What’s new
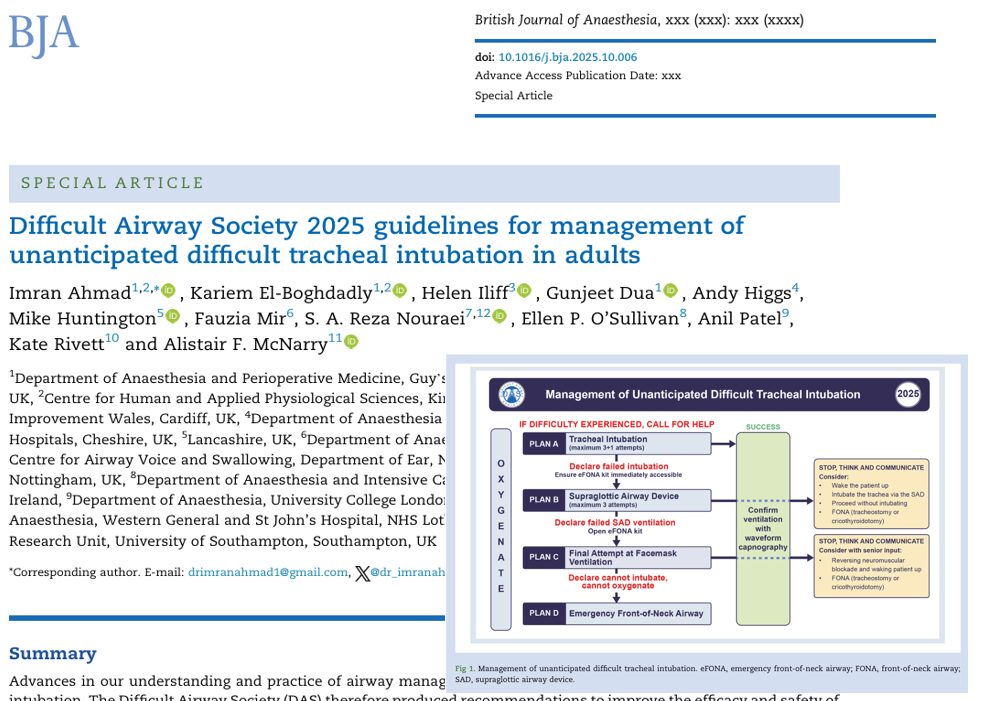
The 2025 DAS guideline, titled “Management of unanticipated difficult tracheal intubation in adults”, is a major update authored by Imran Ahmad et al. and published in the British Journal of Anaesthesia.
Key features:
- 1,241 papers reviewed via systematic review, three‑round Delphi process over 3 years.
- 65 recommendations covering major domains: assessment, peroxygenation, human factors, post‑intubation care, and more.
- Maintains the linear algorithm of Plan A → Plan B → Plan C → Plan D (intubation → supraglottic airway → facemask ventilation → emergency front‐of‐neck airway).
- Emphasises maximising success (first pass, oxygenation) rather than only managing failures.
Why this matters
- Unanticipated difficult airway situations remain a key source of perioperative morbidity and mortality; updated evidence means practice must evolve.
- Clinicians now have a modern, evidence‑based tool to guide management when intubation becomes challenging.
- The guideline synthesises technological advances (e.g., videolaryngoscopy, point‑of‑care ultrasound), human factors, and systems thinking into airway management.
Highlighted domains and key changes
1. Pre‑intubation assessment & planning
- The guideline reinforces structured airway assessment AND creates a strategy for the physiologically difficult airway (e.g., shock, severe hypoxia, obesity).
- Planning includes preparation of equipment, team roles, backup plans, and the use of cognitive aids.
2. Peroxygenation and oxygenation strategies
- Continuous oxygen delivery throughout airway management is prioritised.
- Strategies such as high‑flow nasal oxygen, non‑invasive ventilation, and head‑up ramping are given emphasis.
3. First‑pass success and device strategy
- The document emphasises maximising first‑attempt intubation success using appropriate tools and techniques.
