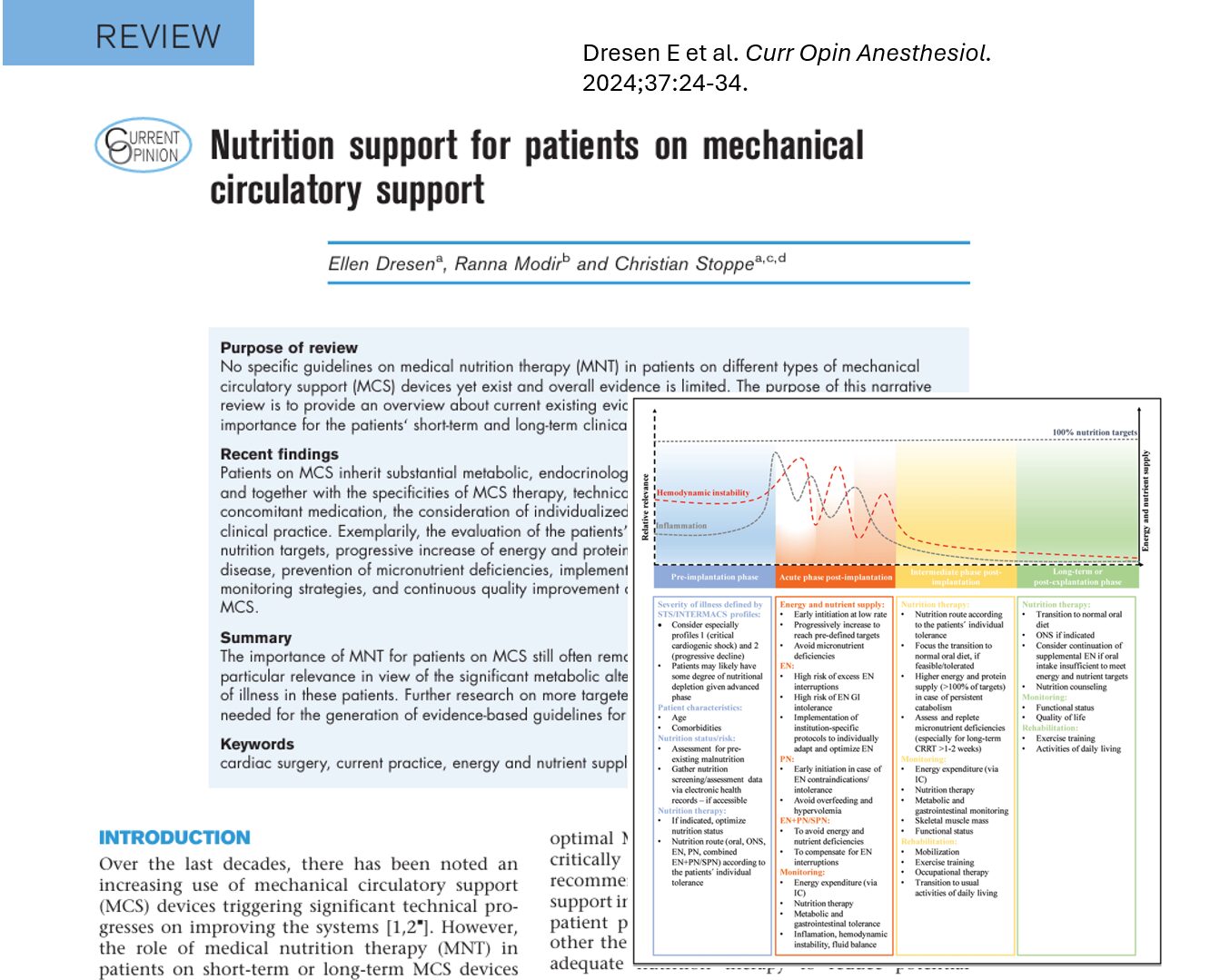
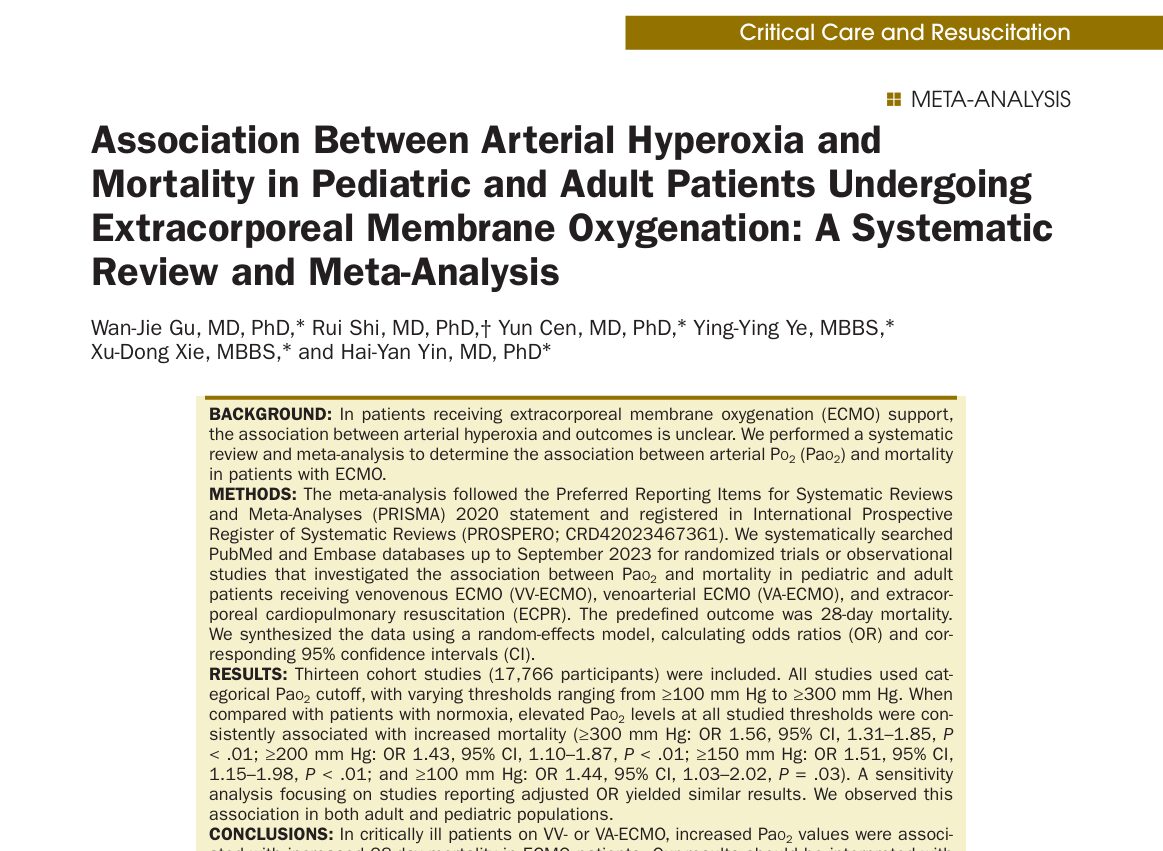
As the use of mechanical circulatory support (MCS) devices like ECMO and VADs increases, critical care teams face an ongoing challenge: delivering safe, effective nutrition to these highly complex patients. A review by Dresen et al. (2024) in Current Opinion in Anaesthesiology synthesizes the latest findings on nutrition in MCS patients, offering insights that could help reduce complications and improve recovery.
Why nutrition matters in MCS
Patients on MCS are at risk for catabolic stress, muscle wasting, and malnutrition, all of which worsen outcomes and prolong ICU stays. However, nutrition therapy in this population remains underexplored due to:
- Complex device-patient interactions
- Frequent multi-organ failure
- Hemodynamic instability
- High risk of gastrointestinal (GI) complications
Key takeaways from the 2024 review
Early nutrition is feasible and safe
- Enteral nutrition (EN) can be initiated within 24–48 hours after MCS initiation if the patient is hemodynamically stable.
- Trophic feeds (10–20 kcal/h) are recommended to start, progressing as tolerated.
Hypocaloric feeding preferred early
- Avoid overfeeding during the early inflammatory phase.
- Aim for hypocaloric, high-protein regimens to preserve lean body mass while minimizing complications.
Monitoring and adaptations are crucial
- Frequent assessment of gastric residuals, abdominal pressures, and GI tolerance is essential.
- Indirect calorimetry, if available, helps fine-tune energy requirements.
Step-by-step approach to nutrition in MCS
-
Initial assessment
- Check for contraindications: uncontrolled shock, active GI bleeding, high vasopressor requirements
