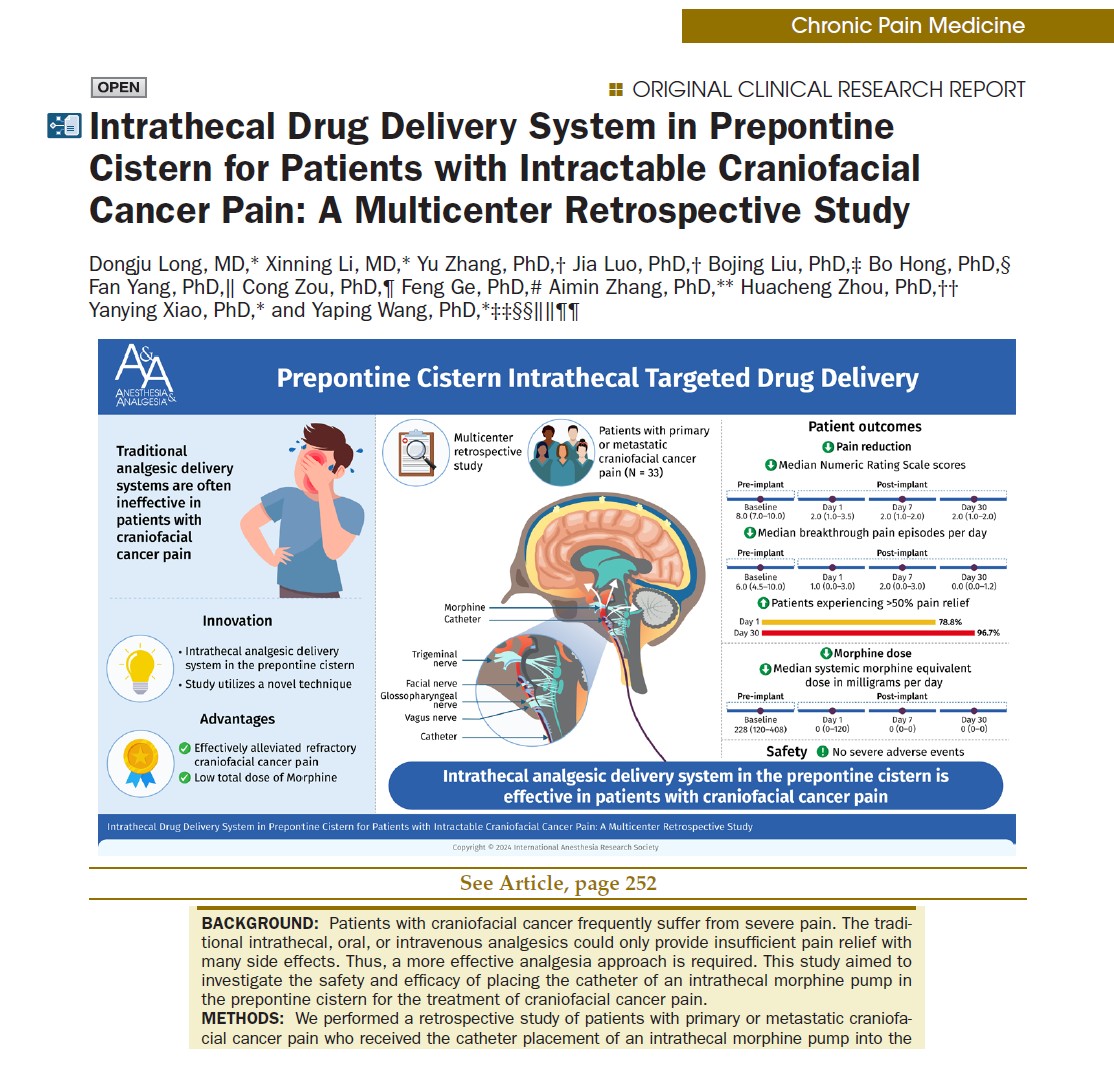
Patients with craniofacial cancer often endure debilitating and unrelenting pain. This type of pain, caused by malignancies in the head and facial regions, is frequently resistant to traditional analgesics. Oral, intravenous, or conventional intrathecal opioids often fail to provide effective relief and carry significant side effects. Now, a pioneering study by Dongju et al. has revealed a promising solution: placing an intrathecal drug delivery system (ITDD) catheter in the prepontine cistern, located near the brainstem.
