Direct oral anticoagulants (DOACs) have transformed anticoagulation therapy, offering safer and more convenient alternatives to traditional agents like warfarin. However, managing DOACs around high bleeding risk procedures such as neuraxial anesthesia and deep peripheral nerve blocks remains a complex clinical challenge.
This post explores the latest 2025 evidence and guidance from the American Society of Regional Anesthesia and Pain Management (ASRA) and the evolving Perioperative Anticoagulant Use for Surgery Evaluation (PAUSE) protocol.
Why is DOAC management critical in regional anesthesia?
DOACs are widely prescribed for conditions like atrial fibrillation and venous thromboembolism. Approximately 10–15% of DOAC-treated patients will undergo procedures that require temporary cessation of anticoagulation.
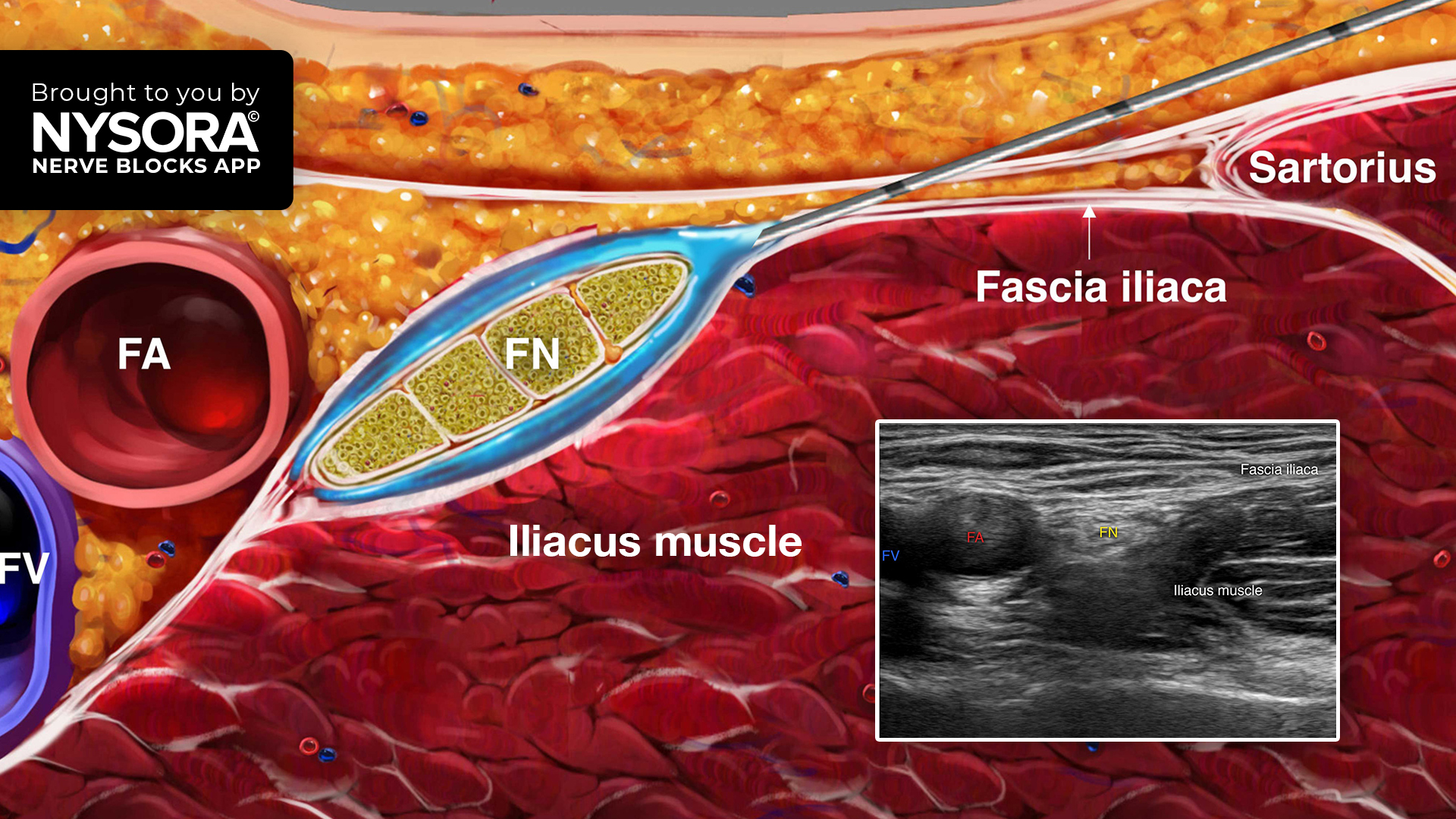
Neuraxial anesthesia and deep peripheral nerve blocks are increasingly used, with benefits such as:
- Improved pulmonary outcomes
- Enhanced bowel function
- Opioid-sparing effects
Yet these benefits must be balanced against the risk of bleeding complications, including the rare but severe spinal epidural hematoma.
