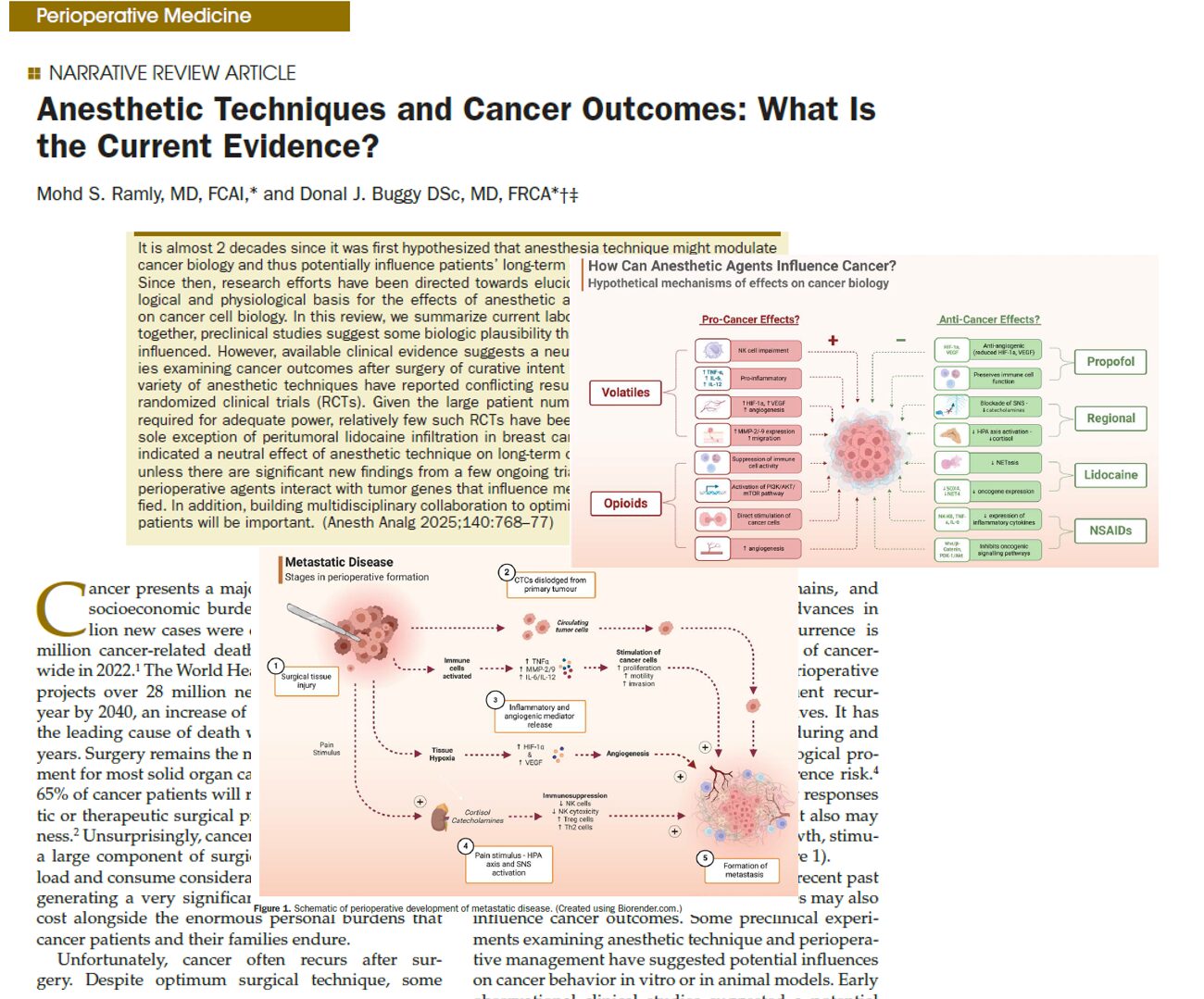
In the ever-evolving landscape of cancer care, the role of anesthesia during cancer surgery has garnered significant scientific attention. Could the choice of anesthetic technique influence cancer recurrence and survival rates? A 2025 review by Dr. Mohd S. Ramly and Dr. Donal J. Buggy offers the latest insights into this critical question.
Scientific background
The “seed and soil” hypothesis, dating back to 1889, remains central: cancer cells (“seed”) metastasize if the body’s environment (“soil”) is receptive. Surgery can inadvertently promote cancer spread through:
- Stress-induced immune suppression
- Inflammatory responses stimulate residual tumor growth
- Formation of supportive metastatic niches
Anesthetic agents could influence these biological processes by modulating immunity, inflammation, and cellular signaling.
Anesthetic methods studied
1. Propofol total intravenous anesthesia (TIVA) vs. volatile anesthesia
Laboratory findings:
- Propofol reduces angiogenesis and inflammation.
- Volatile agents like sevoflurane may promote cancer cell proliferation via hypoxia pathways.
Clinical findings:
- Large trials in breast, gastrointestinal, and colorectal cancers show no significant difference in cancer recurrence or survival between propofol and volatile anesthesia.
- Ongoing studies like GA-CARES continue to explore this question.