Why this study matters
This multicenter retrospective study, involving 33 patients across 11 major hospitals in China, is the first large-scale investigation to assess the safety and efficacy of prepontine cistern-targeted morphine delivery for refractory craniofacial cancer pain.
The science behind the strategy
What is the prepontine cistern?
The prepontine cistern is a cerebrospinal fluid (CSF)-filled space located in front of the pons, a critical brainstem structure where multiple cranial nerves arise, including the trigeminal nerve, which transmits facial pain.
Delivering morphine into this area allows for:
- Direct targeting of cranial nerve roots
- Rapid and localized action
- Lower morphine doses for the same effect
- Reduced systemic exposure and side effects
Why not traditional intrathecal placement?
Conventional ITDD systems deliver drugs to lumbar or thoracic spinal segments, which are less effective for head and neck pain. High cervical placement or intracisternal methods have been explored but are often invasive, high-risk, or difficult to stabilize. The prepontine approach, via lumbar puncture, avoids these challenges.
Study overview
- Type: Multicenter retrospective cohort
- Duration: September 2019 – December 2023
- Participants: 33 patients (mean age 60.5 years; 60.6% male)
- Indications:
- Intractable craniofacial cancer pain
- Failure of conventional opioid therapy
- Unacceptable side effects from systemic opioids
- Catheter insertion:
-
- Via lumbar puncture
- Guided fluoroscopically to the prepontine cistern
Results: significant and sustained pain relief
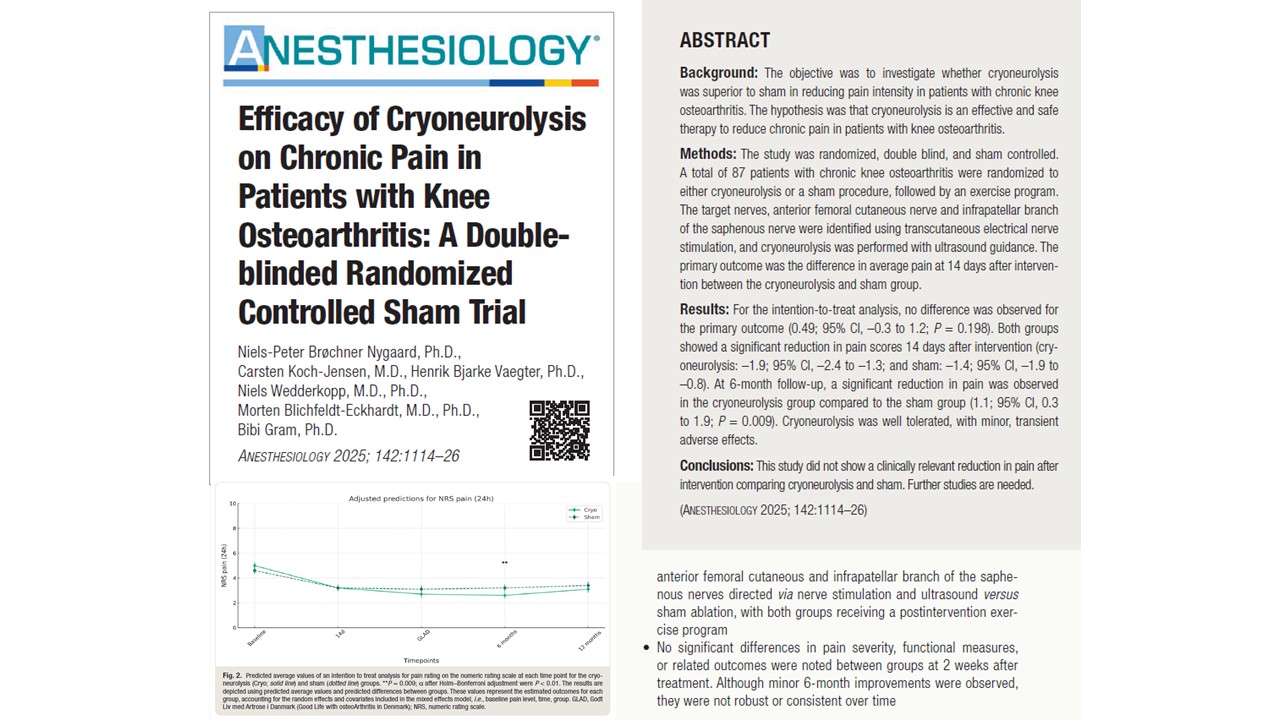
Pain intensity (NRS score)
- Preoperative median: 8.0 (on a scale of 0–10)
- Postoperative day 1: 2.0
- Postoperative day 30: 1.0
- 90% reduction in pain severity
Breakthrough pain episodes
- Pre-op: Median 6.0 episodes/day
- Post-op day 30: Median 0.0 episodes/day
- P value: < .001 (statistically significant)
Pain improvement categories
- Day 1:
- Moderate (≤50% relief): 7 patients
- Effective (50–75%): 10 patients
- Excellent (>75%): 16 patients
- Day 30:
- Moderate: 1 patient
- Effective: 9 patients
- Excellent: 20 patients
- Total achieving >50% pain relief by day 30: 96.7%
Morphine dosage optimization
Systemic morphine equivalents
- Baseline median: 228 mg/day
- Post-op day 1: 0–120 mg/day
- Day 7 and 30: 0 mg/day in most patients
Intrathecal morphine dose
- Day 1: Median 0.16 mg/day
- Day 30: Increased to 0.36 mg/day as needed
- Rationale: Gradual titration to maintain relief while minimizing respiratory depression
How the procedure works
