Diabetes mellitus (DM) in pregnancy has become an increasingly significant challenge in modern obstetric care. Once considered a relatively rare complication, it is now one of the most common medical conditions encountered during pregnancy. According to recent data, 5–9% of all pregnancies are affected by clinically relevant diabetes, with even higher rates observed in certain ethnic groups. This rise is driven by multiple converging factors, including a global surge in obesity, an increase in maternal age, sedentary lifestyles, and a higher prevalence of preexisting type 1 and type 2 diabetes in women of reproductive age.
From an anesthesiology perspective, the implications are profound. Pregnancy itself introduces unique physiologic changes, such as increased insulin resistance and altered carbohydrate metabolism, that demand careful glucose management during labor, delivery, and the perioperative period. The stakes are high: maternal hyperglycemia has a direct effect on the fetus, and both under- and over-treatment carry risks for mother and child. Anesthesiologists must therefore integrate detailed knowledge of diabetes physiology, monitoring technologies, insulin therapy, and potential complications into their peripartum care plans.
This in-depth review synthesizes current evidence and clinical recommendations on the management of diabetes in pregnancy, with a particular focus on the anesthesia provider’s role. We will explore the physiologic underpinnings, diagnostic classification, ambulatory and inpatient management strategies, technology integration, insulin dosing adjustments, and the recognition and treatment of high-risk complications such as diabetic ketoacidosis (DKA). By the end, we aim to provide a comprehensive framework for anesthesiologists navigating this increasingly common comorbidity.
Physiological changes in pregnancy relevant to diabetes
Pregnancy is a state of progressive insulin resistance, particularly pronounced in the second and third trimesters. This is largely due to placental hormones, notably human placental lactogen, but also estrogen, progesterone, cortisol, and prolactin, which act to increase maternal lipolysis and decrease peripheral glucose utilization. This adaptation ensures that glucose is preferentially shunted to the developing fetus.
Key physiologic implications:
- Glucose transfer – Passes freely across the placenta by simple diffusion and facilitated transport.
- Insulin transfer – Does not cross the placenta; the fetus relies entirely on its pancreatic insulin production.
- Fetal hyperglycemia – Directly proportional to maternal glucose levels; stimulates fetal insulin secretion beginning in the late first trimester.
- Labor metabolism – Labor is an intense metabolic event, increasing maternal glucose utilization and hepatic glucose production.
- Postpartum reset – In gestational diabetes mellitus (GDM), insulin resistance resolves rapidly after delivery; however, long-term type 2 diabetes risk remains elevated.
Classification of diabetes in pregnancy
Correct classification informs treatment strategy and prognosis.
Preexisting diabetes
- Type 1 diabetes mellitus (T1DM)
- Autoimmune β-cell destruction.
- Absolute insulin deficiency—insulin therapy is mandatory.
- Includes latent autoimmune diabetes of adulthood.
- Type 2 diabetes mellitus (T2DM)
- Progressive β-cell dysfunction combined with insulin resistance.
- Often linked to obesity and metabolic syndrome.
- May be managed with lifestyle changes, oral agents, or insulin.
Gestational diabetes mellitus (GDM)
- GDM A1 – Diagnosed in second/third trimester, managed with diet and exercise alone (~85% of cases).
- GDM A2 – Requires pharmacologic therapy (usually insulin) (~15% of cases).
Screening and diagnosis
Universal screening
- Recommended by ACOG, USPSTF, and others at 24–28 weeks for women without known preexisting diabetes.
Early screening
- ADA suggests screening before 15 weeks for high-risk groups (obesity, PCOS, high-risk ethnicities).
- Early pregnancy diagnostic thresholds mirror nonpregnant criteria:
- HbA1c ≥ 6.5%
- Fasting plasma glucose ≥ 126 mg/dl
- 2-hour OGTT ≥ 200 mg/dl
Note: HbA1c values drop during pregnancy due to increased red blood cell turnover, reducing reliability after 15 weeks.
Ambulatory management
Glucose targets
Pregnancy demands stricter glucose control than in nonpregnant adults:
- Fasting: < 95 mg/dl
- 1-hour postprandial: < 140 mg/dl
- 2-hour postprandial: < 120 mg/dl
Why stricter targets?
