Single-injection peripheral nerve blocks provide high-quality postoperative analgesia in orthopedic surgery but are limited by their duration of action. Adjuvants such as dexamethasone and dexmedetomidine – although the optimal mode of administration remains debated-have been shown to prolong brachial plexus block duration. Some clinical trials examining these adjuvants have combined medium-acting local anesthetics (LAs), such as lidocaine, with long-acting agents like bupivacaine. While adding a medium-acting LA may accelerate block onset, this practice significantly shortens the duration of both sensorimotor blockade and postoperative analgesia.
A potential solution is to use an unmixed long-acting LA together with perineural adjuvants, which may extend the duration of the block.
In a new randomized, prospective, double-blind clinical trial conducted at Hospital de San Carlos, researchers compared 0.5% bupivacaine alone to a mixture of 0.25% bupivacaine and 1% lidocaine, both combined with the perineural adjuvants dexamethasone and epinephrine, to determine whether the pure formulation would extend postoperative analgesia and sensory–motor block duration.
Study objective and methods
The randomized controlled trial’s primary hypothesis was that 0.5% bupivacaine—in the presence of perineural dexamethasone and epinephrine – would result in longer motor block duration than the bupivacaine-lidocaine mixture, albeit with a slower onset.
Study design
- Type: Randomized, prospective, double-blind controlled trial.