Step-by-step surgical technique
- Preoperative imaging: MRI to confirm catheter access route
- Patient positioning: Side-lying, under local anesthesia
- Lumbar puncture: Via L2/L3 or L3/L4 using 14G Tuohy needle
- Catheter insertion:
-
- Navigated through spinal canal and foramen magnum
- Positioned at the prepontine cistern using fluoroscopy
5. Infusion port placement:
-
- Subcutaneously on the anterior axillary line
- Connected to external electronic pump
6. Drug administration:
-
- Initial morphine dose = 1/1000 of oral equivalent
- Delivered at 0.1 mL/hour continuously
- Breakthrough pain managed via bolus: 0.1 mL every 30 minutes
Safety outcomes
Adverse events
- Mild and transient:
- Hypotension (1 patient)
- Nausea, dry mouth, sedation (few patients)
- No severe complications:
- No respiratory depression
- No CNS infection or catheter dislodgement
- No neurological deficits
Comparison to older techniques
- Prepontine placement avoids:
-
- Tetraplegia risk from cervical spinal puncture
- Hemorrhage from skull drilling
- High infection risk from ventricular methods
Advantages over conventional methods

Study limitations
- Retrospective design: Limits causal inference
- Small sample size: Only 33 patients
- Short follow-up: Long-term safety data is needed
- Lack of control group: No direct comparison to other techniques
Future directions
- Randomized controlled trials to validate efficacy and safety
- Long-term studies assessing catheter durability and infection rates
- Combination therapy: Testing synergistic effects with ziconotide or bupivacaine
- Use in benign craniofacial pain conditions
Conclusion
The results of this multicenter study highlight the transformative potential of prepontine intrathecal morphine delivery. It not only provides rapid, sustained pain relief but does so with minimal drug dosage and negligible side effects. For patients with intractable craniofacial cancer pain, this method opens new therapeutic horizons.
As the field of neuromodulation evolves, targeted, anatomical drug delivery is set to revolutionize pain medicine. The prepontine cistern approach stands at the forefront of this shift, bringing relief where it’s most needed, in the most precise way.
For more detailed information, refer to the full article in Anesthesia & Analgesia.
Long D, Li X, Zhang Y, et al. Intrathecal Drug Delivery System in Prepontine Cistern for Patients with Intractable Craniofacial Cancer Pain: A Multicenter Retrospective Study. Anesthesia & Analgesia. 2025;141(2).
To get more updates on the latest impactful research in pain medicine, download NYSORA’s Pain Medicine Assistant!