Case presentation
A 56-year-old woman presented six weeks postoperatively from a surgical repair of a flexor digitorum profundus (FDP) laceration. She demonstrated an active flexion dysfunction of the fifth digit. Given the necessity for intraoperative patient cooperation to gauge the surgery’s functional outcome, general anesthesia was ruled out.
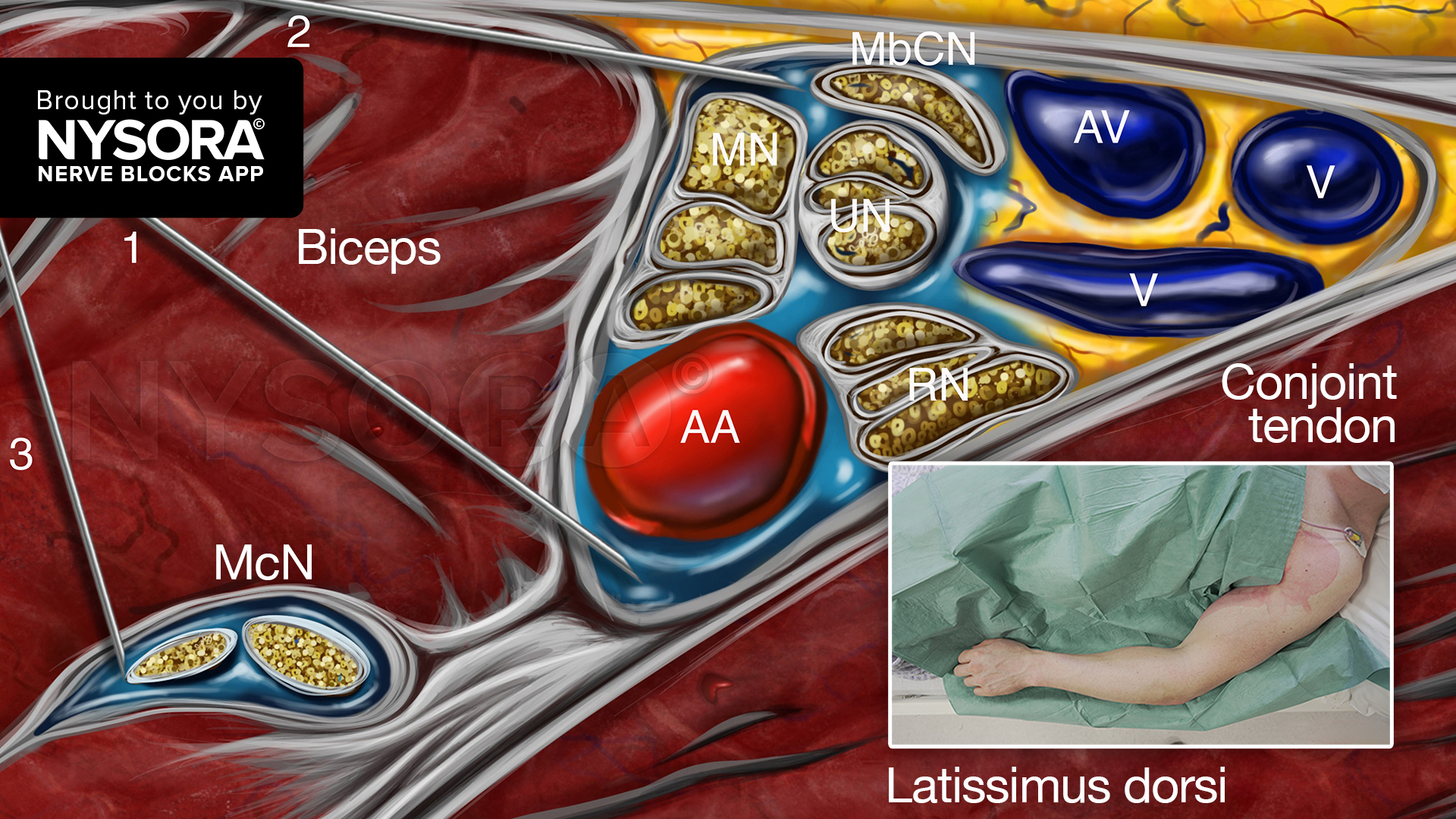
Nerve block techniques
Median and ulnar nerve blocks at the wrist
- Rationale: Blocking the median and ulnar nerves just proximal to the wrist crease allows for anesthesia of the fifth digit without compromising the motor function of the hand flexors. This approach ensures complete anesthesia for the surgical intervention while preserving the ability to test finger flexion actively.