- Location: Hospital de San Carlos.
- Enrollment period: May – December 2023.
- Sample size: 40 patients (20 per group).
- Inclusion: Adults aged 18-80 years, ASA I–III, weight ≥ 80 kg, scheduled for forearm, wrist, or hand surgery.
- Exclusion: Inability to consent, local infection, neuropathy, coagulopathy, organ failure, allergy to local anesthetics, pregnancy, prior infraclavicular surgery, or chronic opioid use.
- Randomization and blinding: A research assistant generated a computer-based randomization list and prepared sealed opaque envelopes. Both patients and clinicians assessing outcomes were blinded to group allocation.
Interventions
- Group B: 35 mL of 0.5% bupivacaine + epinephrine (5 µg/mL) + dexamethasone (4 mg).
- Group BL: 35 mL of 0.25% bupivacaine + 1% lidocaine + same adjuvants.
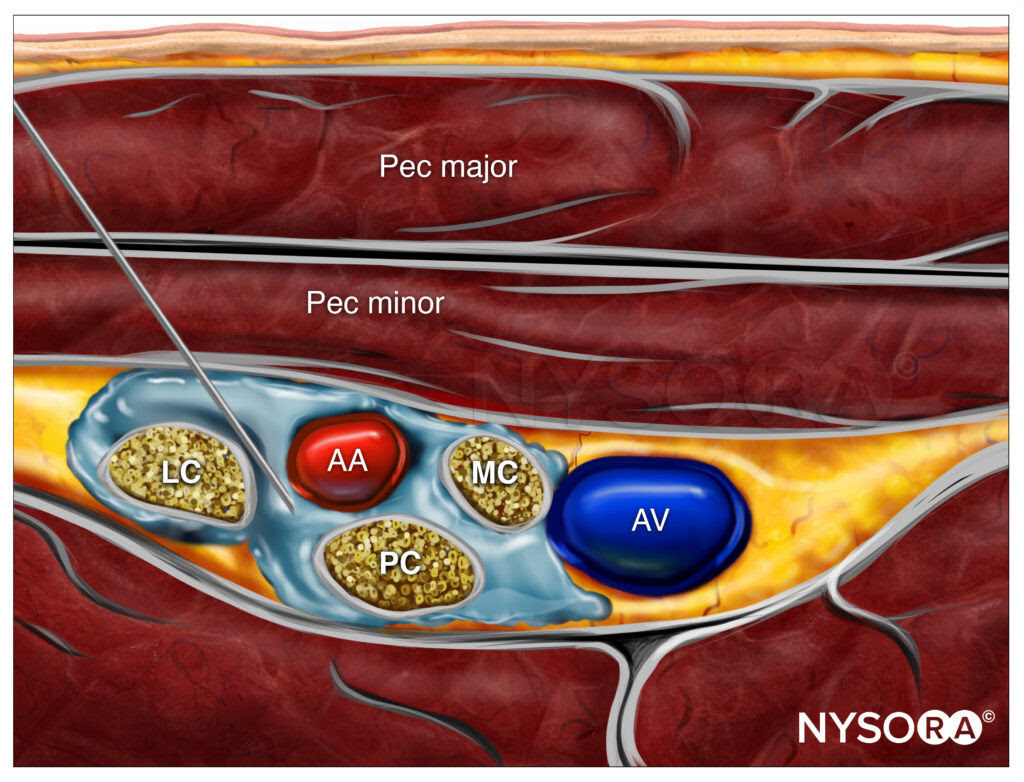
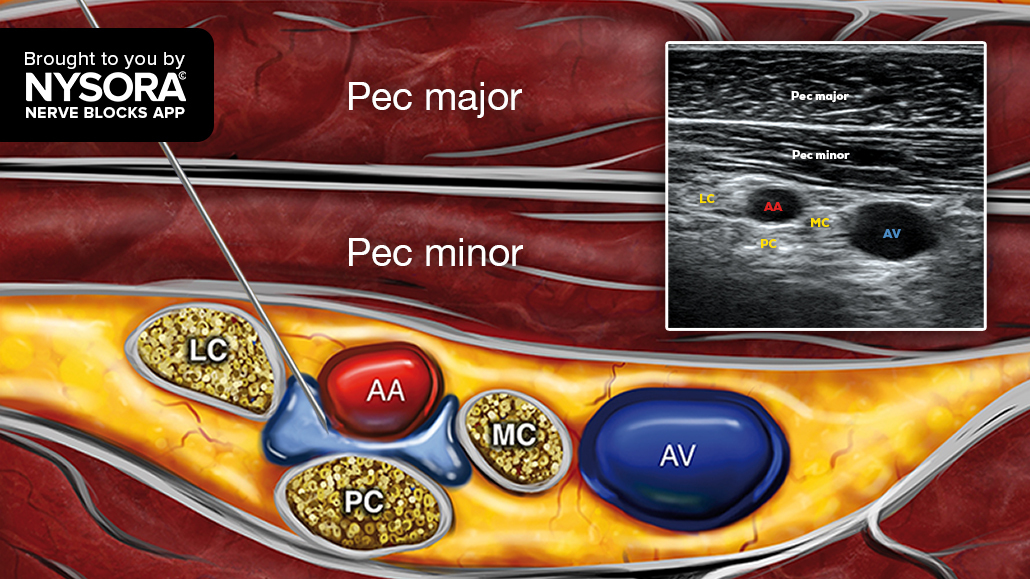
All blocks were performed by a single experienced anesthesiologist using ultrasound guidance and a standardized infraclavicular approach, placing the needle dorsal to the axillary artery for local anesthetic deposition.
Outcomes
- Primary: Duration of motor block (patient-reported).
- Secondary: Sensory block duration, postoperative analgesia duration, onset time, block success, surgical anesthesia rates, rebound pain, and adverse events.
Patients recorded the times when motor and sensory function returned and when pain first occurred. Follow-up was conducted at 24, 48, and 72 hours, with a 7-day check for complications.
