Learning objectives
- Describe the indications for esophagectomy
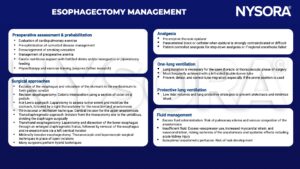
- Manage patients presenting for esophagectomy
Background
- Esophageal cancer is the eighth most common malignancy worldwide
- Curative therapy for many patients involves surgery (esophagectomy), often with preoperative chemotherapy
- Esophagectomy remains high-risk with substantial associated morbidity and mortality
Risk factors for esophageal malignancy
| Risk factor | Adenocarcinoma | Squamous cell carcinoma |
|---|---|---|
| Lifestyle | Smoking | Alcohol, smoking (may show synergism), poor oral hygiene |
| Racial origin | Caucasian more common than Asian or African | Sub-Saharan African Heritage three times higher than Caucasians |
| Far East Asian Heritage | ||
| Age and gender | Increasing age, male greater than female | Male greater than female |
| Dietary | Low dietary intake of fruit and vegetables | Salted vegetables, preserved fish |
| Disease | Gastro-oesophageal reflux, Barrett’s oesophagus, obesity, family history (rare) | Mutations of alcohol metabolic pathways, achalasia, caustic injury, nutritional deficiencies, non-epidermolytic palmoplantar keratoderma |
| Economic | Developed world | Low socioeconomic status |
| Developing world | ||
| Medical/industrial | Thoracic radiation, medications that relax the lower oesophageal sphincter | Thoracic radiation |
Risk factors for perioperative morbidity and mortality
- Poor cardiac and/or pulmonary function
- Advanced age
- Tumor stage
- Diabetes mellitus
- Impaired general health
- Hepatic dysfunction
- Peripheral vascular disease
- Smoker
- Chronic use of steroids
Management
Postoperative complications
| Respiratory | Pneumonia |
| Atelectasis | |
| Acute respiratory stress syndrome | |
| Recurrent laryngeal nerve palsy | |
| Surgical | Anastomotic leak |
| Cardiac | Supraventricular arrhythmias (e.g., atrial fibrillation) |
- The risk of respiratory complications can be minimized by adequate analgesia, reversal of muscular block, normothermia, chest physiotherapy and hemodynamic stability
- Major anastomotic leaks require surgical exploration and revision surgery
- Smaller leaks are managed by keeping the patient nil by mouth, giving high protein enteral feed or total parenteral nutrition, antibiotics, chest physiotherapy, radiologically guided drainage collection and performing serial contrast studies
Suggested reading
- Howells P, Bieker M, Yeung J. Oesophageal cancer and the anaesthetist. BJA Education. 2017;17(2):68-73.
- Veelo DP, Geerts BF. Anaesthesia during oesophagectomy. J Thorac Dis. 2017;9(Suppl 8):S705-S712. doi:10.21037/jtd.2017.03.153
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com