As global health systems increasingly grapple with their environmental impact, the operating room has emerged as a key area for sustainable reform. One of the largest contributors to hospital emissions is the administration of general anesthesia (GA). A new study published in the British Journal of Anaesthesia (2025) by Bernat et al. provides critical new evidence on how different anesthetic techniques compare in terms of greenhouse gas (GHG) emissions and overall ecological footprint.
Why this study matters
Healthcare globally is responsible for a substantial proportion of GHG emissions. If it were a country, the healthcare sector would be the fifth-largest emitter in the world. Operating rooms are especially resource-intensive, with anesthetic gases accounting for up to 40% of surgical emissions.
This study by Bernat et al. stands out due to its real-world, multicentre scope, analyzing over 35,000 adult surgeries across three major French hospitals. It’s the most comprehensive comparison to date of:
- Total intravenous anesthesia (TIVA) using propofol
- Target-controlled inhalation anesthesia (TCIA) using sevoflurane
- Manually optimised sevoflurane anesthesia
Overview of anesthetic techniques
1. Total intravenous anesthesia (TIVA)
- Administered exclusively via IV using propofol
- Avoids the use of volatile gases
2. Target-controlled inhalation anesthesia (TCIA)
- Uses automated systems to deliver sevoflurane at ultra-low fresh gas flows (~0.5–0.8 L/min)
3. Manually optimised sevoflurane
- Inhalation anesthesia is managed manually by anesthetists using protocols to minimize gas waste
Key findings: GHG emissions per hour
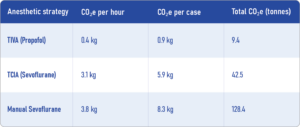
These results show that TIVA with propofol produces 8 to 10 times fewer carbon emissions per hour than either form of sevoflurane-based inhalation anesthesia.
Environmental impacts beyond carbon emissions
While CO₂ emissions are the main metric, other pollutants were considered:
Plastic waste per procedure
- TIVA: 72 g
- TCIA: 18 g
- Manual Sevoflurane: 27 g
Aluminium waste per procedure
- Only in strategies using sevoflurane in aluminium bottles (TIVA group): 0.09 g
Electrical consumption (syringe pumps for TIVA)
- Marginal, contributing 0.1 tonnes CO₂e across all procedures
Despite the low CO₂e, TIVA leads to more plastic waste, primarily from disposable syringes and propofol containers.
Step-by-step guide to greener anesthesia
- Eliminate desflurane and nitrous oxide from anesthetic protocols.
- Adopt TIVA wherever clinically appropriate.
- Use TCIA systems for cases that require inhalation anesthesia.
- Educate clinicians on low-flow techniques and eco-friendly practices.
- Manage waste responsibly, especially propofol disposal and plastic recycling.
- Monitor anesthetic usage via software-integrated machines.
Evidence for clinical equivalence or superiority
In addition to environmental advantages, TIVA has shown:
- Faster recovery times
- Reduced postoperative nausea/vomiting
- Fewer delirium episodes in elderly and cancer surgery patients
- Comparable or better quality of recovery scores
These findings help support a shift towards TIVA from both ecological and patient-care perspectives.
The global context
Currently, over 75% of surgeries worldwide rely on inhaled anesthesia. A full shift to TIVA isn’t feasible immediately. Instead, a dual strategy is recommended:
- Promote TIVA for routine surgeries
- Implement TCIA or low-flow sevoflurane for complex or long procedures
Even without full adoption, phasing out desflurane and N₂O, along with training providers in sustainable practices, could reduce anesthetic GHG emissions by up to 98%.
Final thoughts
This study adds robust, real-world evidence to a growing body of research advocating for greener anesthesia. TIVA, when feasible, should be the preferred method to reduce the carbon footprint of surgical care.
However, sustainability is not just about emissions; it’s about striking a balance between patient safety, waste management, and resource availability. The future of anesthesia will likely depend on smarter integration of automated systems, sustainable materials, and clinician training.
Reference: Bernat M. et al. The carbon footprint of general anaesthesia in adult patients: a multicentre observational comparison of intravenous and inhalation anaesthetic strategies in 35,242 procedures. British Journal of Anaesthesia;134:1620-1627.
For more information on anesthetic techniques and their impact on the environment, check out Anesthesia Updates on the NYSORA Anesthesia Manual App.
Get access to step-by-step management algorithms, the latest research, and peer-reviewed insights—all in one place. Download the app today and experience the future of anesthesia education and decision-making.
AI On Call: Case of the Week
How does your choice of anesthetic technique affect the environment?