- Start indirect calorimetry if available
-
Early trophic feeding
- Begin with 10–20 kcal/h enterally if stable
- Use continuous infusion to improve tolerance
-
Monitor and adjust
- Evaluate gastric residuals every 4–6 hours
- Consider abdominal pressure monitoring in high-risk patients
- Increase calories gradually to meet 60–70% of goal by day 4–5
-
Parenteral support (if needed)
- Start supplemental PN if enteral route is not tolerated by day 5–7
- Avoid early full-calorie PN due to risk of overfeeding and infection
Special considerations by device type

Nutritional targets: not one-size-fits-all
- Protein: 1.3–2.0 g/kg/day (adjusted for actual vs. ideal weight)
- Energy: Gradual progression from 20 kcal/kg/day to ~25–30 kcal/kg/day
- Micronutrients: Thiamine, selenium, and vitamin D are often deficient in critically ill patients
What’s missing? The evidence gap
Despite its importance, nutrition in MCS remains under-studied. The review emphasizes:
- A lack of high-quality RCTs
- Limited device-specific protocols
- Need for individualized feeding strategies based on perfusion, inflammation, and recovery trajectory
Practical tips for ICU teams
- Start small: trophic feeds are better than none
- Monitor continuously, not just daily
- Communicate closely with pharmacists, dietitians, and the MCS team
- Document tolerance and nutritional adequacy daily
For more detailed information, refer to the full article in Current Opinion in Anesthesiology.
Dresen E et al. Nutrition support for patients on mechanical circulatory support: Current practice and future directions. Curr Opin Anesthesiol. 2024;37:24-34.
Read more about this topic in NYSORA’s Anesthesia Updates.