- Technique: Under ultrasound guidance, the median and ulnar nerves were identified between the superficial and deep flexors of the wrist and fingers. Next, a 25-gauge needle was inserted in-plane or out-of-plane to inject 5 mL of lidocaine 2% into the fascia containing the nerves. The onset of anesthesia was observed within 10 minutes.
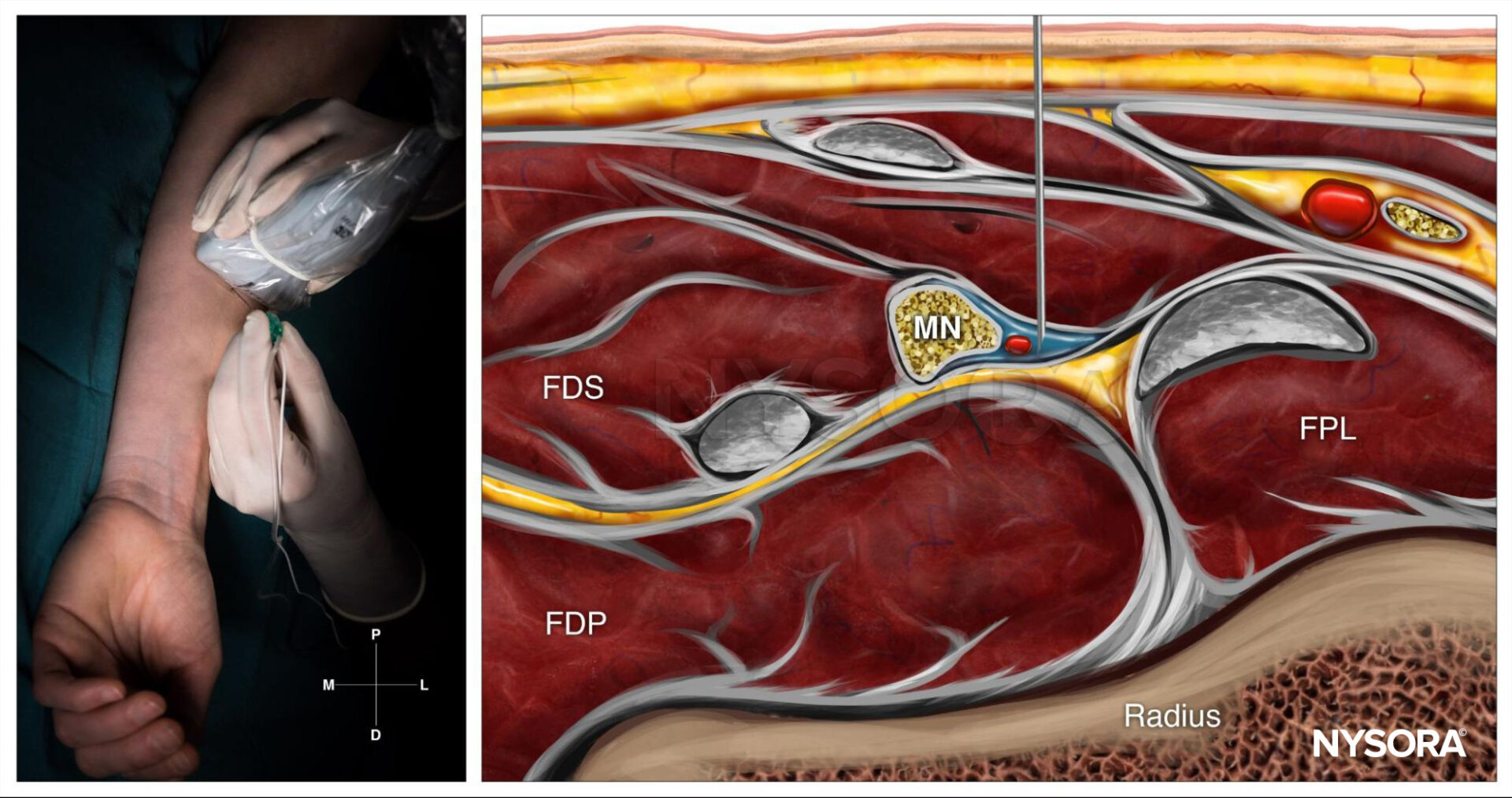
Median nerve block at the level of the wrist; Reverse Ultrasound Anatomy with needle insertion out-of-plane and local anesthetic spread (blue). MN, median nerve; FPL, flexor pollicis longus muscle; FDS, flexor digitorum superficialis muscle; FDP, flexor digitorum profundus muscle.
