In a landmark randomized clinical trial published in the November 2025 issue of Anesthesia & Analgesia, researchers showed that high-flow nasal oxygen (HFNO) is a viable and safe alternative to mechanical ventilation via a laryngeal mask airway (LMA) during short general anesthesia without muscle paralysis.
This study focused on a critical question: Can HFNO, a less invasive method of respiratory support, match the effectiveness and safety of LMA ventilation in the operating room? The answer, backed by rigorous data, is a resounding yes, with a few caveats.
Study highlights at a glance
- Trial design: Single-center, randomized, noninferiority study
- Sample: 180 female patients undergoing elective operative hysteroscopy
- Duration: Conducted from May 2022 to June 2023
- Primary outcome: Intraoperative respiratory support success
- Key finding: HFNO was noninferior to LMA ventilation, with a 99% success rate in both groups
What is high-flow nasal oxygen (HFNO)?
HFNO delivers heated, humidified oxygen-enriched air through specialized nasal cannulae at high flow rates (up to 70 L/min). Originally developed for intensive care, HFNO has gained popularity in anesthesia and perioperative medicine due to its simplicity and potential for reducing complications associated with invasive airway devices.
Research methods
Patient criteria
- Inclusion: ASA physical status I–II, < 70 years, undergoing elective hysteroscopy
- Exclusion: BMI > 30, OSAS, COPD, complex or long surgeries (> 60 min), cardiac/neuromuscular diseases
Randomization and procedure
Participants were randomized 1:1 into two groups:
- HFNO group
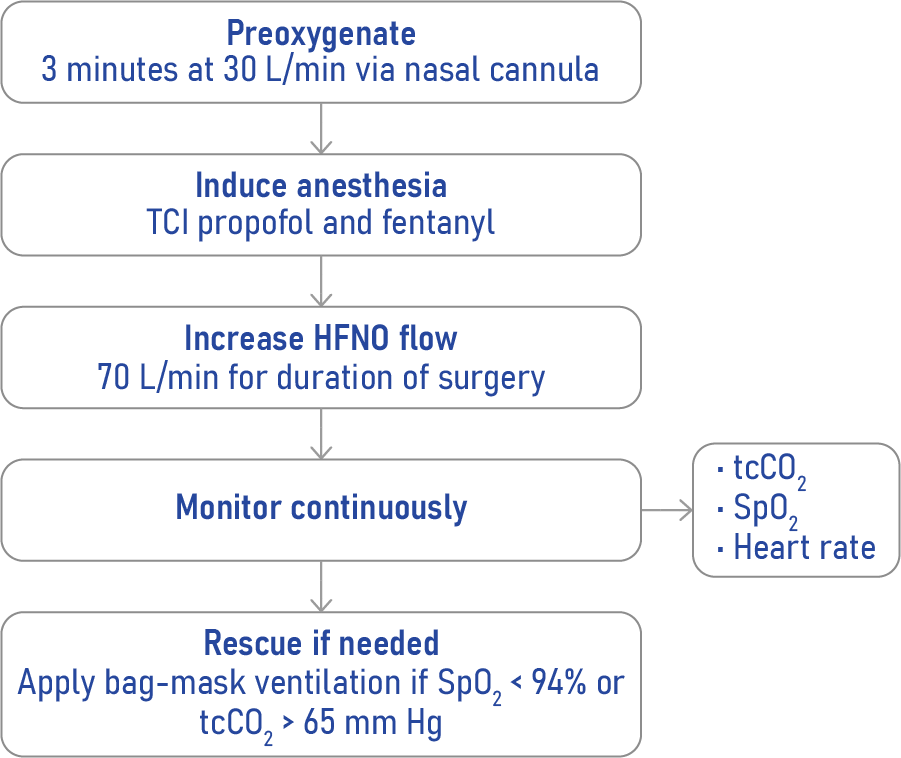
- Preoxygenation: 100% oxygen at 30 L/min for 3 minutes
- Maintenance: 70 L/min of 100% oxygen throughout surgery
- LMA group
- Preoxygenation via facial mask at 15 L/min
- Ventilation via I-Gel LMA using volume-controlled mechanical ventilation
Anesthesia protocol
- Induction with target-controlled infusion (TCI) of propofol and fentanyl
- No neuromuscular blockade used
- Monitoring: Spo2, transcutaneous CO2 (tcCO2), heart rate, and blood pressure
Primary and secondary outcomes
Respiratory support success (Primary outcome)
- Defined as Spo2 ≥ 94%, tcCO2 < 65 mm Hg, and no need for rescue airway interventions
- Success rate: 99% in both HFNO and LMA groups
Postoperative respiratory symptoms (Secondary outcomes)
- HFNO group: 2% experienced mild symptoms
- LMA group: 21% had symptoms such as sore throat and discomfort
Airway complications and postoperative dyspnea
- Low and comparable between groups
- 1 patient in each group required rescue intervention
Advantages of HFNO over LMA
- Less invasive: No insertion of airway devices into the pharynx
- Lower risk of trauma: Avoids complications like sore throat, laryngeal injury, or vocal cord damage
- Faster recovery: Shorter anesthesia duration and quicker postoperative arousal
- Simplified workflow: Easier setup and fewer manual interventions
Risks and considerations with HFNO
While HFNO maintained adequate oxygenation, the tcCO2 levels were significantly higher than those in the LMA group:
- Average tcCO2 during surgery: 42 mm Hg (HFNO) vs 36 mm Hg (LMA)
- Peak tcCO2: Up to 65 mm Hg in some HFNO patients
- Implication: Risk of hypercarbia, a condition where carbon dioxide builds up in the bloodstream
This underscores the need for close patient monitoring and careful patient selection, particularly avoiding use in patients with CO2 retention risk.
Step-by-step guide: how HFNO was implemented
Clinical implications
- Noninferiority confirmed: HFNO is a valid alternative to LMA for procedures under 30 minutes
- Better patient comfort: Lower incidence of throat and airway irritation
- Need for monitoring: Continuous CO2 monitoring is critical to detect hypercarbia
- Expansion potential: Could be used for other short surgeries with proper safeguards
Final thoughts
This trial adds robust clinical evidence supporting HFNO as a noninvasive, efficient, and patient-friendly alternative to traditional mechanical ventilation for short surgeries under general anesthesia without neuromuscular blockade. As the medical community continues to seek safer and more comfortable anesthesia techniques, HFNO is poised to play an increasingly central role—provided that its use is individualized and carefully monitored.
Reference: Frassanito L et al. High-Flow Nasal Oxygen versus Mechanical Ventilation Through a Laryngeal Mask During General Anesthesia Without Muscle Paralysis: A Randomized Clinical Trial. Anesth Analg. 2025;141:1116-1125.
Read more about this topic in the Anesthesia Updates section of the Anesthesia Assistant App.