Understanding the risks
What is spinal epidural hematoma?
A spinal epidural hematoma is a rare complication of neuraxial anesthesia that can lead to permanent neurological damage. Risk factors include:
- Advanced age
- Renal dysfunction
- Coagulopathies
- Use of anticoagulants like DOACs
Estimated risk:
- Lumbar: 7.5 per 10,000 procedures
- Thoracic: up to 3.6 per 10,000 procedures
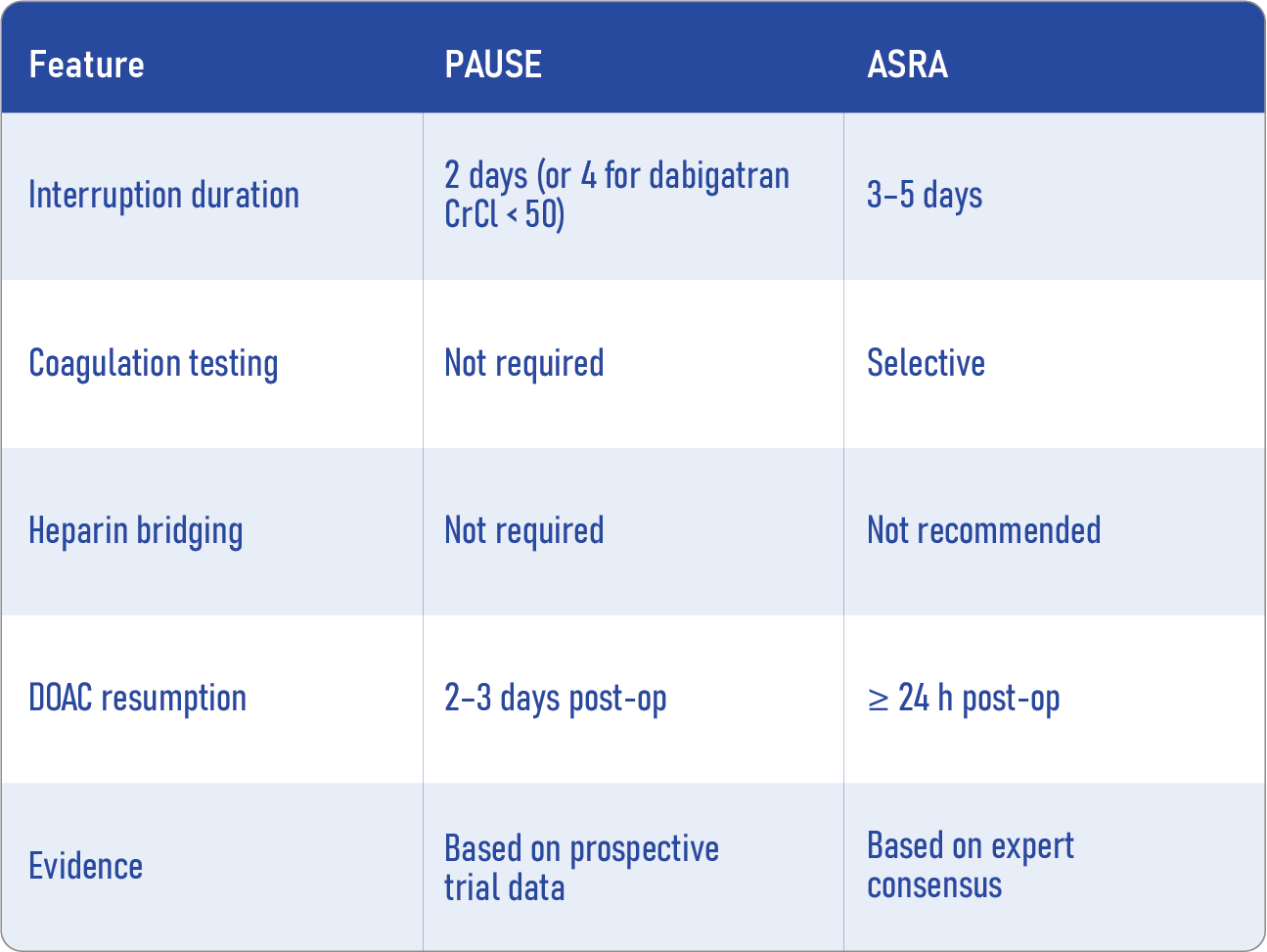
Comparing the ASRA guidelines vs. the PAUSE protocol
ASRA guidelines (2025 update)
- DOAC interruption: 72 hours minimum before neuraxial or deep nerve block procedures
- Dabigatran with CrCl < 50 mL/min: 120-hour interruption
- Resumption: Minimum 24 hours after needle removal
- Testing: DOAC level testing recommended (<30 ng/mL) if interruption is shorter or in special populations (elderly, obese, renal dysfunction)
- Heparin bridging: No longer recommended
PAUSE protocol
- Standardised approach based on bleeding risk and DOAC pharmacokinetics
- DOAC interruption: 2 days (60–68 hours), 4 days for dabigatran with CrCl <50 mL/min
- Resumption: 2–3 days post-procedure
- Testing: Not required
- Major bleeding rates: ~3% for high-risk procedures
Key differences at a glance
Step-by-step: managing DOACs for neuraxial procedures
- Assess bleeding and thromboembolic risk.
- Evaluate renal function, especially for dabigatran.
- Choose interruption protocol: ASRA (conservative) or PAUSE (standardised).
- Discontinue DOACs according to protocol (see table below).
- Consider DOAC level testing for high-risk patients (ASRA).
- Perform the procedure once the anticoagulant effect is minimal.
- Delay resumption by 2–3 days to reduce bleeding risk.
When to consider ASRA over PAUSE
- Patients at extremely high risk for spinal epidural hematoma
- Those with comorbidities such as severe renal disease, spinal abnormalities