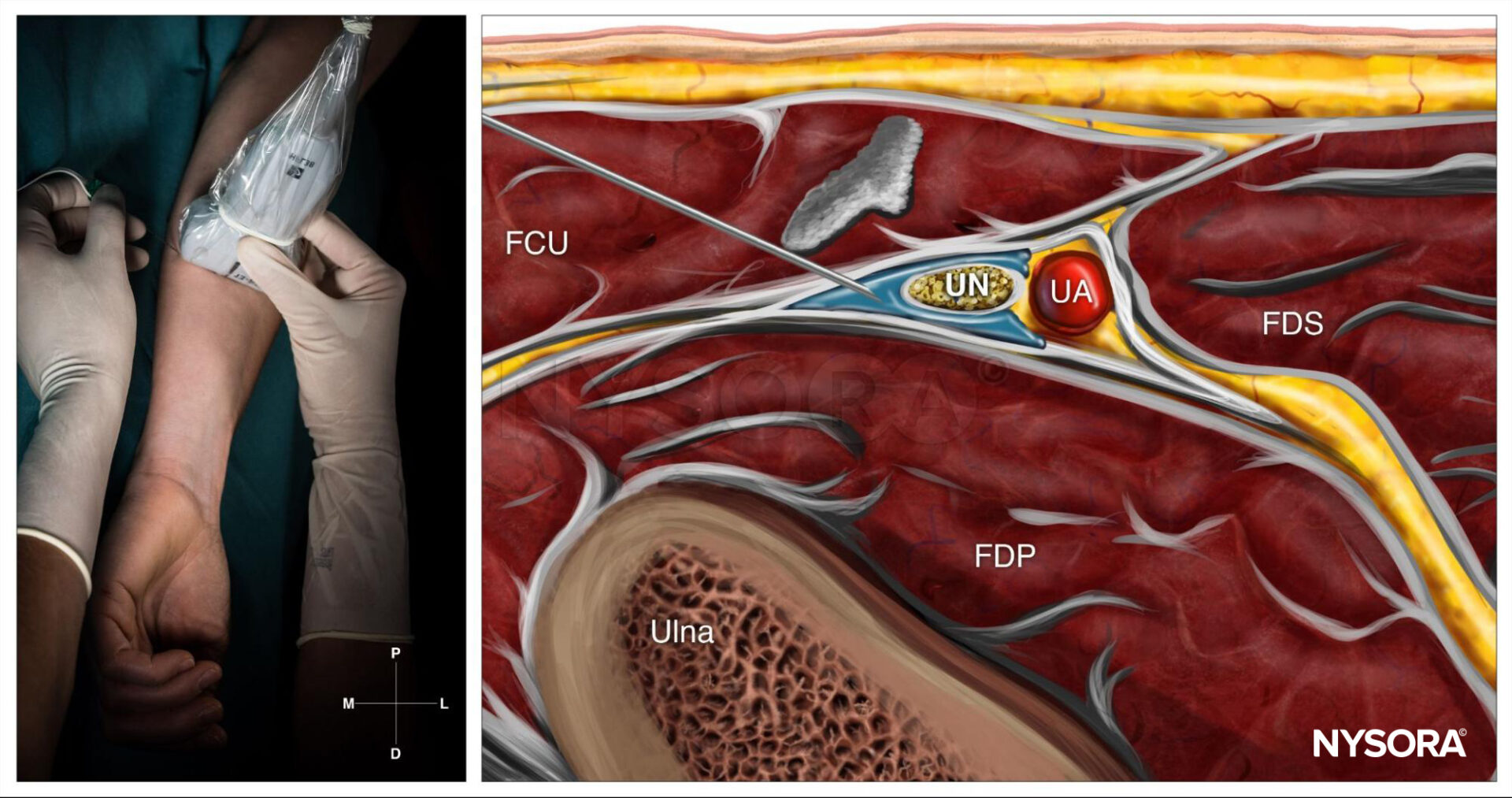
Ulnar nerve block at the level of the wrist; Reverse Ultrasound Anatomy with needle insertion in-plane and local anesthetic spread (blue). UN, ulnar nerve; UA, ulnar artery; FCU, flexor carpi ulnaris; FDP, flexor digitorum profundus muscle; FDS, flexor digitorum superficialis muscle.
Patient outcome
Throughout the surgical procedure, the patient was comfortable and pain-free, confirming the nerve blocks’ effectiveness. The patient could actively open and close her hand upon the surgeon’s request, allowing real-time assessment of the fifth digit’s flexor tendon. Although the tendon release initially seemed successful, further intraoperative testing revealed residual adhesions. The surgeon then undertook additional cleaning of the flexor tendon, achieving a complete restoration of hand function.
