The use of dexamethasone in the perioperative setting is common due to its proven benefits in reducing postoperative nausea, pain, and opioid use. However, for patients with diabetes, concerns about hyperglycemia and infection risks have led to hesitation in its application. Recent findings from a major systematic review and meta-analysis, along with new decision-making tools, provide clarity for clinicians navigating this complex issue
Why the Concern?
Dexamethasone is a corticosteroid known to cause transient hyperglycemia by increasing hepatic gluconeogenesis and decreasing peripheral glucose utilization. While this hyperglycemia is often mild and self-limiting in non-diabetic patients, it raises alarms in diabetic individuals already at risk of poor wound healing, surgical site infections (SSIs), and other complications associated with elevated glucose levels.
Historically, clinicians have had limited data to guide dexamethasone use in diabetics. Most studies either excluded diabetic patients or failed to report outcomes specific to them. This absence of evidence led to clinical conservatism, with many avoiding dexamethasone altogether in this population.
What the new evidence says
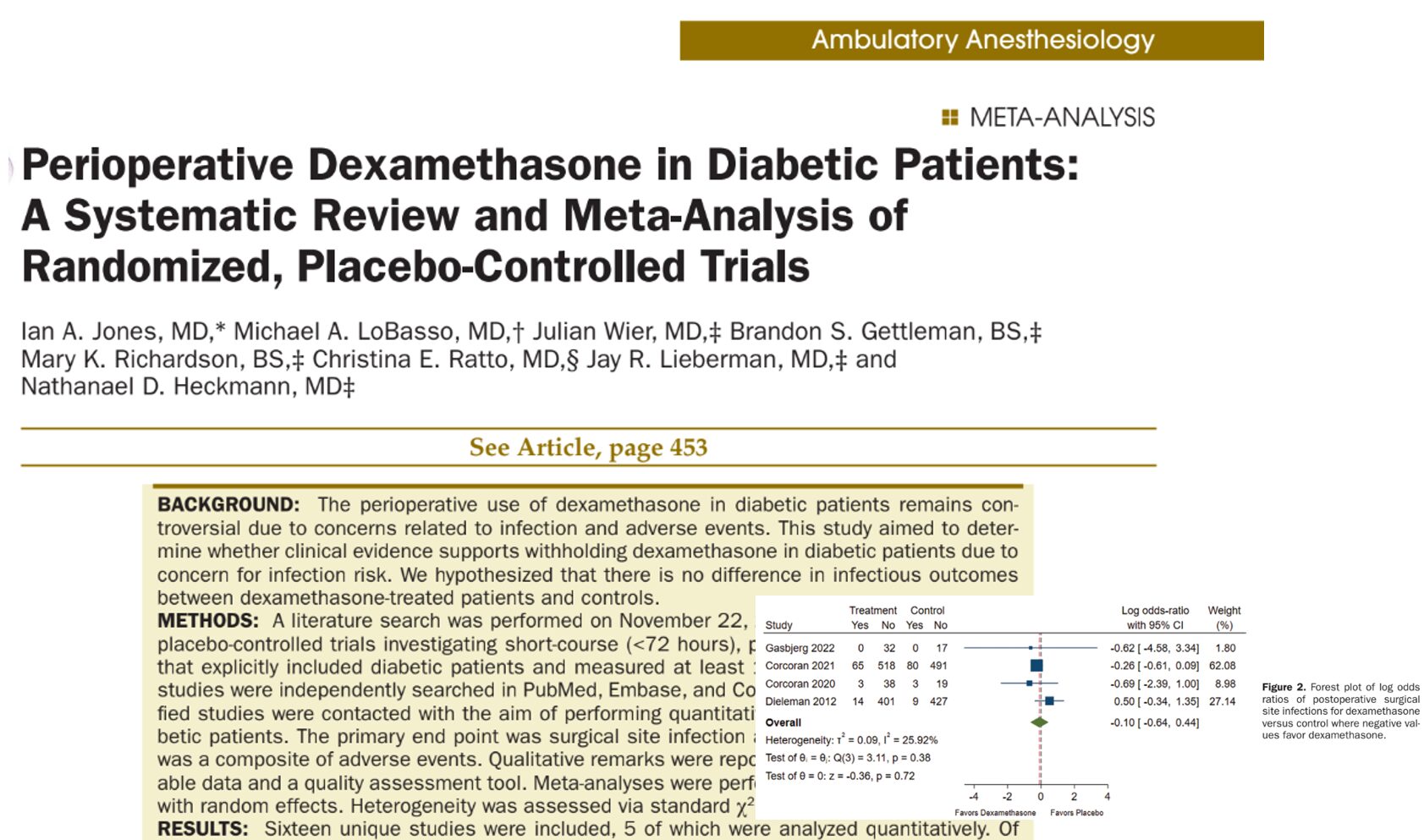
A systematic review by Jones et al. (2024) analyzed 16 randomized controlled trials, encompassing 2,592 diabetic patients, to determine if perioperative dexamethasone increases the risk of complications, particularly infections.
