Central arterial lines are indispensable in pediatric cardiac surgery, ensuring real-time hemodynamic monitoring, arterial blood sampling, and effective perioperative management. While the femoral artery has traditionally been the preferred access point, growing clinical concern over its associated complications has driven interest in alternative sites — most notably, the axillary artery.
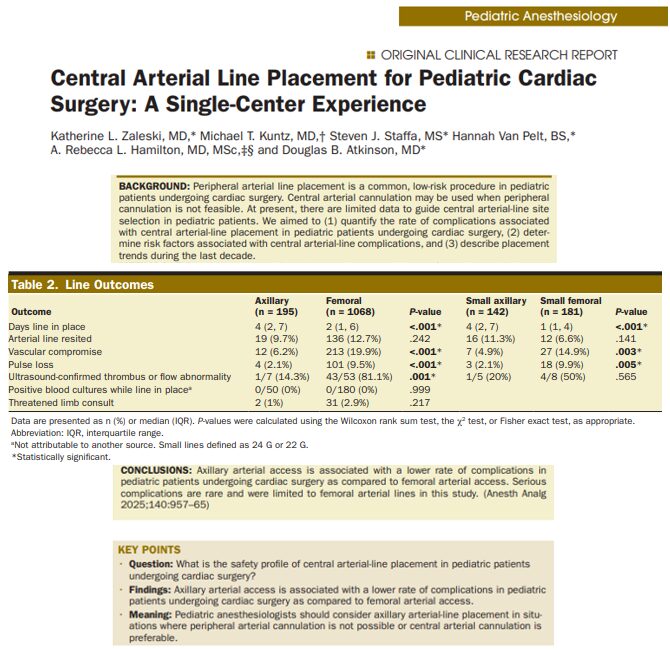
A recent single-center, retrospective study by Zaleski et al. (2025), published in Anesthesia & Analgesia, provides the most comprehensive dataset to date on this topic. Analyzing 1,263 arterial line placements at Boston Children’s Hospital over a decade, the study compares axillary and femoral approaches regarding safety, complication rates, and procedural trends. The results are eye-opening—and may be practice-changing
Why central arterial access matters in pediatric cardiac surgery
In the delicate landscape of pediatric cardiac surgery, central arterial lines serve as vital conduits for:
- Continuous blood pressure monitoring
- Arterial blood gas sampling
- Hemodynamic assessment
- Timely detection of intraoperative events
However, the choice of arterial access site can profoundly influence the risk of complications, particularly in neonates, infants, and children with comorbidities such as genetic syndromes or prematurity.
Study design
- Setting: Boston Children’s Hospital
- Duration: July 2012 – June 2022
- Patients: 1,135 pediatric cardiac surgery patients
- Lines Analyzed: 1,263 (195 axillary, 1,068 femoral)
- Primary Outcome: Complication rate (vascular compromise, pulse loss, thrombus, infection)
- Secondary Outcomes: Risk factors for complications, line placement trends
Key findings
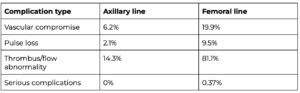
Complication rates
Why arterial site choice matters: Anatomical and physiological considerations
Axillary artery:
- Robust collateral circulation via the subclavian and scapular arteries
- Less prone to ischemia, even in the event of temporary obstruction
- Avoids the groin, reducing infection risk in diapered or immobile patients
Femoral artery:
- High risk of thrombotic events, especially in small vessels of neonates
- Limited collateral circulation increases the potential for ischemic damage
- Proximity to the groin increases infection risk in some pediatric patients
Independent risk factors for complications
For vascular compromise:
-
- Femoral location (OR 4.16)
- Genetic syndromes (OR 1.68)
- Prematurity (OR 1.48)
- Longer anesthesia time (OR 1.17/hour)
- Larger catheter size (≥2.5 Fr)
For pulse loss:
-
- Femoral location (OR 7.43)
- Genetic syndromes (OR 1.86)
- Prematurity (OR 1.65)
- 22 G catheter size (OR 3.26)
Protective factor:
-
- Larger patient size (higher weight in kg)
Shifting trends over time
Perhaps one of the most revealing aspects of the study is how clinical practice has evolved in response to these findings.
Axillary line use over time:
- 2012: 0% of arterial lines placed axillary
- 2022: 50% of arterial lines placed axillary
This reflects a paradigm shift in institutional confidence regarding axillary placement as a safer alternative to femoral access.
Step-by-step: Axillary line placement best practices
Given the emerging preference for axillary access, it’s essential to standardize safe and effective techniques:
-
Assess need
- Determine whether peripheral arterial access is not feasible
- Prioritize central access in hemodynamically unstable patients or those undergoing complex surgeries
-
Select appropriate patients
- Evaluate for genetic syndromes, prematurity, and low weight
- Axillary lines may be preferable in high-risk patients
-
Use ultrasound guidance
- Significantly improves accuracy
- Reduces accidental puncture, hematoma, and misplacement
-
Choose the right catheter size
- Use 24G or smaller catheters when possible
- Avoid large-bore catheters in neonates and low-weight infants
-
Optimal placement site
- Insert in the second segment of the axillary artery
- This region minimizes risk to adjacent neurovascular structures
-
Post-insertion monitoring
- Perform hourly neurovascular checks
- Monitor for distal perfusion, capillary refill, and limb movement
Clinical implications
This study provides robust data supporting axillary arterial access as a safer alternative to femoral placement in pediatric cardiac surgery. The findings are especially relevant for:
- Anesthesiologists performing intraoperative monitoring
- Pediatric cardiac surgeons selecting arterial access strategies
- ICU teams managing postoperative care
- Clinical policymakers shaping institutional guidelines
Conclusion
Zaleski et al.’s study delivers compelling evidence that axillary arterial lines are safer than femoral lines in pediatric cardiac surgery, with lower risks of thrombus, pulse loss, and vascular compromise.
Key takeaways:
- Femoral access carries a higher risk, particularly in premature or syndromic patients
- Axillary access offers better outcomes, especially when performed with ultrasound
- Institutional trends are shifting, reflecting a change in clinical confidence
- Clinicians should re-evaluate access strategies for each patient
This research supports an evidence-based movement toward axillary access as a first-line strategy, particularly in centers with high pediatric surgical volumes and experienced teams.
For more information, refer to the full article in Anesthesia & Analgesia.
Zaleski KL et al. Central Arterial Line Placement for Pediatric Cardiac Surgery: A Single-Center Experience. Anesth Analg. 2025;140:957-965.
For more literature highlights like this, Pediatric Anesthesia Updates 2025 is the resource to stay up-to-date in pediatric anesthesia!