Comparative analysis of circumferential and non-circumferential nerve block techniques
The study by Dieguez-Garcia et al. 2020 sheds light on two prominent approaches to local anesthesia administration. This groundbreaking research investigates whether circumferential (C) or non-circumferential (NC) spread of local anesthetic produces superior sensory and motor block outcomes in the median and ulnar nerves.
Background
Local anesthetic (LA) spread patterns are crucial in nerve block efficacy. Circumferential spread involves the homogeneous distribution of LA around the nerve, a method traditionally associated with quicker and more effective block onset. However, the technique demands precision, increasing the risk of inadvertent trauma to surrounding nerves and blood vessels. While easier to execute, the non-circumferential spread may compromise the block’s effectiveness.
Study objectives and methodology
The goal was to evaluate the proportion of patients achieving complete sensory block at 5, 15, and 30 minutes post-injection intervals. Secondary outcomes included motor block efficacy, nerve swelling incidence, and adverse event rates.
Key aspects of the study design included:
- Participants: 124 patients scheduled for open carpal tunnel syndrome surgery.
- Randomization: Patients were assigned a C or NC spread of 6 mL of 1% mepivacaine.
- Assessment tools: Standardized cold sensation and motor function tests assessed sensory and motor blocks.
- Blinding: Both patients and outcome assessors were blinded to the group allocation.
Results
Primary outcome: sensory block
- At 5 minutes post-injection, a complete sensory block was achieved significantly more often in the C group:
- Median nerve: Relative Risk (RR) 2.4 (p=0.04).
- Ulnar nerve: RR 3.0 (p=0.01).
- By 15 and 30 minutes, block success rates were comparable between the C and NC groups, nearing 100% effectiveness.
Secondary outcomes: motor block and nerve swelling
- The C group demonstrated higher rates of complete motor block at 15 and 30 minutes:
- Median nerve: RR 1.5 (p<0.01) at 15 minutes; RR 1.1 (p=0.02) at 30 minutes.
- Ulnar nerve: RR 1.7 (p<0.01) at 15 minutes; RR 1.2 (p<0.01) at 30 minutes.
- Nerve swelling incidence was approximately 26% across both groups and nerves, with no significant difference between the C and NC approaches.
Adverse events
No nerve damage or severe complications were reported. Only one patient experienced a mild hematoma, which required no further treatment.
Implications for clinical practice
The findings suggest that circumferential spread provides a rapid onset of complete sensory and motor block within 15 minutes, making it particularly advantageous in time-sensitive surgical settings. However, non-circumferential spread achieves comparable results at 30 minutes, offering a safer and simpler alternative when immediate block onset is not critical.
Recommendations
- Circumferential spread: Reserved for scenarios demanding rapid onset of anesthesia, particularly when performed by experienced practitioners to minimize complications.
- Non-circumferential spread: Preferred for routine procedures, providing effective results with lower technical demands.
Study limitations and future directions
While the study highlighted the efficacy of C spread, certain limitations must be acknowledged:
- A higher volume (6 mL) of anesthetic was used, which may not reflect typical clinical practices where smaller doses are employed.
- Long-term effects were self-reported and not validated by follow-up examinations, possibly underestimating adverse outcomes.
- Results were specific to using a 20° bevel needle; variations in needle design could alter findings.
Future research should explore the impact of lower anesthetic volumes, alternative needle designs, and long-term outcomes assessed via comprehensive neurological evaluations.
Conclusion
The comparative analysis underscores the nuanced advantages of circumferential versus non-circumferential techniques. Both methods achieve high success rates for median and ulnar nerve blocks, with circumferential spread offering a slight edge in rapidity and completeness under specific conditions. Tailoring the choice of technique to clinical scenarios and practitioner expertise ensures optimal outcomes for patients undergoing regional anesthesia.
For more information, refer to the full article in Regional Anesthesia & Pain Medicine.
Dieguez-Garcia P, Lopez-Alvarez S, Juncal J, Lopez AM, Sala-Blanch X. Comparison of the effectiveness of circumferential versus non-circumferential spread in median and ulnar nerve blocks. A double-blind randomized clinical trial. Reg Anesth Pain Med. 2020 May;45(5):362-366.
For more case studies like these and the complete guide to the 60 most frequently used nerve blocks, download the Nerve Blocks App HERE. Don’t miss the chance to get the bestselling NYSORA Nerve Blocks App also in book format – the perfect study companion with the Nerve Blocks app!