- Universal use of videolaryngoscopy is increasingly expected, and the guideline incorporates evidence for this.
4. Using the algorithm: Plan A to D
- Plan A: Tracheal intubation.
- Plan B: Supraglottic airway device ventilation.
- Plan C: Facemask ventilation.
- Plan D: Emergency front‑of‑neck airway (eFONA).
- The guideline reinforces the importance of rapid progression through plans if failure occurs, and clear criteria for when to move to the next plan.
5. Human factors, teamwork & training
- A strong focus on non‑technical aspects: team briefing, role assignment, simulation training, and clear documentation.
- The guideline emphasises that improving success is not only about devices, but about systems and people.
6. Post‑intubation care & documentation
- After successful airway management, the guideline emphasises confirming placement (waveform capnography), monitoring ventilation and oxygenation, and documenting what happened (including a plan if further airway difficulty).
Quick‑reference summary: what should your team do?
-
Pre‑intubation preparation:
- Perform airway assessment & mark potential difficulties.
- Ensure equipment (videolaryngoscope, bougie/stylet, supraglottic devices, eFONA kit), team roles, and plan are ready.
- Preoxygenate thoroughly; consider a ramped position for obesity or physiology‑challenged patients.
- Perform airway assessment & mark potential difficulties.
-
Intubation attempt (Plan A):
- Use videolaryngoscopy as first‑line where available.
- Aim for first‑pass success.
- If unsuccessful within defined attempts/time, transition to Plan B.
- Use videolaryngoscopy as first‑line where available.
-
Plan B / Plan C:
- Insert a supraglottic airway device if intubation fails (Plan B).
- If that fails, consider facemask ventilation (Plan C) — but know when to move forward.
- Insert a supraglottic airway device if intubation fails (Plan B).
-
Plan D – eFONA:
- If you are in a “cannot intubate, cannot oxygenate” scenario, proceed with emergency front‑of‑neck airway without delay.
- Every team member must know this plan and how to execute it.
- If you are in a “cannot intubate, cannot oxygenate” scenario, proceed with emergency front‑of‑neck airway without delay.
-
Post‑intubation & handover:
- Confirm tube placement with capnography.
- Monitor oxygenation, ventilation, and hemodynamics.
- Document the airway course, what device was used, why the failure occurred (if applicable), and plan for extubation/next airway.
- Debrief with the team for learning.
- Confirm tube placement with capnography.
Implementation tips for your department
- Step 1: Disseminate the guideline among your anesthesia and airway teams (consultants, trainees, OT staff, ICU staff).
- Step 2: Review your airway equipment check‑lists: include videolaryngoscope (if available), bougie/stylet, supraglottic devices, eFONA kit, oxygenation adjuncts.
- Step 3: Update your airway algorithms and posters in operating theatres and ICU to reflect Plan A→B→C→D and the emphasis on first‑pass success.
- Step 4: Plan simulation sessions that include unanticipated difficult intubation scenarios, focus on teamwork, human factors, and transitions between plans.
- Step 5: Audit your airway events: track first‑pass success rate, number of attempts, rescue device usage, eFONA usage, complications; feed back to your team.
- Step 6: Ensure documentation templates capture the airway plan, what was used, any difficulties, how they were managed, and the extubation/handover plan.
Final thoughts
The 2025 DAS guideline marks a significant step forward in adult airway management by combining up‑to‑date evidence, a clear algorithmic structure, and a strong emphasis on maximising success rather than just managing failure. For anesthetists, intensivists, and emergency airway practitioners, this is a must‑read.
By embedding these recommendations into your department’s workflow, you can help improve patient safety, team performance, and outcomes in one of the highest‑risk moments in perioperative care.
Reference: Ahmad I et al. Difficult Airway Society 2025 guidelines for management of unanticipated difficult tracheal intubation in adults. Br J Anaesth. Published online November 7, 2025.
Read more about this topic in the Anesthesia Updates section of the Anesthesia Assistant App.