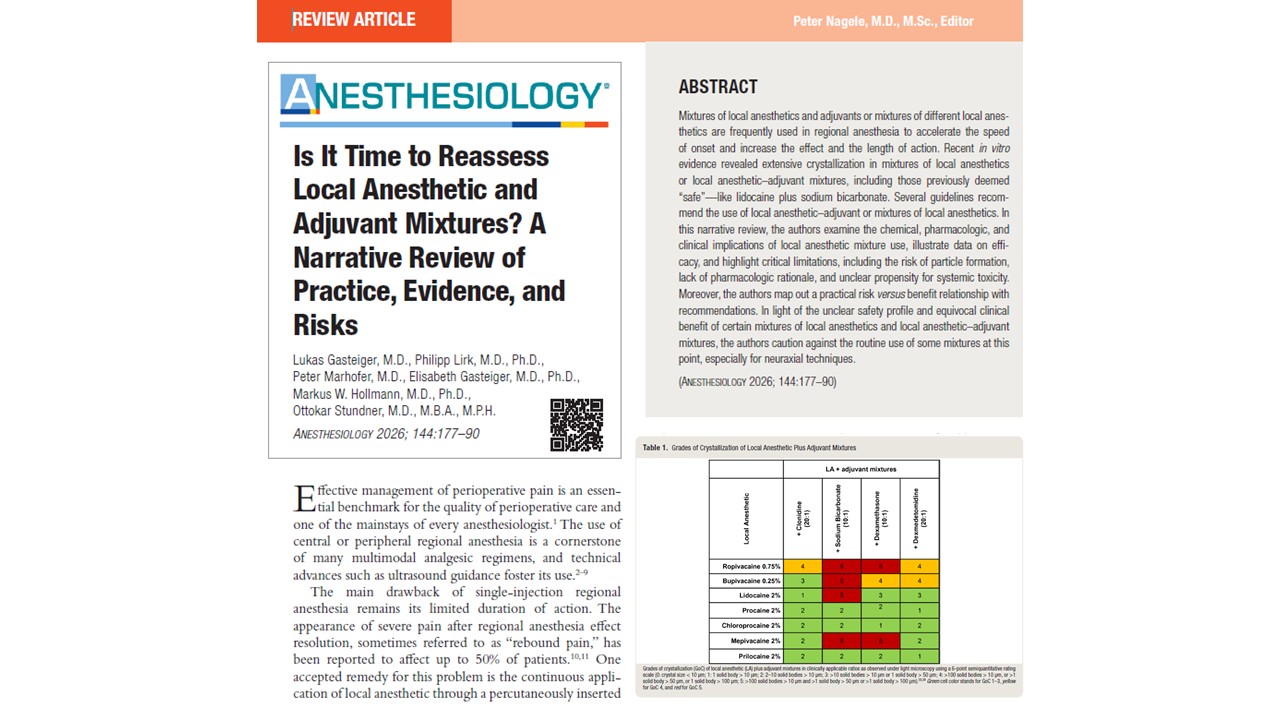
“Novel” local anesthetics remain promising but offer limited proven benefit
Extended-release formulations such as liposomal bupivacaine remain attractive for their theoretical prolonged duration, but the evidence base is inconsistent. Many trials fail to show superiority over standard bupivacaine for peripheral nerve blocks, and concerns remain regarding LAST risk if rescue blocks are needed. Other investigational agents, including polymer-bound anesthetics and C-fiber–targeting compounds, warrant further study. Overall, technique, volume, and multimodal analgesia remain more impactful than new formulations.
Conclusion
This review highlights how regional anesthesia can become a central pillar of modern ambulatory surgery when implemented within a cohesive, well-organized system. Short-acting spinal agents, optimized peripheral nerve blocks, and structured workflows support rapid recovery, early mobilization, and high patient satisfaction—even for complex or high-risk patients. Complication rates can be minimized with careful dosing and modern equipment, while proactive pain management strategies mitigate rebound effects. Although novel local anesthetics continue to emerge, current evidence supports incremental improvements rather than transformative changes. Ultimately, the success of regional anesthesia in ambulatory care depends less on any single drug or technique and more on system-level coordination, clinician expertise, and patient-centered education.
Future research
Future work should evaluate optimal spinal dosing strategies across a wider range of ambulatory procedures; define best practices for outpatient continuous catheter programs; and compare modern local anesthetic formulations in real-world settings. Research should also clarify the role of AI-supported scheduling, risk stratification tools, and novel delivery systems in enhancing safety and efficiency.
Clinical implications
Regional anesthesia offers a powerful means to improve efficiency, expand outpatient eligibility, and enhance patient experience. With thoughtful workflow integration, short-acting intrathecal agents, and reliable postoperative pathways, regional anesthesia strengthens—not slows—ambulatory surgical programs. While novel anesthetics remain under evaluation, most current gains arise from optimized systems, experienced clinicians, and clear communication with patients.