Key findings
-
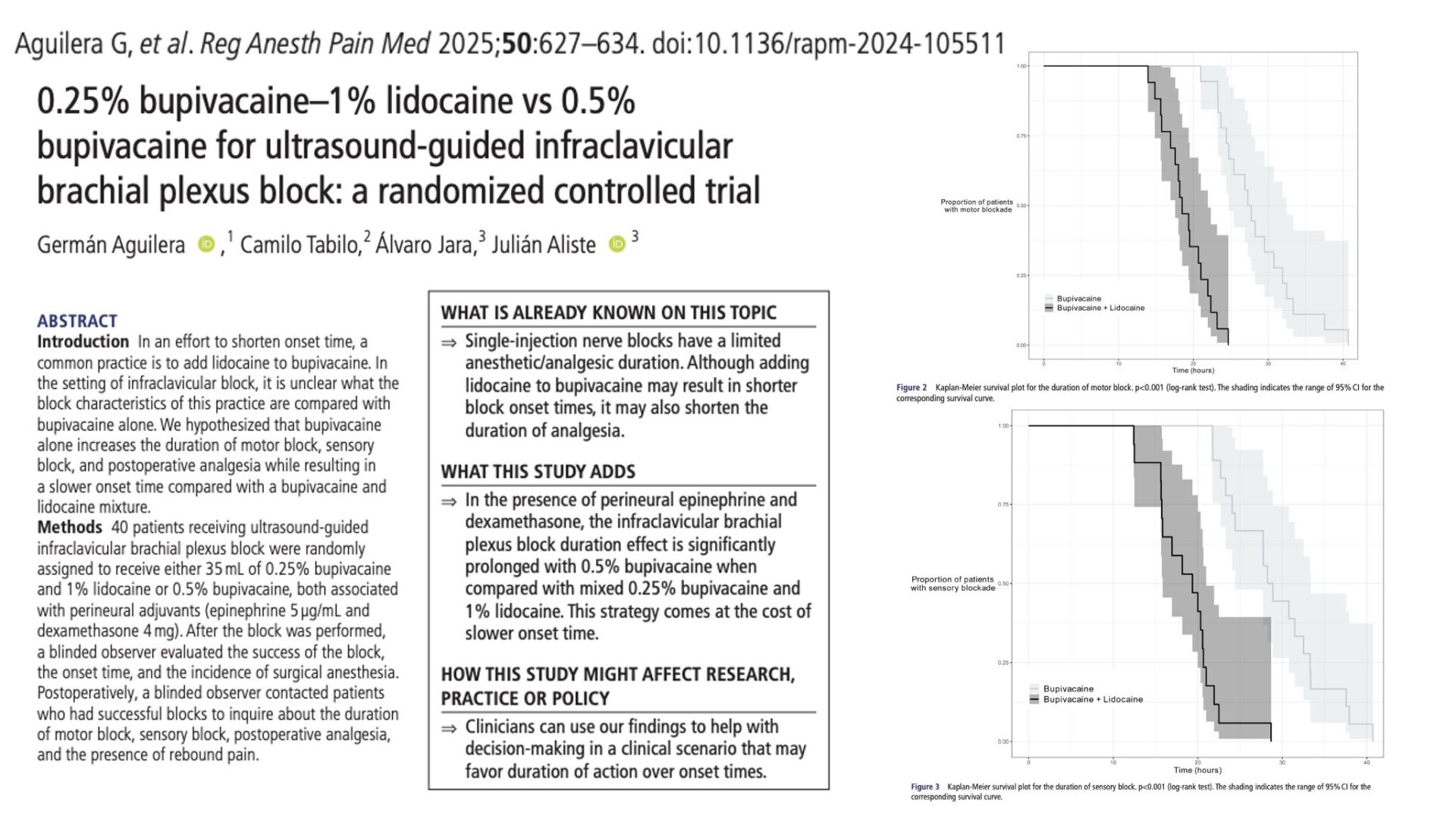
Primary outcome: Motor block duration
- Bupivacaine alone: 28.4 ± 5.2 hours.
- Bupivacaine-lidocaine mixture: 18.9 ± 3.1 hours.
- Mean difference: + 9.5 hours (95% CI 6.5–12.4; p < 0.001).
Pure bupivacaine extended motor block by approximately 50% compared to the mixture.
-
Secondary outcomes
- Sensory block duration:
- Bupivacaine: 29.3 ± 5.8 hours.
- Mixture: 18.7 ± 4.0 hours.
- Difference: + 10.6 hours (p < 0.001).
- Postoperative analgesia duration:
- Bupivacaine: 38.3 ± 7.4 hours.
- Mixture: 24.3 ± 6.6 hours.