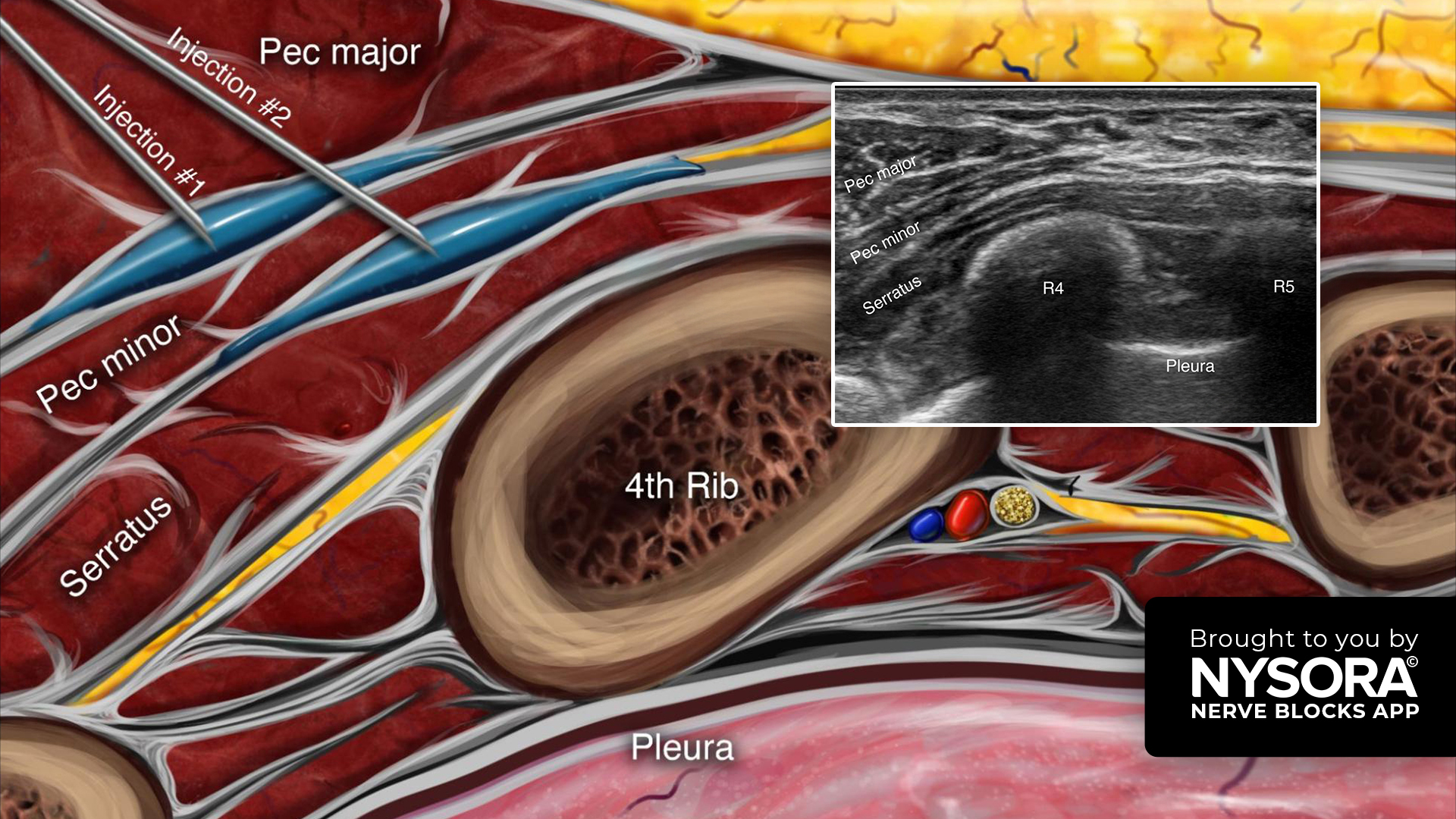
2. Regional anesthesia and neuraxial blocks
Hypothesized benefits:
- Blunting the surgical stress response.
- Reducing opioid requirement.
- Preserving natural killer (NK) cell function.
Reality check:
- Major trials show no difference in cancer outcomes between general anesthesia with or without neuraxial techniques.
3. Intravenous lidocaine
- Early retrospective data suggested improved survival.
- However, a recent RCT in pancreatic cancer patients found neutral effects on recurrence and survival.
- Peritumoral infiltration during breast cancer surgery shows promising results with reduced local recurrence and improved survival.
Other perioperative agents studied
Nonsteroidal anti-inflammatory drugs (NSAIDs)
- Epidemiologic studies suggest a potential benefit, especially for colorectal and breast cancers.
- RCTs using long-term celecoxib showed no survival benefit.
- Routine perioperative NSAID use is not currently recommended for oncologic benefit.
Opioids
- Opioids may have immunosuppressive or pro-tumor effects.
- Gene expression differences in tumors may modulate these effects.
- Current evidence advises using opioids based on analgesic needs, not oncologic concerns.
Ketamine, dexamethasone, alpha-2 agonists, acetaminophen
- Data are inconclusive or mixed.
- These drugs should continue to be used based on standard clinical indications.
Future directions
- Epigenetics and tumor genomics may unlock personalized anesthetic strategies.
- Larger, multicenter RCTs, especially outside of breast and colorectal cancer, are needed.
- Ongoing trials like GA-CARES and CAN-Colorectal may provide definitive guidance.
Conclusion
Despite initial hopes, no anesthetic or analgesic technique (except possibly peritumoral lidocaine in breast cancer) has shown a definitive benefit on long-term cancer outcomes. Anesthesia decisions should currently focus on patient safety, comfort, and quality of recovery, not on unproven oncologic effects.
As research continues, the dream of personalized onco-anesthesia tailored to a patient’s genetic profile edges closer to reality.
Reference: Ramly MS et al. Anesthetic Techniques and Cancer Outcomes: What Is the Current Evidence?. Anesth Analg. April; 140:p 768-777.
For more information on this topic, check out Anesthesia Updates on the NYSORA Anesthesia Assistant App.
Get access to step-by-step management algorithms, the latest research, and peer-reviewed insights—all in one place. Download the app today and experience the future of anesthesia education and decision-making.