Key findings:
- No increased risk of surgical site infections (SSIs): The pooled analysis found no statistically significant difference in infection rates between patients who received dexamethasone and those who did not.
- Reduced risk of composite adverse events: Dexamethasone was associated with a significant reduction in overall adverse events, including respiratory complications, prolonged hospitalization, and cardiovascular issues.
- Dexamethasone improved outcomes such as:
- Reduced postoperative nausea and vomiting (PONV)
- Lower pain scores
- Shorter hospital stays
- Fewer respiratory complications
Importantly, even when accounting for variability in dosage and surgical type, the overall safety profile remained favorable.
What Does This Mean Clinically?
This meta-analysis offers strong reassurance that dexamethasone can be used safely in diabetic patients when applied with thoughtful assessment and appropriate dosing. But how should clinicians approach decision-making in real time?
To aid in this, a practical decision-making pathway has been developed to guide perioperative dexamethasone use based on a patient’s HbA1c level, current glucose control, and infection risk factors.
Dexamethasone decision-making pathway
A clinical decision algorithm has been proposed to guide perioperative dexamethasone use based on HbA1c levels and glucose control:
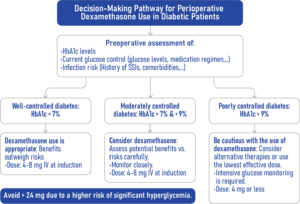
Preoperative Assessment Should Include:
- HbA1c levels
- Current glucose control: Evaluate glucose levels and medication regimen
- Infection risk: Consider history of surgical site infections (SSIs), comorbidities, etc.
Based on HbA1c and Diabetes Control Status:
-
Well-Controlled Diabetes (HbA1c < 7%)
- Dexamethasone use is appropriate — benefits outweigh risks.
- Recommended dose: 4–8 mg IV at induction.
-
Moderately Controlled Diabetes (HbA1c between 7% and 9%)
- Consider dexamethasone, assess potential benefits vs. risks carefully.
- Monitor the patient closely.
- Recommended dose: 4–8 mg IV at induction.
-
Poorly Controlled Diabetes (HbA1c > 9%)
- Be cautious with dexamethasone:
- Consider alternative therapies or use the lowest effective dose.
- Intensive glucose monitoring is required.
- Recommended dose: 4 mg IV or less.
Important Note:
Avoid dexamethasone doses greater than 24 mg due to a significantly increased risk of severe hyperglycemia.
Why Dosing Matters
One of the most important takeaways from the meta-analysis was the variability in dexamethasone dosing across studies. Some studies used doses as high as 100 mg (e.g., in cardiac surgery), while others used modest 4–8 mg doses typical for antiemetic prophylaxis. Despite this variability, no increased infection risk was identified, suggesting that even higher doses may be acceptable in select cases.
That said, the risk of hyperglycemia is dose-dependent. In poorly controlled diabetes, clinicians should err on the side of caution by:
- Opting for lower doses
- Monitoring blood glucose intensively
- Considering alternative antiemetics or analgesics
For additional strategies on managing hyperglycemia during the perioperative period, including in ambulatory settings, check out this news post.
Key clinical recommendations
For anesthesiologists and surgical teams:
- Dexamethasone can be safely integrated into perioperative protocols for diabetic patients with HbA1c < 9%.
- Use lower doses and closer monitoring for patients with poor glycemic control.
- Consider patient comorbidities and surgical infection risk before administration.
- Continue to monitor ongoing research for guidance on optimal dosing in uncontrolled diabetes.
Benefits Beyond PONV
Dexamethasone’s reputation as an antiemetic is well-earned, but this study highlights its broader utility. In diabetic patients, the following additional benefits were noted:
- Reduced pain intensity
- Decreased opioid requirements
- Shortened ICU and hospital stays
- Reduced respiratory complications (e.g., need for mechanical ventilation)
- Potential reduction in major adverse cardiac events (in cardiac surgery patients)
These findings suggest that perioperative dexamethasone has a role in enhancing recovery and minimizing complications, even in higher-risk populations.
Conclusion
For too long, perioperative dexamethasone use in diabetic patients has been hampered by theoretical concerns that are not well supported by clinical evidence. The systematic review by Jones et al. makes a strong case for change.
Dexamethasone, when appropriately dosed and monitored, can be a safe and beneficial adjunct for diabetic patients undergoing surgery. Rather than a blanket avoidance, a personalized, evidence-based approach should be adopted, tailored to the individual patient’s glycemic control and perioperative risk.
As the landscape of perioperative care continues to evolve, so should our practice patterns. Dexamethasone remains a valuable tool, not to be feared, but to be used wisely.
For more detailed information, refer to the full article in A&A.
Jones IA. et al. Perioperative Dexamethasone in Diabetic Patients, Anesth Analg. 2024;139:479-489.
Read more about this topic in the Anesthesia Updates section of the Anesthesia Assistant app. Prefer a physical copy? Get the latest literature and guidelines in book format. For an interactive digital experience, check out the Anesthesia Updates Module on NYSORA360!