- Elective procedures where extra caution is warranted
The PAUSE-2 pilot: what did we learn?
The PAUSE-2 pilot trial randomized DOAC-treated patients undergoing high bleeding risk procedures, including neuraxial anesthesia. Key takeaways:
- DOAC levels < 30 ng/mLwere achieved in ~95% of both ASRA and PAUSE groups
- PAUSE shortened DOAC interruption by ~25% without compromising safety markers
- No significant increase in bleeding risk was observed.
- The trial was underpowered to detect rare events like spinal hematoma
Looking ahead: PAUSE-2 trial
The full-scale PAUSE-2 trial will directly compare ASRA and PAUSE strategies for neuraxial procedures. It aims to determine:
- Whether shorter DOAC interruptions are safe
- If more patients can benefit from neuraxial anesthesia
- Whether routine DOAC testing can be eliminated without increasing risk
- This landmark study could influence future guidelines and expand access to safer regional anesthesia for anticoagulated patients.
Conclusion
Managing DOACs in the context of neuraxial anesthesia and deep nerve blocks demands a careful balance between bleeding and thrombotic risks. While ASRA offers a cautious, time-tested approach, the PAUSE protocol introduces a more pragmatic strategy grounded in pharmacokinetics.
Until larger trials like PAUSE-2 provide definitive answers, clinicians must individualise decisions based on:
- Patient comorbidities
- Renal function
- Procedure risk
- Institutional capabilities
The future of DOAC management lies in safer, evidence-based protocols that preserve both anticoagulant protection and procedural safety.
Reference: Suleiman A et al. Direct oral anticoagulant management for neuraxial anaesthesia and deep peripheral nerve blocks. Br J Anaesth. 2025;135:1603-1608
Download the AA App now to put trusted anesthesia guidance in your pocket.