- Difference: + 14 hours (p < 0.001).
- Onset time:
- Bupivacaine: median 35 minutes.
- Mixture: median 20 minutes.
- p < 0.001 (faster onset in the mixture group).
- Block success rates: Comparable between groups; almost all patients achieved surgical anesthesia without supplemental blocks.
- Rebound pain incidence:
- Bupivacaine: 11.1%.
- Mixture: 31.6%.
- Difference not statistically significant (p = 0.23), but numerically lower in pure bupivacaine group.
-
Safety
- No significant differences in vascular puncture, hematoma, systemic local anesthetic toxicity, paresthesia, or Horner syndrome.
- Two patients experienced temporary paresthesia lasting up to 3 months, both resolving without intervention.
Discussion
This study clearly demonstrates that 0.5% bupivacaine, when combined with dexamethasone and epinephrine, significantly prolongs sensory and motor block duration and extends postoperative analgesia compared to a bupivacaine-lidocaine mixture in infraclavicular blocks.
The trade-off is a slower onset time – a median delay of 15 minutes compared to the mixture. This means that pure bupivacaine may be best suited for situations where a rapid onset is not critical, such as when blocks are performed in a preoperative block room or when general anesthesia is used for surgery and the nerve block is intended for postoperative pain control.
Pharmacologically, bupivacaine’s higher lipophilicity and protein binding result in slower clearance from nerve tissues, prolonging block duration. Mixing with lidocaine dilutes this concentration, reducing the depot effect and shortening the block’s lifespan.
Conclusion
In ultrasound-guided infraclavicular brachial plexus block for upper limb surgery, pure 0.5% bupivacaine with perineural dexamethasone and epinephrine provides the longest sensorimotor block and postoperative analgesia reported for a single-shot technique in this setting. While it delays onset, its extended duration makes it a valuable option for optimizing postoperative pain control and potentially reducing opioid use in the first 48 hours after surgery.
Future research
The authors suggest further trials to:
- Evaluate different concentrations of bupivacaine and other long-acting agents (e.g., ropivacaine, levobupivacaine).
- Compare intravenous vs perineural administration of adjuvants with pure bupivacaine.
- Assess functional recovery timelines when using prolonged motor block strategies.
- Study outcomes in supraclavicular, interscalene, and axillary brachial plexus approaches.
Clinical implications
For surgical cases where long-lasting analgesia is a priority – such as fracture fixation or procedures with significant postoperative pain-pure bupivacaine with adjuvants may reduce the need for perineural catheters or repeated blocks.
Conversely, for short cases or when a fast onset is critical, such as urgent trauma surgery under regional anesthesia alone, a mixture may be preferred.
Additionally, the lower incidence of rebound pain observed with pure bupivacaine, while not statistically significant, is consistent with prior findings that longer-lasting blocks may soften the transition to normal sensation and mitigate pain spikes.
Clinical pearls
- 0.5% bupivacaine extended motor block by ~50% vs. mixture (28.4 vs. 18.9 h).
- Sensory block and analgesia durations were also longer (29.3 vs 18.7 h; 38.3 vs. 24.3 h).
- Trade-off: Slower onset (35 vs. 20 min).
- Lower (non-significant) incidence of rebound pain with pure bupivacaine.
Practical tip: Use 0.5% bupivacaine for long, painful upper limb surgeries where duration matters more than rapid onset. Reserve mixtures for urgent cases.
For more detailed information, refer to the full article in RAPM.
Aguilera G. et al. 0.25% bupivacaine-1% lidocaine vs 0.5% bupivacaine for ultrasound-guided infraclavicular brachial plexus block: a randomized controlled trial. Reg Anesth Pain Med. 2025;50:627-634.
Download the Nerve Blocks App HERE for in-depth insights on the infraclavicular brachial plexus block. Prefer a physical copy? The bestselling NYSORA Nerve Blocks App is available in book format – an essential resource for mastering nerve blocks! And for a digital learning experience, check out the Nerve Blocks Manual Module on NYSORA360!