For nonpregnant adults, glucose control aims to prevent long-term vascular complications; in pregnancy, the primary goal is to reduce immediate fetal risks such as macrosomia, stillbirth, and neonatal hypoglycemia.
Monitoring strategies
Self-monitoring of blood glucose (SMBG)
- Standard approach: fasting + 1 or 2 hours post-meal.
- Higher adherence is linked to better perinatal outcomes.
Continuous glucose monitoring (CGM)
- T1DM: Recommended by ADA and UK NICE guidelines.
- T2DM & GDM: Data emerging; routine use not yet standard.
- Advantages: Better detection of glycemic trends, reduced risk of unrecognized hypo-/hyperglycemia.
- Limitations: Possible inaccuracy during compression, temperature extremes, or interference (e.g., acetaminophen).
Hybrid closed-loop (HCL) systems
- Combine CGM, an automated insulin pump, and a control algorithm.
- Reduce patient burden but still require manual bolusing for meals.
- Demonstrated improved glycemic control in pregnant women with T1DM.
Insulin therapy in pregnancy
First-line therapy
- Insulin is preferred for T1DM, insulin-requiring T2DM, and GDM A2.
- Not recommended: Metformin, glyburide, GLP-1 receptor agonists—due to fetal risks.
Regimens
- Basal insulin: NPH, glargine (once or twice daily).
- Bolus insulin: Lispro or aspart before meals.
- Adjustments are made frequently to meet tighter glucose targets.
Timing of delivery
Due to the stillbirth risk associated with poor glucose control:
- T1DM/T2DM on insulin: Delivery at 39 weeks or earlier if complications arise.
- GDM A2: 37–39 weeks, depending on control.
- Poor control may prompt consideration of late preterm delivery.
Inpatient and intrapartum care
Intrapartum glucose target
- 70–110 mg/dl during active labor (ACOG recommendation).
Insulin management
- Often achieved with IV insulin infusion protocols, supplemented with dextrose-containing fluids as needed.
- Transition from subcutaneous to IV insulin when entering active labor is common.
CGM during labor
- Not FDA-approved for inpatient use, but increasingly encountered.
- Anesthesiologists must account for:
- Sensor placement (avoid compression during positioning).
- Potential device interference in the OR.
- Data verification with fingerstick testing during rapid glucose changes.
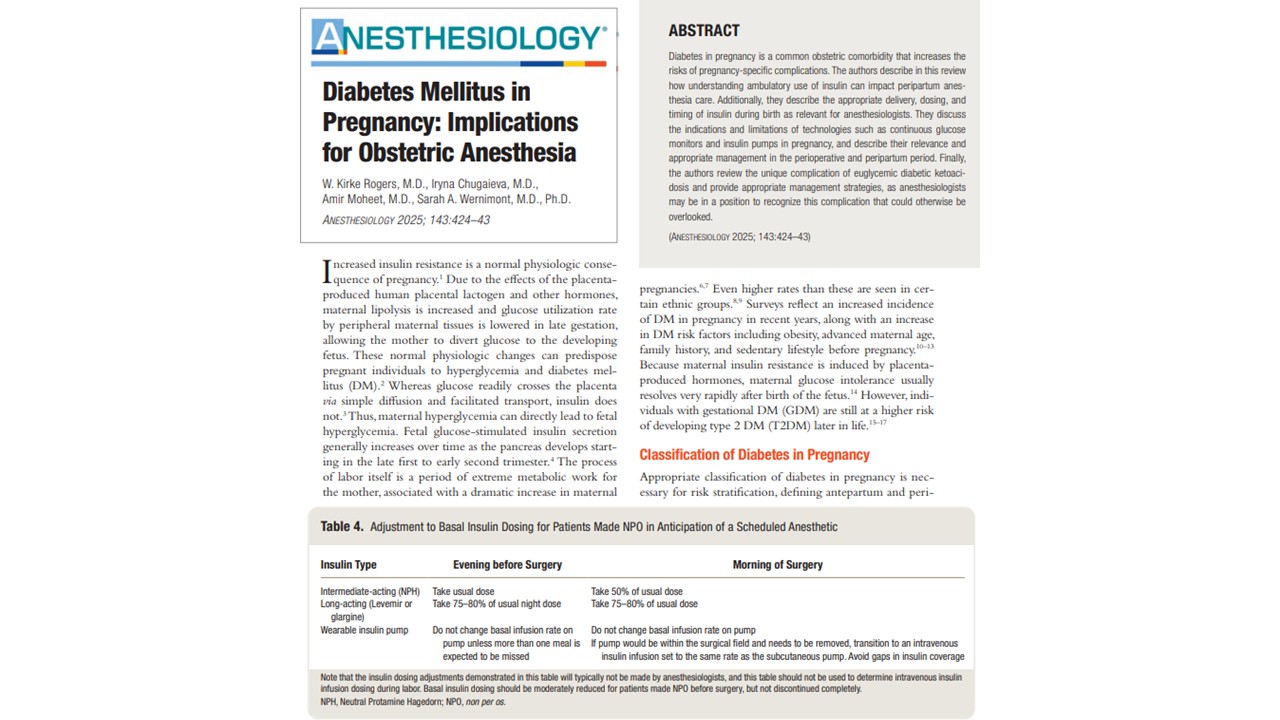
Perioperative insulin adjustments
Before scheduled cesarean:
- Reduce basal insulin dose by 25–50% depending on formulation.
- For insulin pumps: reduce basal rate by ~25%.
- Avoid insulin gaps in T1DM patients to prevent ketoacidosis.