Clinical pearls
- Walking spinals with chloroprocaine or prilocaine enable rapid ambulation and discharge.
- Early psychological guidance increases block acceptance and improves outcomes.
- Begin oral analgesia before block regression to prevent rebound pain.
- Outpatient catheters work well when paired with structured education and follow-up.
Practical tip: Build your ambulatory workflow around regional anesthesia—block rooms, education, discharge protocols—rather than adding it as an afterthought.
For more detailed information, refer to the full article in Current Opinion in Anesthesiology.
Horn A. et al. Regional techniques and novel local anesthetics in ambulatory anesthesia. Curr Opin Anaesthesiol. 2025;38:728-733
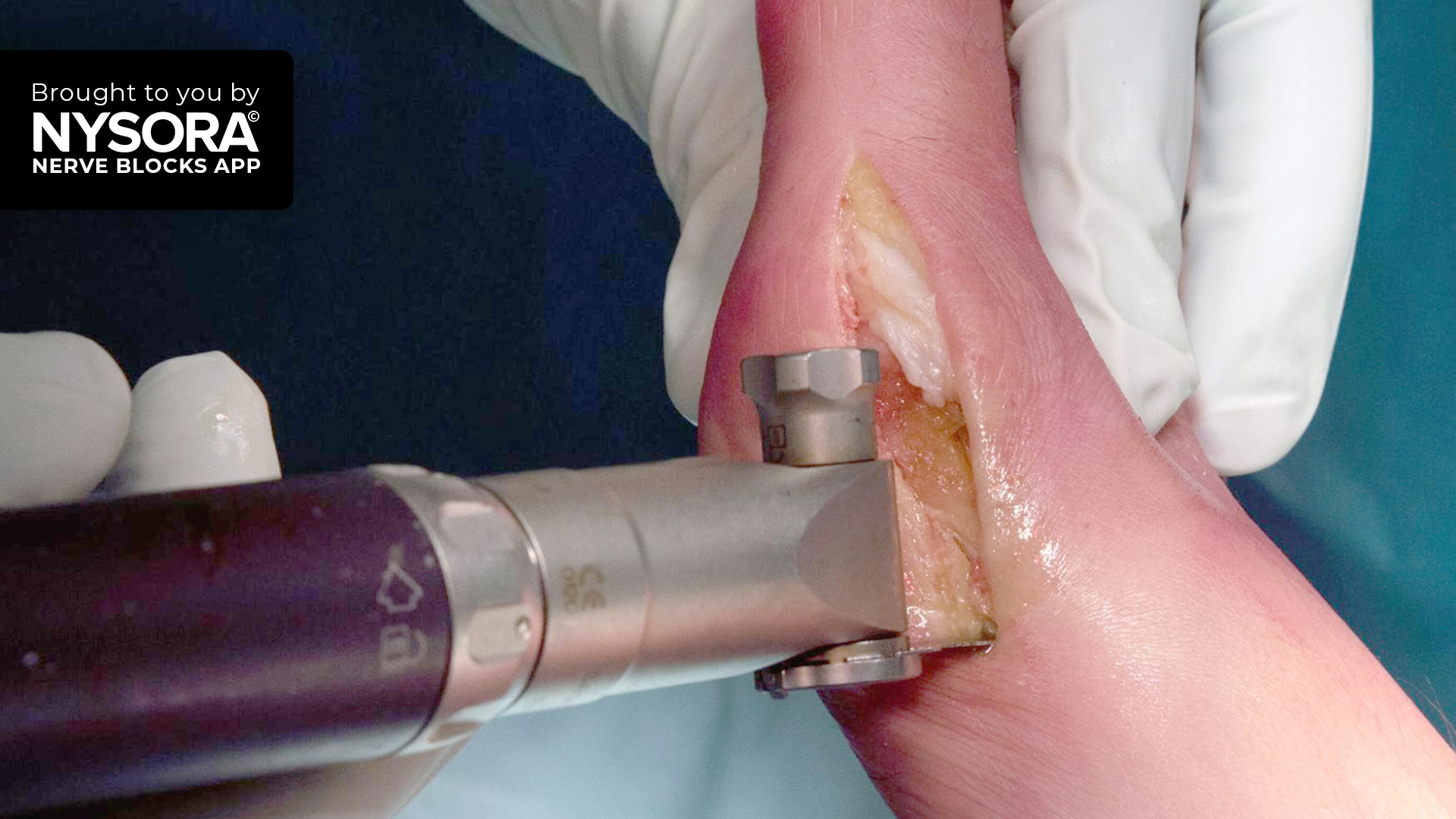
Access the full library of regional anesthesia techniques, expert videos, and clinical pearls in the NYSORA Nerve Blocks App.