Hypoglycemia management
Treat if BG ≤ 70 mg/dl or symptoms are present:
- If able to take PO: 15 g carbs → recheck in 15 min (“15-15 rule”).
- If NPO: 25 ml IV D50 or IM glucagon if no IV access.
Anesthetic considerations
- Choice: Neuraxial or general—both acceptable, guided by obstetric and medical considerations.
- IV access: Two lines recommended—one dedicated to insulin/high-risk infusions.
- Dexamethasone: Delay until after delivery to reduce neonatal hypoglycemia risk.
- Aspirin prophylaxis: Often continued through delivery for preeclampsia prevention.
Diabetic ketoacidosis (DKA) in pregnancy
- It can occur at lower glucose levels (euglycemic DKA).
- This condition is more common in T1DM but also seen in T2DM and GDM.
- Diagnosis: Anion gap > 12 + positive ketones, regardless of glucose.
- Management:
- Aggressive fluids (6–10 L over 24–36 h).
- IV insulin infusion (0.1 U/kg/h) with or without bolus.
- Early potassium replacement if < 5.3 mEq/l.
- Add 5% dextrose when glucose < 200 mg/dl.
- Continuous fetal monitoring.
Conclusion
The landscape of obstetric anesthesia is shifting as diabetes in pregnancy becomes more prevalent. For anesthesiologists, this means not only understanding the metabolic physiology of pregnancy but also mastering the integration of modern glucose monitoring tools, insulin delivery technologies, and nuanced perioperative protocols.
While IV insulin infusions remain the gold standard for intrapartum management, the increasing use of continuous glucose monitors and hybrid closed-loop systems raises important questions about how these devices might be incorporated into hospital protocols. Moreover, heightened vigilance is essential for recognizing complications like euglycemic DKA, which can be easily missed without a high index of suspicion.
Ultimately, optimal care requires a multidisciplinary approach, meticulous monitoring, and a readiness to adapt protocols as new evidence and technologies emerge. The anesthesiologist’s role is not just to provide anesthesia but to ensure metabolic stability, protect maternal and fetal well-being, and coordinate seamlessly with obstetric and endocrinology teams.
For more information, refer to the full article in Anesthesiology.
Rogers WK, Chugaieva I, Moheet A, Wernimont SA. Diabetes Mellitus in Pregnancy: Implications for Obstetric Anesthesia. Anesthesiology. 2025 Aug 1;143(2):424-443.
Read more about diabetes mellitus in our Anesthesiology Manual: Best Practices & Case Management.